Introduction
Despite advanced surgery, radiotherapy and
chemotherapy, glioblastoma relapses in almost all patient, with
tumors recurring locally or in a disseminated pattern.
Dissemination, an end-stage complication of glioblastoma, is
considered to be untreatable, with a reported mean survival time of
2–4 months (1–3). Furthermore, previous reports have
indicated that chemotherapy for disseminated glioblastoma exhibits
limited therapeutic efficacy (1,3,4). Bevacizumab, a monoclonal antibody that
inhibits vascular endothelial growth factor, is an effective
established therapy for recurrent glioma, following treatment with
radiotherapy plus temozolomide. However, there has been no previous
report of the effectiveness of bevacizumab in disseminated
glioblastoma following multidisciplinary therapy.
Encephalocraniocutaneous lipomatosis (ECCL) is a
rare, sporadically occurring neurocutaneous syndrome characterized
by the presence of skin lesions and ocular and central nervous
system (CNS) anomalies (5). Since
Haberland and Perou reported the first case in 1970, ~60 patients
have been reported to date (6,7), and the
etiology of ECCL remains unknown thus far. Although CNS
abnormalities, such as intracranial lipomas and arachnoid cysts,
are one of the major characteristics of ECCL, the association of
ECCL with a malignant brain tumor has never been reported. We
herein report a primary glioblastoma in an adult ECCL patient who
exhibited an intense and favorable response to bevacizumab.
Case report
Medical history and diagnosis
A 32-year-old woman was referred to Shizuoka City
Shimizu Hospital from a local Children's Hospital at the age of 15
years. At birth, the patient exhibited multiple malformations,
including alopecia with underlying fatty tissue on her right
frontal scalp, choristoma on her right eye, and a large head
circumference. At the age of 4 months, the patient had been
diagnosed with hydrocephalus, an intracranial arachnoid cyst and
lipoma, all of which were identified during brain imaging performed
at the Children's Hospital.
Pathology and surgeries
For her first surgery, the patient underwent a right
frontotemporal craniotomy with fenestration of the arachnoid cyst
and placement of a ventriculoperitoneal shunt. Although the patient
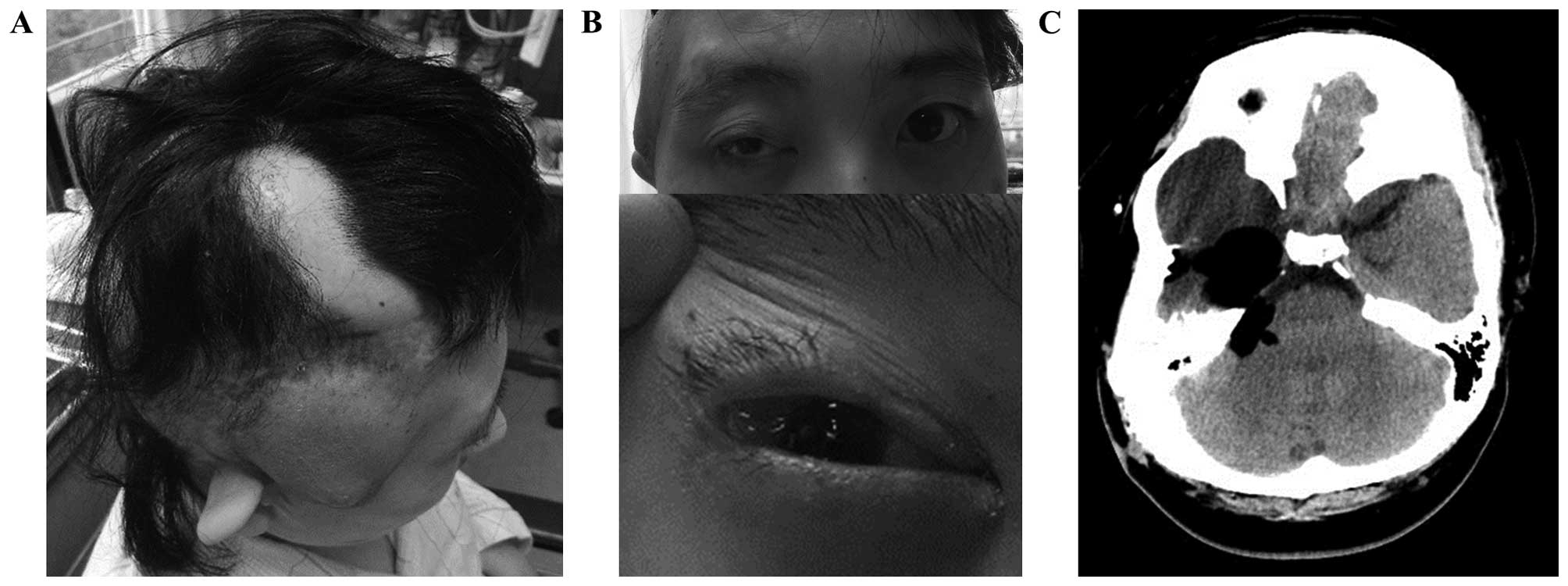
displayed the typical characteristics of ECCL at birth (Fig. 1A-C), she was diagnosed with Goldenhar
syndrome, a similar congenital disease characterized by spinal and
craniofacial abnormalities during early childhood. The patient was
referred to our institution for the consecutive treatment of
hydrocephalus and convulsions at the age of 15 years and underwent
revision of the ventriculoperitoneal shunt several times at the
Children's Hospital and at our institution.
