Introduction
As is universally known, radiation therapy can cause
numerous side-effects in clinical practice, including side
reactions of the respiratory, cerebrovascular and gastrointestinal
systems, and so forth. However, carotid artery dissection induced
by radiotherapy is infrequent. The present case study reports on
the clinical and neuroimaging characteristics of one patient with
cerebral infarction caused by radiotherapy.
Case report
A 66-year-old man was admitted to the emergency
department of our hospital (Shanghai Ninth People's Hospital,
Shanghai, China) presenting with sudden mild left hemiplegia,
hemianesthesia, nausea and vomiting. The patient had a medical
history of nasopharyngeal carcinoma treated with radiotherapy
combined with chemotherapy 10 years previously, and right basal
ganglia hemorrhage 1 year prior to his admission. Initially, a
computerized axial tomography (PHILIPS Brilliance 64 CT scanner;
Philips Healthcare, DA Best, The Netherlands) was performed which
revealed no evidence of any high-density lesion (Fig. 1). Intravenous thrombolysis treatment
was not administered due to a previous cerebral hemorrhage,
although the patient remained within the time window. As the
patient's left hemiplegia had deteriorated with the onset of left
central facial paralysis, he was transferred to the intensive care
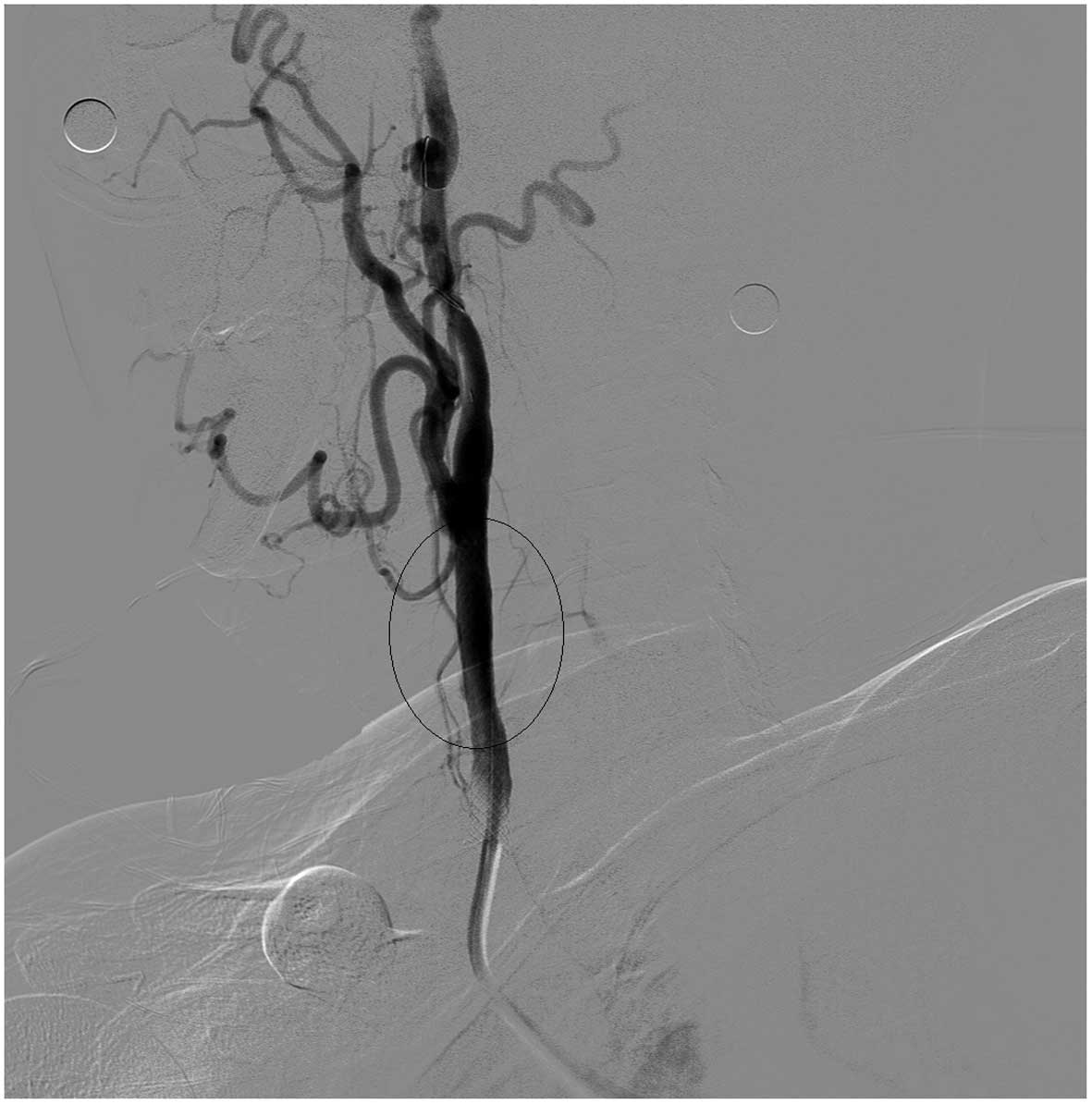
unit for monitoring and medical management. A cerebral angiography
was performed, with evidence of right common carotid artery
dissection and stenosis (Fig. 2).
