Introduction
Glioblastoma multiforme is a highly malignant glioma
of astrocytic origin (1). The tumor
is defined as grade IV according to the World Health Organization
(WHO) classification, and is a cytologically malignant, mitotically
active, necrosis-prone neoplasm, typically associated with rapid
pre- and postoperative disease evolution and a fatal outcome, with
a median survival of ~12 months (2,3).
With an incidence of 3.19/100.000 patient years,
glioblastoma multiforme is the most common glioma in adults
(typical age, 50–70 years), located mostly in the frontotemporal
cerebral lobes (1,4).
The treatment of choice currently consists of
maximal safe surgical resection and postoperative concomitant
radiochemotherapy (RCTx), followed by further chemotherapy with the
orally administered alkylating drug temozolomide (5). The indication for radiotherapy (RTx)
depends on the patient's general condition [Karnofsky performance
status (PS) or Eastern Cooperative Oncology Group PS], age and
extent of surgery (6,7). Typically, conformal RTx consists of
54–60 Gy (1.8–2.0 Gy per fraction), with limited safety margins of
a maximum 2.0 cm. Long-term local control is difficult to achieve.
Extracranial metastases are reported to occur in 0.4–0.5% of all
cases (8–12). In 1928, Davis first reported a patient
with disseminated glioblastoma (13).
The affected organs included the lung, upper extremity soft tissue
and chest wall. The natural history of glioblastomas that
metastasize to organs outside the central nervous system is largely
unknown. Between 1928 and 2009, 88 cases of extracranial metastasis
from glioblastoma (n=83) and gliosarcoma (n=5) have been published,
reported and analyzed by Lun et al (14). In 2015, Pietschmann et al
reviewed existing data and performed a new meta-analysis with 150
cases (15). In addition to brain
stem and spinal axis, lymph nodes and visceral organs, including
the liver, lung, pleura and bones, were found to be involved. In
only one of all documented cases an extracranial oral cavity
metastasis of significant extent and exhibiting rapid growth was
described (16).
Case report
A 70-year-old female patient was admitted to our
hospital suffering from progressive lack of concentration and
cognitive deficit. The patient's husband also reported a
personality change. Arterial hypertension, hyperthyroidism and
lipometabolic disorder were documented, without other
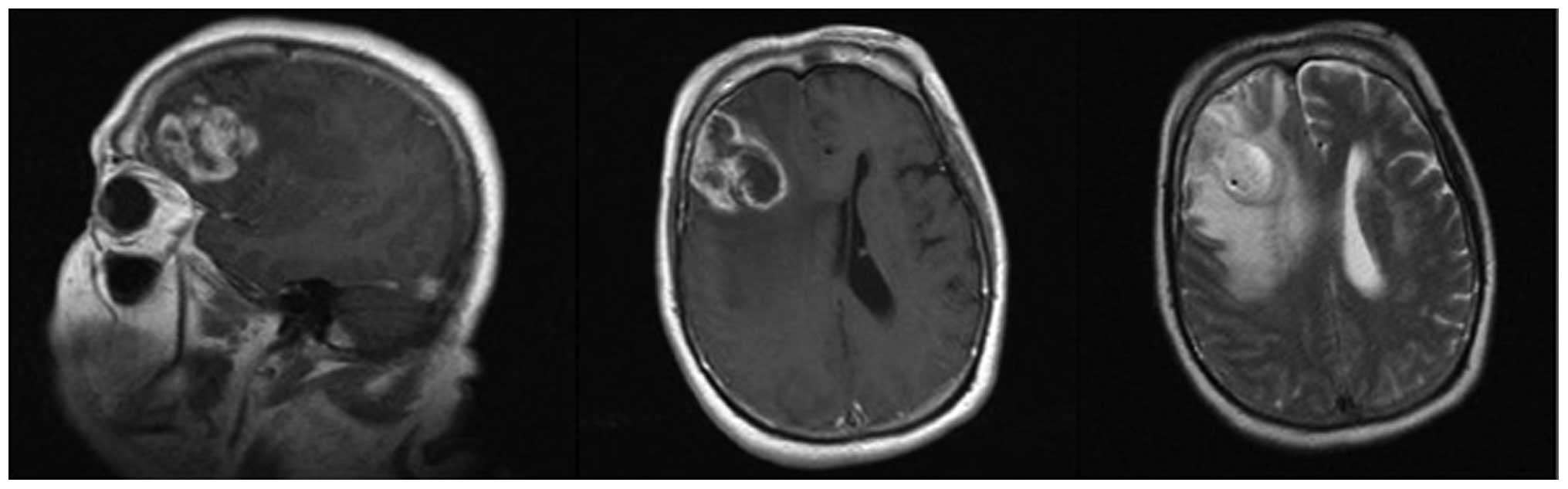
comorbidities. Initially, we performed magnetic resonance imaging
(MRI) of the head, which revealed a massive tumor in the right
frontal lobe, with perifocal oedema and midline dislocation of 6
mm, suspicious for glioblastoma (Fig.