At the age of 32 years, the patient developed a gait
disturbance and mild left hemiparesis; these symptoms gradually
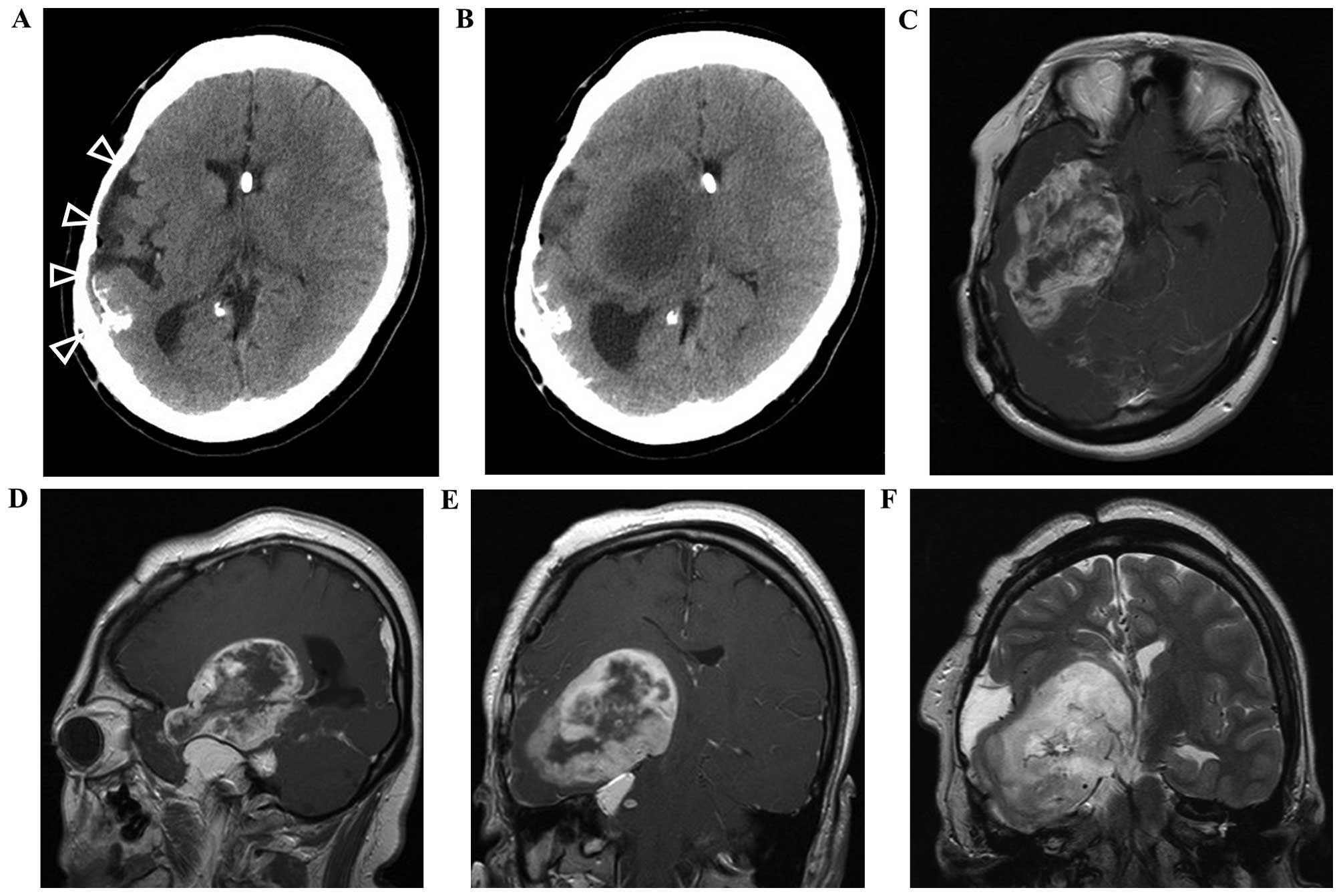
worsened. A head computed tomography (CT) scan revealed a
low-density expanded lesion located at the right temporal lobe
extending throughout the right basal ganglia, although no mass
lesions were observed on a previous CT conducted 1 year prior
(Fig. 2A and B). Brain
gadolinium-enhanced magnetic resonance imaging (MRI) revealed a
ring-enhanced mass adjacent to the upper surface of the lipoma at
the right middle cranial fossa (Fig.