Subsequently, 5,000 U heparin was injected into the patient's body
intravenously. With respect to the guide wire and other materials,
an 8F guided tube was placed in the right common carotid artery,
and the protective device was placed at the distal end of the
internal carotid artery. A 9×50 mm WALLSTENT™ stent (Boston
Scientific Corporation, Natick, MA, USA) was then imported and
released after having been accurately located. Cerebral angiography
was subsequently performed, which demonstrated that the dissection
and stenosis were markedly improved (Fig.
3). Aspirin (100 mg per day) and clopidogrel (75 mg per day for
1 year) for anti-platelet aggregation, and Lipitor (atorvastatin;
20 mg per day) for stabilizing intravascular plaque, were
administered following the stent implantation. The patient is
required to continue to take aspirin and Lipitor for life. After
the patient was discharged from hospital, all the symptoms went
into remission.
Discussion
Blood flows through the cleft of the carotid artery
intima and into the cystic degeneration of the vascular media, thus
forming a carotid artery dissection. To the best of our knowledge,
carotid artery dissection induced by radiotherapy occurs
infrequently. Furthermore, the pathogenesis of radiation-induced
carotid artery dissection has yet to be fully elucidated.
Based on a review of the literature, one of the
side-effects of radiotherapy is endothelial damage. Little et
al (1) proposed that
radiation-induced endothelial damage may simply be a consequence of
cell loss due to cell killing. In vitro studies have
revealed that radiation therapy causes the endothelial
colony-forming cells (ECFCs), which are the endothelial progenitor
cells of the vascular endothelium, to undergo large-scale
senescence, which acts as a forerunner of vascular damage and
subsequent atherosclerosis (2).
Circulating ECFCs have robust proliferative potential and form a
profusion of new blood vessels in vivo, thereby exerting an
important role in the repair of damaged vascular endothelium
(3,4).
On the basis of previous research, Pradhan et al (5) discovered that childhood survivors of
cancer who received radiotherapy had statistically lower ECFCs and
circulating endothelial cells (P<0.05) compared with those who
received no radiotherapy. However, radiation-induced genomic
instability, oxidative stress-disrupted mitochondrial function and
accelerated cellular senescence have also been implicated in the
pathogenesis of endothelial damage and subsequent arteriosclerosis
(6–10). Several previous studies demonstrated
that radiotherapy of head-and-neck cancer may result in an increase
in carotid intima-media thickness and carotid stenosis,
consequently leading to a higher risk of cerebrovascular events,
including transient ischemic attack and stroke (11–13).
In the present case report, the cause behind the
patient's common carotid artery dissection may be that radiotherapy
resulted in endothelial damage and the decline of endothelial
repair capacity: The damaged parts of his right common carotid
artery intima were not able to be repaired quickly, and blood
flowed through the cleft of his right common carotid artery intima
into the vascular media, thereby forming a carotid artery
dissection. The dissection is driven by the pressure of blood flow,
and gradually expands.
Radiation-induced carotid artery dissection is
generally asymptomatic at the early stages. Onset of acute ischemic
stroke is the predominant manifestation. For patients with
head-and-neck radiotherapy history, dissection should be
considered.