1). The tumor was sized 4.2×2.8×3.9 cm. Navigated maximal safe
tumor excision was performed with osteoplastic craniotomy and dura
mater plastic surgery. The postoperative course was uneventful.
Histology and immunohistochemical investigation revealed a
O6-methylguanine-DNA methyltransferase-positive
glioblastoma multiforme, WHO grade IV. Adjuvant RCTx was initially
performed with low-dose temozolomide 140 mg/day, subsequently
escalated to the standard dose of 200 mg/day (total dose 60 Gy, 2
Gy per fraction).
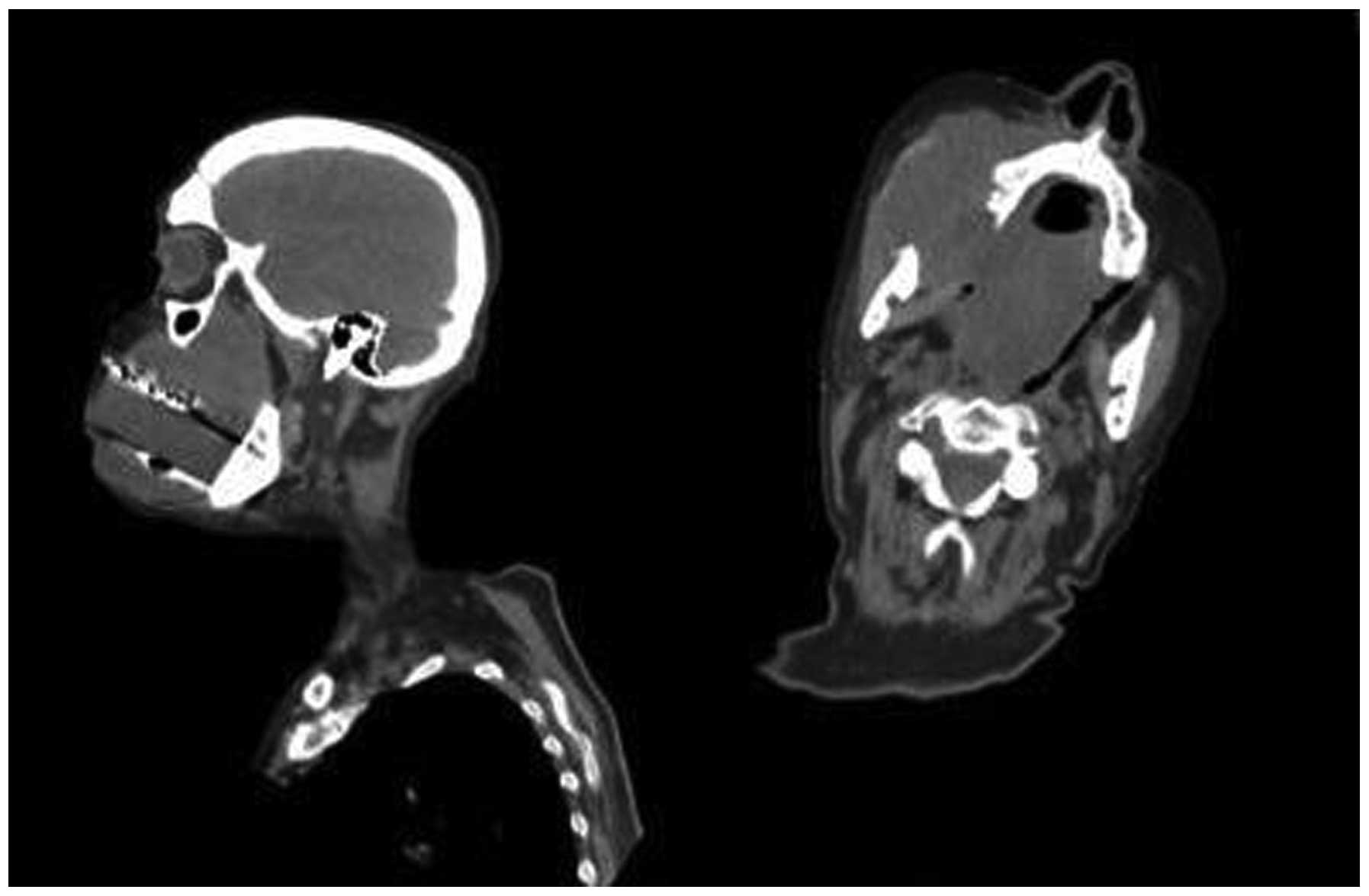
One year after the diagnosis, the patient developed
a rapidly progressive oral cavity tumor, filling the entire buccal
cavity within 2 weeks (Fig. 2).