2C-E). Although the mass was large (maximum diameter, 8.0 cm),
a small amount of perifocal edema was observed (Fig. 2F). A cerebral angiography was
performed, demonstrating an arteriovenous shunt and strong tumor
staining. The tumor was preoperatively diagnosed as glioblastoma,
and the patient underwent a second right frontotemporal craniotomy
with partial removal of the tumor. The surgery was performed with
the assistance of a navigation system (StealthStation
S7®; Medtronic, Minneapolis, MN). The tumor was highly
hemorrhagic, and a small portion of the upper dorsal mass of the
gadolinium-enhanced lesion remained (Fig.
3).
Postoperative results and additional
treatment
A postoperative MRI examination revealed a cerebral
infarction located in the right anterior limb of the internal
capsule and basal ganglia. No consciousness disorder was observed,
and the left lower extremity palsy improved to the point of
independent gait, whereas the left upper extremity palsy
deteriorated. The histological diagnosis of the tumor was
glioblastoma (Fig. 4). After the
operation, the patient's condition was diagnosed as ECCL based on
its characteristic features. At 3 weeks post-resection, local
radiotherapy (72 Gy in 60 fractions over 6 weeks) and temozolomide
chemotherapy (75 mg/m2/day) were initiated. An adjuvant
chemotherapy regimen was next initiated, consisting of temozolomide
at 150 mg/m2 daily for 5/28 days at our outpatient
clinic. After six courses of the adjuvant chemotherapy and 8 months
after the resection, the patient complained of occasional
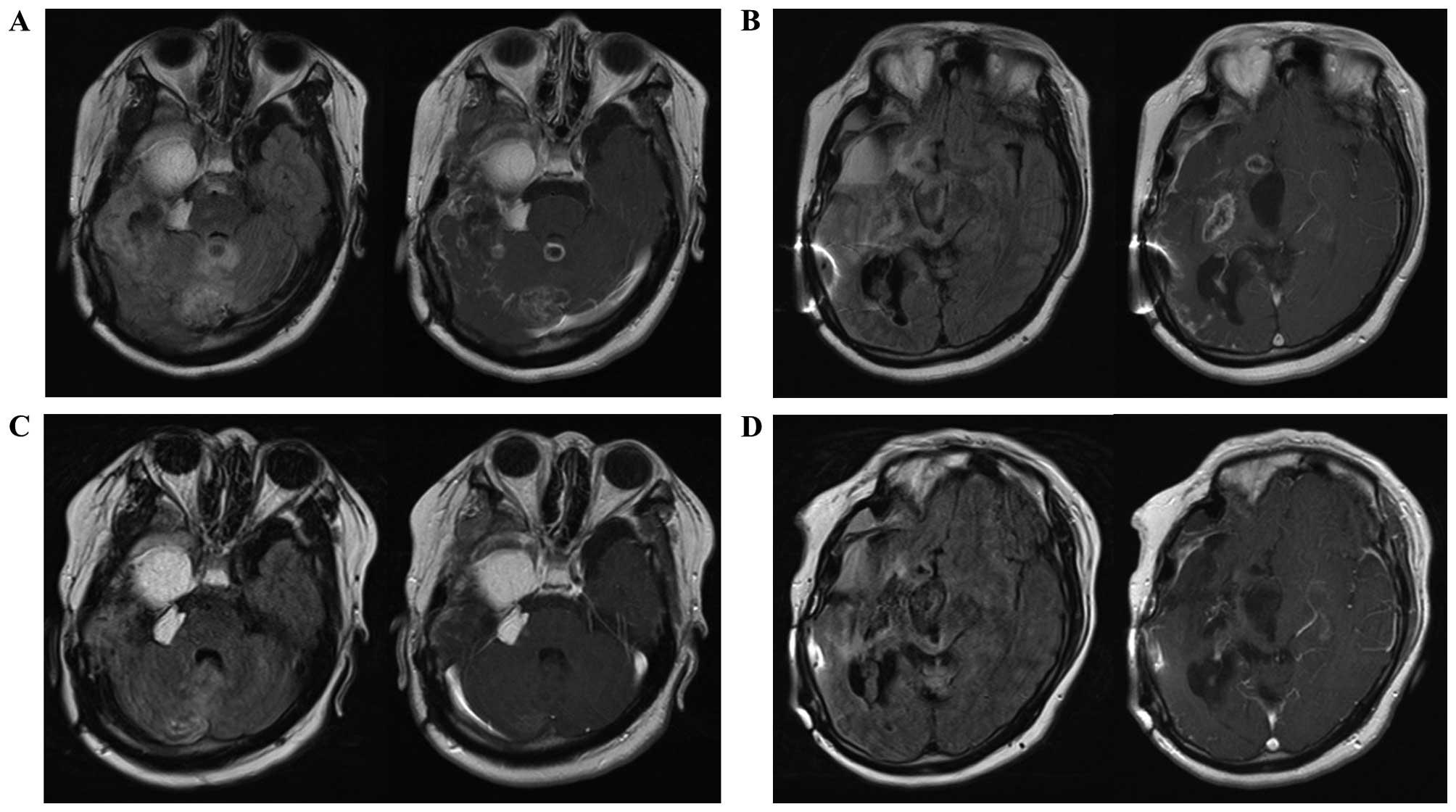
headaches. A tumor recurrence at the anteromedial wall of the
