Introduction
Adenoid cystic carcinoma is a relatively rare
epithelial tumor of the minor salivary glands that is clinically
characterized by slow growth, high frequency of local recurrence
and perineural invasion (1,2). The most common localization is the
parotid gland, followed by the submandibular and sublingual glands
(2). The reported frequency of
occurrence in the tongue is 19.8%, with 85% occurring in the tongue
base (3–5). Surgical excision with wide margins is
the treatment of choice when the cancer metastasizes to the lymph
nodes; postoperative radiotherapy is recommended for cases with
positive surgical margins (2,4). In this case study, an adenoid cystic
carcinoma of the tongue base that recurred locally following
postoperative radiation therapy, was successfully treated with
brachytherapy.
Case report
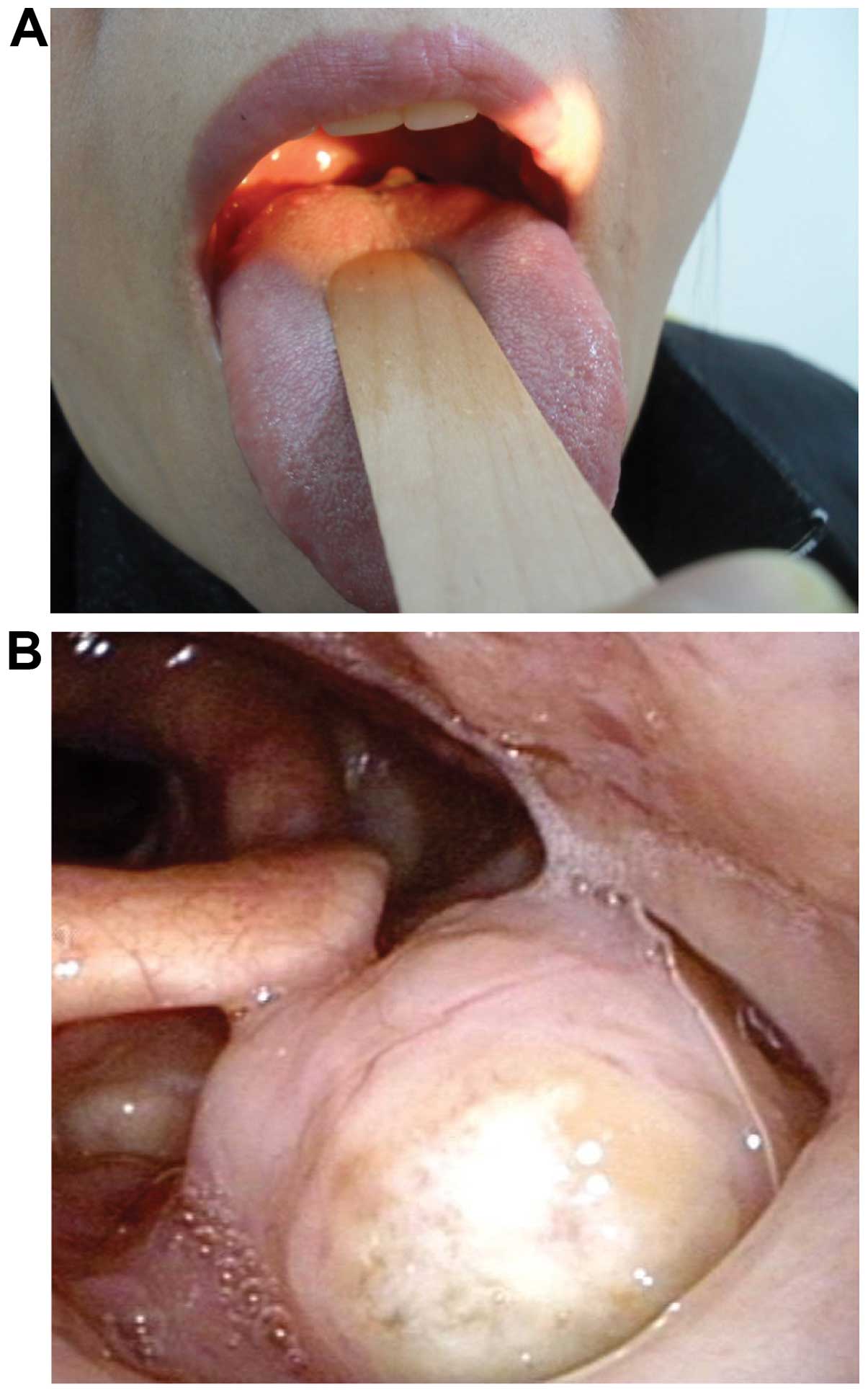
A 50-year-old woman complained of a sore throat and
discomfort during swallowing. An intraoral examination by
laryngoscope revealed a whitish yellow cystic mass at the base of
the tongue. The histopathological analysis revealed an adenoid
cystic carcinoma; on magnetic resonance imaging (MRI), the tumor
was sized 25×25×30 mm and invaded the intrinsic muscle of the left
posteroinferior tongue. The tumor was staged as cT4N0M0. Following
wide local excision, three-dimensional conformal radiotherapy was
performed at a total dose of 56 Gy. Complete remission was obtained
following radiotherapy; however, during follow-up, local recurrence
was observed at the tongue base on visual inspection and
laryngoscopic examination (Fig. 1).