Following biopsy, the histological examination revealed a necrotic
retromaxillary metastasis of the previously diagnosed glioblastoma,
exhibiting histological characteristics identical to those of the
primary resected tumor. Systemic metastases were not identified.
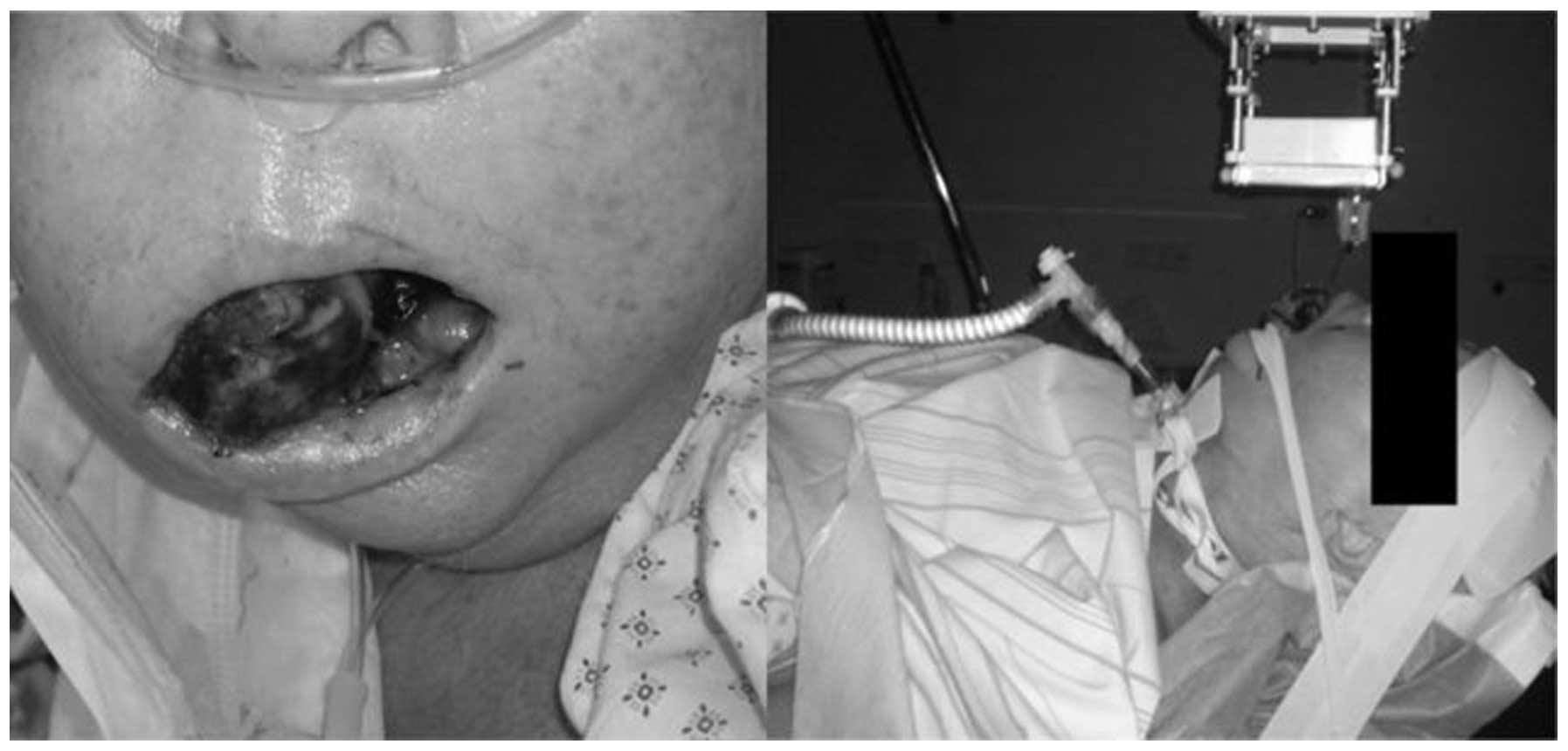
The patient was unable to speak or eat (Fig. 3). Following extensive
interdisciplinary discussion, we decided to proceed with local
palliative RTx and supportive measures. The patient developed
massive breathing difficulties, necessitating transfer to the
intensive care unit, followed by tracheotomy and immediate
mechanical ventilation. We first planned to administer a total of
45 Gy/3 Gy per fraction. In the light of rapid progress of the
tumor, a dose of 5 Gy per fraction was applied (Fig. 3). However, after 4 applications, the
patient's relatives requested discontinuation of RTx and the
patient succumbed to the disease soon thereafter.
Discussion
We herein report the case of a patient suffering
from glioblastoma with subsequent retromaxillary metastatic spread
completely filling the buccal cavity. Initial treatment with
cranial tumor extirpation followed by RCTx with 60 Gy and
temozolomide was performed. At the time of relapse and clinical
deterioration, the patient was treated with 20 Gy to the metastatic
area. However, RTx was discontinued and the patient succumbed to
the disease soon thereafter. Extracranial metastasis from
glioblastoma remains an uncommon finding (15). Thus far, a massive metastasis
completely filling the buccal cavity has only been reported in 1996
by Horiuchi et al (16) in a
41-year-old female. In contrast to our patient, simultaneous local
recurrence of the tumor was described. MRI and computed tomography
scans revealed orbital, nasal and oral masses extending inferiorly