resected cavity and a disseminated tumor located in the cerebellum
were confirmed on MRI examination (Fig.
5A and B). Additional chemotherapy with bevacizumab was
initiated (10 mg/kg every 2 weeks), concomitantly with
temozolomide. The headaches resolved immediately after the
initiation of bevacizumab chemotherapy. After five courses of
bevacizumab chemotherapy, another MRI examination revealed that the
residual, relapsed and disseminated tumors had completely
disappeared. Temozolomide and bevacizumab chemotherapy has now been
continued for 2.5 years. The tumor has not recurred, and there have
been no complications (Fig. 5C and
D). Written informed consent was obtained for the patient for
the publication of the case details.
Discussion
ECCL is a rare neurocutaneous disorder involving
multiple organ systems, which typically manifests unilaterally
(5,6).
To the best of our knowledge, only 3 cases of brain tumors, which
were fairly different from the present case, have been reported in
patients with ECCL to date (Table I)
(7–9).
Although all the previous cases were benign tumors and had
developed during childhood, the tumor in the present case developed
in a young adult woman, and the diagnosis of glioblastoma was
histologically confirmed. Of note, all the abnormalities, including
the brain tumor, were located ipsilaterally in the present case,
whereas the tumors had occurred in the midline or on the
contralateral side from the other disorders in the previous cases.
This evidence strongly indicates that the glioblastoma arose on the
biological background of ECCL in this case.
 | Table I.Brain tumors in patients with
encephalocraniocutaneous lipomatosis. |
Table I.