The suspected recurrence was investigated by MRI, revealing a
primary tumor confined to the lateral tongue base. After detecting
the tumor recurrence, a biopsy was performed, confirming that the
recurrence of the adenoid cystic carcinoma was confined to the
mucosa. Considering the patient's age, brachytherapy was performed
in the area surrounding the tumor to preserve the tongue
function.
Brachytherapy was administered using a
computer-assisted high-dose rate remote afterloading dose delivery
system (MicroSelectron; Nucletron-Elekta, Veenendaal, The
Netherlands) utilizing a single 192Ir source with an
activity at installation of ~370 GBq. A total dose of 30 Gy
(biologically effective dose, 36.0 Gy) was administered twice per
week in 3-Gy fractions. The brachytherapy target volume was
determined individually for this patient using the MRI findings.
The target volume encompassed the recurrent tumor as visualized by
MRI and endoscopic examination, as well as a 1.5-cm margin proximal
and distal to the tumor. The image with a dummy source, which was
taken during a conventional simulation, was transferred to the
intraluminal brachytherapy catheter. The geometrically optimized
dose was generated using the Plato BPS v14.2.6 planning system
(Nucletron-Elekta) (Fig. 2).
Considering the lesions, we used the mold with a left lateral
position. The velum stimulation often results in severe gag reflex
during treatment. In this case, the uvula was anesthetized using
lidocaine spray prior to treatment (Fig.
3). Three months after brachytherapy, the patient underwent MRI
and laryngoscopic examination; the mass was not identified
(Fig. 4). In addition, no cancer
cells were detected at the site of the previous tumor biopsy.
During treatment, acute grade 2 radiation mucositis occurred, which
subsided within 3 week after treatment completion. Chronic side
effects did not occur. There has been no tumor recurrence during
the 2 years of follow-up.
This study was approved by the Ethics Committee of
Chonbuk National University Hospital Institutional Review Board and
was performed in compliance with the guidelines of the Helsinki
Declaration of 1975, as revised in 2008. The patient provided
written informed consent and the clinical data were anonymized for
statistical work-up.