from the recurrent tumor in the right temporal lobe through the
anterior and middle skull base. The oral cavity tumor and swelling
of the patient's face grew rapidly. The common characteristics of
the two cases are rapid growth and gender of the patient, but no
connection to cranial tissue was radiologically detected in our
patient.
The reasons for such extensive spread in this
particular location and the growth rate are not well understood. A
necessary requirement for extracranial metastasis is tumor cells
crossing the dura mater, which is the most important barrier.
Surgery and radiation therapy may lead to dural damage and
potentially facilitate extracranial extension. In our case, no
lesion of the dura mater was documented during surgery. A
ventricular systemic shunt was not indicated. Our 70-year-old
patient underwent craniotomy followed by RTx with simultaneous
chemotherapy. Younger patients exhibit an increased risk of
extraneural involvement due to prolonged survival (15,17). The
most common sites of extracranial metastases from glioblastoma are
the lungs, bone (bone marrow), lymph nodes and soft tissues
(14). This is the second report of
an extracranial metastasis with a retromaxillary localization,
exhibiting rapid growth and completely filling the buccal cavity.
Glioblastoma is a tumor with fatal outcome. Although extracranial
metastases remain extremely uncommon, extraneural spread of the
tumor is possible and must be considered in symptomatic patients
during follow-up. Extracranial glioblastomas may present with an
extraordinarily rapid progression pattern, as in our case.
Therefore, fast decision-making and treatment initiation are
crucial for optimal palliative treatment. Further investigation is
required to improve therapy and outcome.