In conclusion, the detailed inquiry of a patient's
past history has a critical role in making a diagnosis of
radiation-induced common carotid artery dissection. This results
from the clinical presentation being non-specific. The condition
may progress rapidly, and result in a poor prognosis. Therefore, a
correct early diagnosis and initiation of appropriate therapy may
lead to rapid recovery, influencing the overall prognosis.
Acknowledgements
The present study was supported by a Research Fund
(grant no. 14411972000) of the Science and Technology Commission of
Shanghai (to DH.W.), a Research Fund (grant no. 201440332) of the
Shanghai Municipal Commission of Health and Family Planning (to
DH.W.), and a Research Fund (grant no. YG2013MS23) of Shanghai
Jiaotong University (to DH.W.).
References
|
1
|
Little MP, Tawn EJ, Tzoulaki I, Wakeford
R, Hildebrandt G, Paris F, Tapio S and Elliott P: Review and
meta-analysis of epidemiological associations between low/moderate
doses of ionizing radiation and circulatory disease risks and their
possible mechanisms. Radiat Environ Biophys. 49:139–153. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mendonca MS, Chin-Sinex H, Dhaemers R,
Mead LE, Yoder MC and Ingram DA: Differential mechanisms of
x-ray-induced cell death in human endothelial progenitor cells
isolated from cord blood and adults. Radiat Res. 176:208–216. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ingram DA, Mead LE, Moore DB, Woodard W,
Fenoglio A and Yoder MC: Vessel wall-derived endothelial cells
rapidly proliferate because they contain a complete hierarchy of
endothelial progenitor cells. Blood. 105:2783–2786. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yoder MC, Mead LE, Prater D, Krier TR,
Mroueh KN, Li F, Krasich R, Temm CJ, Prchal JT and Ingram DA:
Redefining endothelial progenitor cells via clonal analysis and
hematopoietic stem/progenitor cell principals. Blood.
109:1801–1809. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pradhan K, Mund J, Case J, Gupta S, Liu Z,
Gathirua-Mwangi W, McDaniel A, Renbarger J and Champion V:
Differences in circulating endothelial progenitor cells among
childhood cancer survivors treated with and without radiation. J
Hematol Thromb. 1:42015.PubMed/NCBI
|
|
6
|
Schultz-Hector S and Trott KR:
Radiation-induced cardiovascular diseases: Is the epidemiologic
evidence compatible with the radiobiologic data? Int J Radiat Oncol
Biol Phys. 67:10–18. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Andreassi MG and Botto N: DNA damage as a
new emerging risk factor in atherosclerosis. Trends Cardiovasc Med.
13:270–275. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Di Lisa F, Kaludercic N, Carpi A, Menabó R
and Giorgio M: Mitochondria and vascular pathology. Pharmacol Rep.
61:123–130. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Finsterer J: Is atherosclerosis a
mitochondrial disorder? Vasa. 36:229–240. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ito TK, Yokoyama M, Yoshida Y, Nojima A,
Kassai H, Oishi K, Okada S, Kinoshita D, Kobayashi Y, Fruttiger M,
et al: A crucial role for CDC42 in senescence-associated
inflammation and atherosclerosis. PLoS One. 9:e1021862014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kang HS, Roh JL, Lee SW, Kim SB, Choi SH,
Nam SY and Kim SY: Noncancer-related health events and mortality in
head and neck cancer patients after definitive radiotherapy: A
prospective study. Medicine (Baltimore). 95:e34032016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gujral DM, Shah BN, Chahal NS,
Bhattacharyya S, Hooper J, Senior R, Harrington KJ and Nutting CM:
Carotid intima-medial thickness as a marker of radiation-induced
carotid atherosclerosis. Radiother Oncol. 118:323–329. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wilbers J, Meijer FJ, Kappelle AC,
Kaanders JH, Boogerd W, Dorresteijn LD, van Dijk EJ and Steens SC:
Magnetic resonance imaging of the carotid artery in long-term head
and neck cancer survivors treated with radiotherapy. Acta Oncol.
54:1175–1180. 2015. View Article : Google Scholar : PubMed/NCBI
|