Discussion
Adenoid cystic carcinomas constitute ~29.6% of all
minor salivary gland tumors, and their occurrence in the tongue is
extremely rare (4.4%) (3,5,6). The most
common treatment for adenoid cystic carcinoma is wide surgical
excision (4). Alternative treatment
options include radiotherapy, chemotherapy and combination therapy
(surgical excision and radiotherapy, or radiotherapy and
chemotherapy) (5,6). High recurrence rates occur following
surgical resection of the lesion, but complete resection is
difficult, as the resection margin is often positive due to the
presence of a tumor cell (5,7). Therefore, even when surgical resection
is performed, postoperative radiation therapy should be considered
in the majority of the patients for conservative treatment. In
addition, adenoid cystic carcinoma exhibits strong neurotropism and
tends to invade nerves (6,8). Consequently, surgical excision or
radiotherapy alone may fail to eliminate relapse in the surgical
margins (4,6). Distant metastasis is also occasionally
observed in the cervical lymph nodes, lungs, bone and brain. In our
patient, external beam radiotherapy following surgery made it
necessary to limit the dosage of additional external beam radiation
to the peripheral organs despite re-recurrence, making treatment
difficult (9,10). Although total glossectomy is an option
following postoperative radiotherapy, due to the age of the patient
and the desire for long-term, postoperative functional recovery,
mold brachytherapy was performed locally. The additional radiation
therapy doses were a limitation, but since no serious adverse
events occurred, we were able to end treatment after observing
complete disappearance of the lesions. There was no tumor
recurrence during follow-up. However, adenoid cystic carcinoma may
be associated with long-term local recurrence and distant
metastasis, indicating the need for additional follow-up. If local
recurrence occurs at the primary site following long-term disease
control, brachytherapy should be considered.
Adenoid cystic carcinoma recurrence following
surgery is commonly reported after conservative treatment is
applied. However, when recurrence occurs after radiation therapy,
the most common treatment is complete resection of the tongue.
However, when preservation of organ function is desired,
brachytherapy should be considered. In the present case, complete
remission was achieved in a patient with recurrent adenoid cystic
carcinoma following brachytherapy, without serious side
effects.
Acknowledgements
The present study was supported by a fund from the
Institute of Clinical Medicine of Chonbuk National
University-Biomedical Research Institute, Chonbuk National
University Hospital, Jeonju, Republic of Korea.
References
|
1
|
Raux-Rakotomalala F, Houliat T, Martel J,
Stoll D, Bébéar JP and Darrouzet V: Adenoid cystic carcinoma of
head and neck: A review of 30 cases. Rev Laryngol Otol Rhinol
(Bord). 124:235–241. 2003.(In French). PubMed/NCBI
|
|
2
|
Iseli T, Karnell LH, Graham SM, Funk GF,
Buatti JM, Gupta AK, Robinson RA and Hoffman HT: Role of
radiotherapy in adenoid cystic carcinoma of the head and neck. J
Laryngol Otol. 123:1137–1144. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Namazie A, Alavi S, Abemayor E, Calcaterra
TC and Blackwell KE: Adenoid cystic carcinoma of the base of the
tongue. Ann Otol Rhinol Laryngol. 110:248–253. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Soares EC, Carreiro Filho FP, Costa FW,
Vieira AC and Alves AP: Adenoid cystic carcinoma of the tongue:
Case report and literature review. Med Oral Patol Oral Cir Bucal.
13:E475–E478. 2008.PubMed/NCBI
|
|
5
|
Traiantafillidou K, Dimitrakopoulous J,
Iprdanidis F and Koufogiannis D: Management of adenoid cystic
carcinoma of minor salivary glands. J Oral Maxillofas Surg.
64:1114–1120. 2006. View Article : Google Scholar
|
|
6
|
Iyer NG, Kim L, Nixon IJ, Palmer F, Kraus
D, Shaha AR, Shah JP, Patel SG and Ganly I: Factors predicting
outcome in malignant minor salivary gland tumors of the oropharynx.
Arch Otoloryngol Head and Neck Surg. 136:1240–1247. 2010.
View Article : Google Scholar
|
|
7
|
Bradely PJ: Adenoid cystic carcinoma of
the head and neck: A review. Curr Opin Otolaryngol Head Neck Surg.
12:127–132. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Carrasco Ortiz D and Aldape Barrios B:
Adenoid cystic carcinoma of the dorsum of the tongue: Presentation
of a case. Med Oral Patol Oral Cir Bucal. 11:E417–E420. 2006.(In
English, Spanish). PubMed/NCBI
|
|
9
|
Jaber MA: Intraoral minor salivary gland
tumors: A review of 75 cases in a Libyan population. Int J Oral
Maxillofac Surg. 35:150–154. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang D, Li Y, He H, Liu L, Wu L and He Z:
Intraoral minor salivary gland tumors in a Chinese population: A
retrospective study on 737 cases. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 104:94–100. 2007. View Article : Google Scholar : PubMed/NCBI
|