Brain tumors in patients with
encephalocraniocutaneous lipomatosis.
| Case | Age, years | Gender | Location of brain
tumor | Pathological
diagnosis | Location of other
abnormalities | Refs. |
|---|
| 1 | 3 | Male | Suprasellar
(midline) | Pilocytic
astrocytoma | Coloboma (left eye),
alopecia (occipital scalp) | (8) |
| 2 | 7 | Female | Floor of the third
ventricle (midline) | Papillary
glioneuronal tumor | Choristoma (left
eye), alopecia (right scalp), arachnoid cyst (left middle
fossa) | (9) |
| 3 | 12 | Female | Left internal
capsule | Pilocytic
astrocytoma | Intradermic nodes
(right eye), alopecia (right scalp), arachnoid cyst (right middle
fossa) | (7) |
| 4 | 32 | Female | Right temporal
lobe | Glioblastoma | Choristoma (right
eye), alopecia (right scalp), intracranial lipoma (right middle
fossa) | Present study |
Bevacizumab has recently been administered to
patients with anaplastic astrocytoma or glioblastoma and has
resulted in prolonged progression-free survival, but has not been
successful in prolonging overall survival (10). The reduction of perifocal edema
without any antitumor effects has been considered as the main
effect of bevacizumab (11). However,
in the present case, the recurrent and disseminated tumors
disappeared and have not recurred for 2.5 years after the addition
of bevacizumab therapy, thus demonstrating a strong antitumor
effect in this patient. Glioblastomas are classified as the final
form of malignant astrocytic tumors of different etiologies.
Several differences, including age at onset, the minimal presence
of perifocal edema, and a strong antitumor response to bevacizumab,
were observed between this case and ‘typical’ glioblastomas. These
results suggest that the present case was an uncommon type of
glioblastoma associated with ECCL. Both ECCL and glioblastoma are
rare diseases, so their association in our case is unlikely to be a
coincidence. The reason for the atypically strong antitumor effect
of bevacizumab in this case remains unknown. The biological
differences between this particular glioblastoma in our ECCL
patient and common glioblastomas remain unknown, as this is the
first case of ECCL coexisting with a glioblastoma. Further clinical
information regarding the genetic background of ECCL may contribute
to the investigation of glioblastoma therapy.
In summary, to the best of our knowledge, this is
the first case with a confirmed significant response and long-term
clinical remission in a patient with disseminated glioblastoma who
received bevacizumab therapy. This case is also the first report of
ECCL in association with glioblastoma.
References
|
1
|
Arita N, Taneda M and Hayakawa T:
Leptomeningeal dissemination of malignant gliomas. Incidence,
diagnosis and outcome. Acta Neurochir (Wien). 126:84–92. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Awad I, Bay JW and Rogers L:
Leptomeningeal metastasis from supratentorial malignant gliomas.
Neurosurgery. 19:247–251. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Greenberg AD, Scatliff JH, Selker RG and
Marshall MD: Spinal cord metastasis from bronchogenic carcinoma. A
case report. J Neurosurg. 23:72–75. 1965. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Delattre JY, Walker RW and Rosenblum MK:
Leptomeningeal gliomatosis with spinal cord or cauda equina
compression: A complication of supratentorial gliomas in adults.
Acta Neurol Scand. 79:133–139. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Moog U: Encephalocraniocutaneous
lipomatosis. J Med Genet. 46:721–729. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Haberland C and Perou M:
Encephalocraniocutaneous lipomatosis. A new example of
ectomesodermal dysgenesis. Arch Neurol. 22:144–155. 1970.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Valera ET, Brassesco MS, Scrideli CA, de
Castro Barros MV, Santos AC, Oliveira RS, Machado HR and Tone LG:
Are patients with encephalocraniocutaneous lipomatosis at increased
risk of developing low-grade gliomas? Childs Nerv Syst. 28:19–22.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brassesco MS, Valera ET, Becker AP,
Castro-Gamero AM, de Aboim Machado A, Santos AC, Scrideli CA,
Oliveira RS, Machado HR and Tone LG: Low-grade astrocytoma in a
child with encephalocraniocutaneous lipomatosis. J Neurooncol.
96:437–441. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Phi JH, Park SH, Chae JH, Wang KC, Cho BK
and Kim SK: Papillary glioneuronal tumor present in a patient with
encephalocraniocutaneous lipomatosis: Case report. Neurosurgery.
67:E1165–E1169. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chinot OL, Wick W, Mason W, Henriksson R,
Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea
D, et al: Bevacizumab plus radiotherapy-temozolomide for newly
diagnosed glioblastoma. N Engl J Med. 370:709–722. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Narayana A, Gruber D, Kunnakkat S,
Golfinos JG, Parker E, Raza S, Zagzag D, Eagan P and Gruber ML: A
clinical trial of bevacizumab, temozolomide, and radiation for
newly diagnosed glioblastoma. J Neurosurg. 116:341–345. 2012.
View Article : Google Scholar : PubMed/NCBI
|