Introduction
Endometrial cancer (EC) is the third most common
gynecological malignancy worldwide, after breast and cervical
cancers (1). While insulin
resistance and diabetes mellitus (DM) may facilitate the initiation
and progression of EC, effective DM control has been suggested to
prevent or modulate EC (2).
Metformin is an oral insulin-sensitizing agent used as first-line
therapy for type 2 DM (3). As shown
in a recent review, several in vitro and observational
studies have evaluated the potential benefits of metformin in the
prevention or treatment of gynecological cancers (4,5). In
vitro data have demonstrated that metformin administration
inhibits the growth and decreases the invasion and metastasis of EC
cell lines (6,7). A multi-institutional study recently
demonstrated that metformin use was associated with an improvement
in the recurrence-free and overall survival of patients with EC
(8). We herein describe the case of
a patient with EC who was treated with metformin and remained
disease-free during a long follow-up period.
Case report
A 79-year-old woman, gravida 1, para 0, presented
with lower abdominal pain. The patient was examined in a
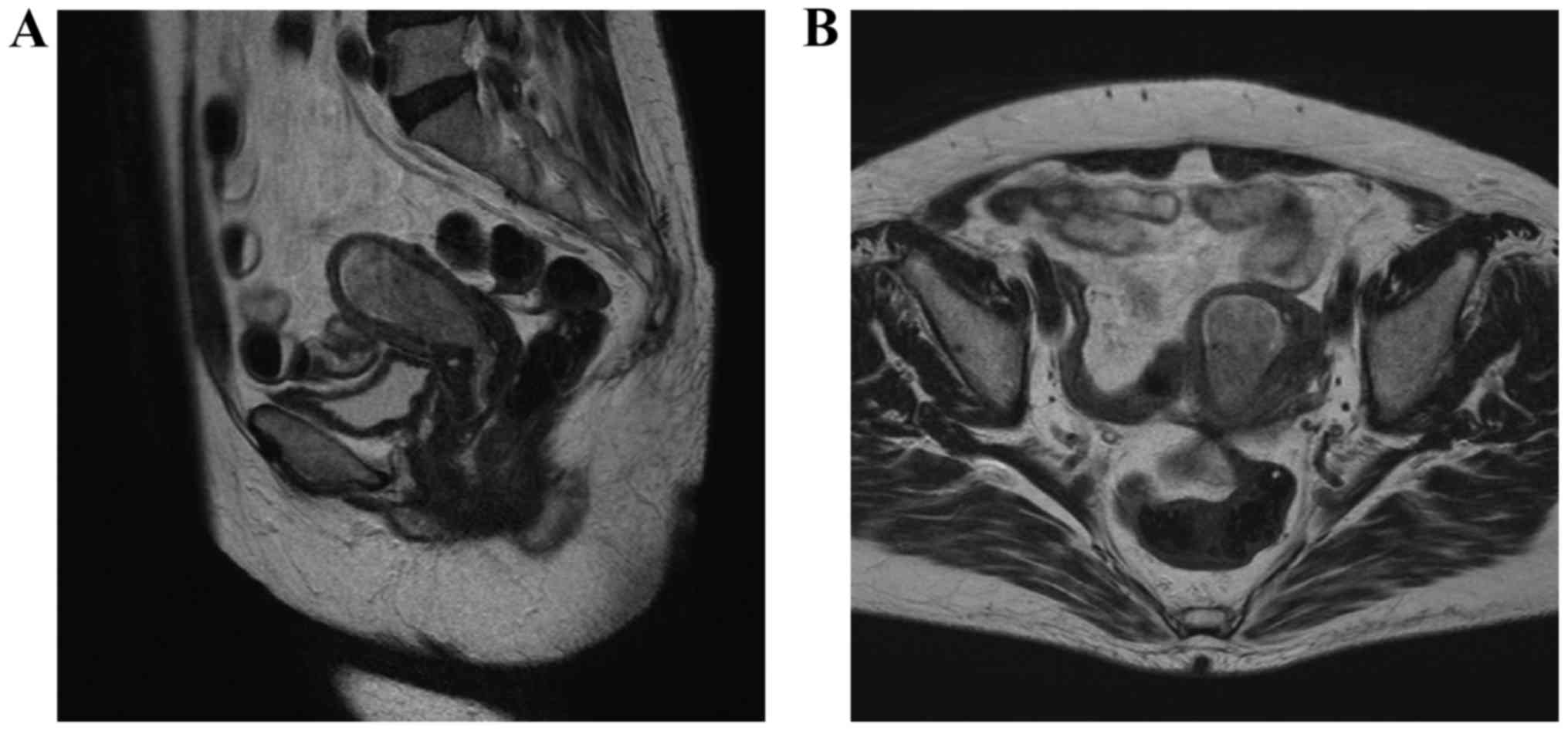
gynecological clinic (September, 2012). Magnetic resonance imaging
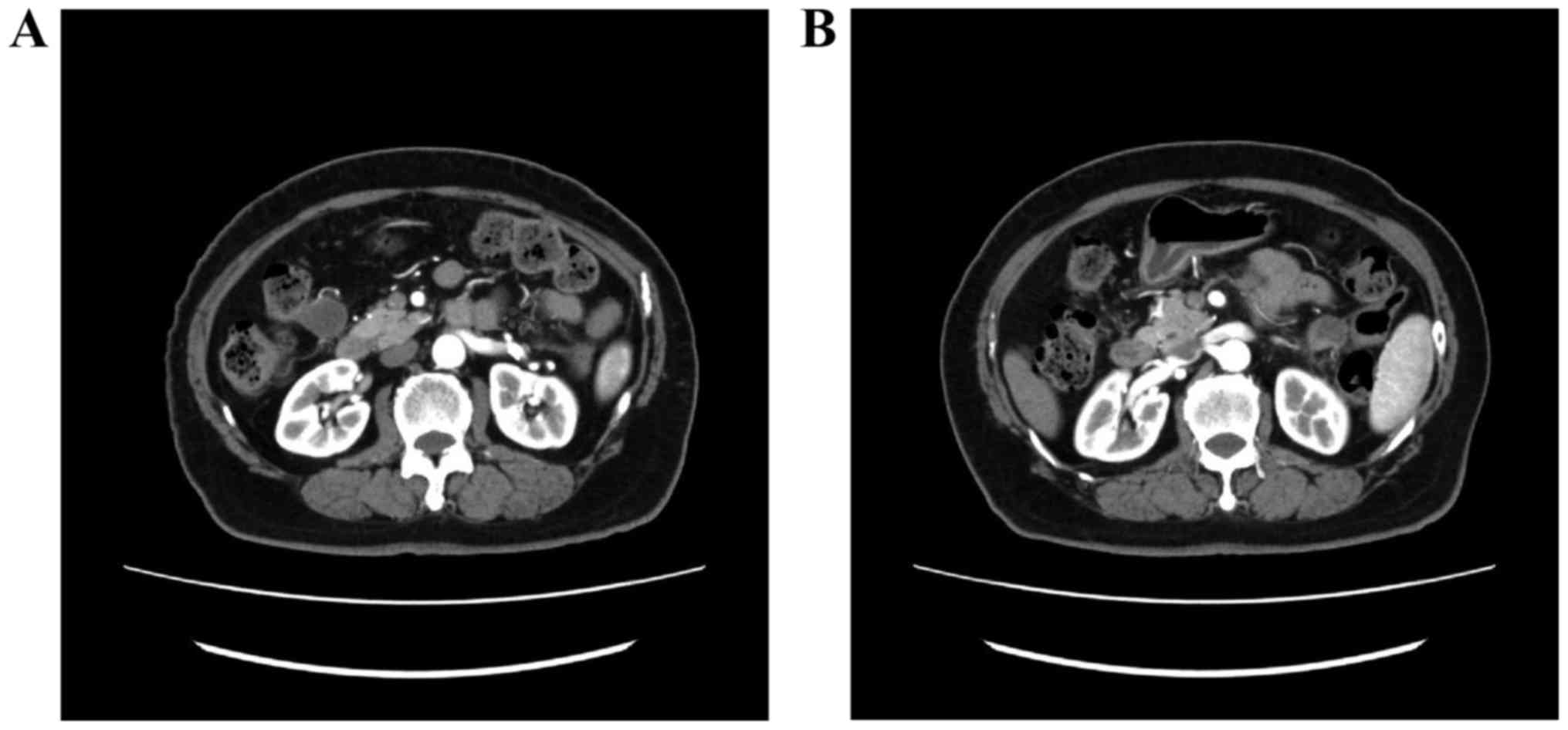
(MRI) revealed a mass sized ~4 cm in the endometrium (Fig. 1) and computed tomography (CT)
revealed two 2-cm peritoneal disseminations (Fig. 2). The carbohydrate antigen-125 level