References
|
1
|
Louis DN, Perry A, Burger P, Ellison DW,
Reifenberger G, von Deimling A, Aldape K, Brat D, Collins VP,
Eberhart C, et al: International Society Of Neuropathology -
Haarlem: International Society of Neuropathology - Haarlem
consensus guidelines for nervous system tumor classification and
grading. Brain Pathol. 24:429–435. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Krex D, Klink B, Hartmann C, von Deimling
A, Pietsch T, Simon M, Sabel M, Steinbach JP, Heese O, Reifenberger
G, et al: Long-term survival with glioblastoma multiforme. Brain.
130:2596–2606. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Visser O, Ardanaz E, Botta L, Sant M,
Tavilla A and Minicozzi P: EUROCARE-5 Working Group: Survival of
adults with primary malignant brain tumours in Europe; Results of
the EUROCARE-5 study. Eur J Cancer. September 5–2015.(Epub ahead of
print). doi: 10.1016/j.ejca.2015.07.032. View Article : Google Scholar
|
|
4
|
DeAngelis LM: Brain tumors. N Engl J Med.
344:114–123. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Preusser M, de Ribaupierre S, Wöhrer A,
Erridge SC, Hegi M, Weller M and Stupp R: Current concepts and
management of glioblastoma. Ann Neurol. 70:9–21. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dolecek TA, Propp JM, Stroup NE and
Kruchko C: CBTRUS statistical report: Primary brain and central
nervous system tumors diagnosed in the United States in 2005–2009.
Neuro Oncol. 14(Suppl 5): 41–49. 2012. View Article : Google Scholar
|
|
7
|
Stummer W, Reulen HJ, Meinel T, Pichlmeier
U, Schumacher W, Tonn JC, Rohde V, Oppel F, Turowski B,
Woiciechowsky C, et al: Extent of resection and survival in
glioblastoma multiforme: Identification of and adjustment for bias.
Neurosurgery. 62:564–576; discussion 564–576. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Smith DR, Hardman JM and Earle KM:
Metastasizing neuroectodermal tumors of the central nervous system.
J Neurosurg. 31:50–58. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pasquier B, Pasquier D, N'golet A, Panh MH
and Couderc P: Extraneural metastases of astrocytomas and
glioblastomas: Clinicopathological study of two cases and review of
literature. Cancer. 45:112–125. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Astner ST, Pihusch R, Nieder C, Rachinger
W, Lohner H, Tonn JC, Molls M and Grosu AL: Extensive local and
systemic therapy in extraneural metastasized glioblastoma
multiforme. Anticancer Res. 26:4917–4920. 2006.PubMed/NCBI
|
|
11
|
Elena A, Melina C, Raffaele N, Carlo B,
Vittoria N, Francesco A, Gaetano F and Marica E: Extraneural
metastases in glioblastoma patients: Two cases with YKL-40-positive
glioblastomas and a meta-analysis of the literature. Neurosurg Rev.
39:37–46. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ray A, Manjila S, Hdeib AM, Radhakrishnan
A, Nock CJ, Cohen ML and Sloan AE: Extracranial metastasis of
glioblastoma: Three illustrative cases and current review of the
molecular pathology and management strategies. Mol Clin Oncol.
3:479–486. 2015.PubMed/NCBI
|
|
13
|
Davis L: Spongioblastoma multiforme of the
brain. Ann Surg. 87:8–14. 1928.PubMed/NCBI
|
|
14
|
Lun M, Lok E, Gautam S, Wu E and Wong ET:
The natural history of extracranial metastasis from glioblastoma
multiforme. J Neurooncol. 105:261–273. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pietschmann S, von Bueren AO, Kerber MJ,
Baumert BG, Kortmann RD and Müller K: An individual patient data
meta-analysis on characteristics, treatments and outcomes of
glioblastoma/gliosarcoma patients with metastases outside of the
central nervous system. PLoS One. 10:e01215922015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Horiuchi T, Osawa M, Itoh N, Kobayashi S,
Nitta J and Hongo K: Extradural extension of glioblastoma
multiforme into the oral cavity: Case report. Surg Neurol.
46:42–46. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bertolini F, Zunarelli E, Baraldi C,
Valentini A, Del Giovane C, Depenni R, Falasca A, Giacobazzi P,
Malagoli M, Meletti S, et al: Survival in patients with newly
diagnosed conventional glioblastoma: A modified prognostic score
based on a single-institution series. Tumori. 98:756–761.
2012.PubMed/NCBI
|