was 53 ng/ml (normal range, <35 ng/ml), and the carcinoembryonic
antigen level was 8.6 ng/ml (normal range, <5.0 ng/ml). The
diagnosis was endometrial adenocarcinoma. The patient had a history
of type 2 DM and hypertension, but was not obese (body mass index,
23.6 kg/m2). The HbA1c level (National Glycohemoglobin
Standardization Program) was 9.1%, and the patient was treated with
oral medications [sulfonylurea and dipeptidyl peptidase-4 (DPP-4)
inhibitor].
The patient was referred to the Shimane University
Hospital for treatment of the pelvic and abdominal masses, where
she underwent modified radical hysterectomy, bilateral
salpingo-oophorectomy, pelvic lymphadenectomy and abdominal mass
resection. All identifiable masses were resected. Pathological
examination revealed a stage IVB (International Federation of
Gynecology and Obstetrics 2008), pT1aN0M1 endometrial serous
adenocarcinoma.
Although adjuvant chemotherapy was planned, the
postoperative follow-up was complicated by perforation of the
digestive tract and severe inflammation of the peritoneum. To
control glycemia, insulin was initially used, but it was replaced
with metformin (250 mg once a day) and other oral medications
(sulfonylurea and DPP-4 inhibitor) following discharge from the
hospital. No further medical treatment was performed.
After being discharged from the hospital, the
patient did not exhibit elevated levels of tumor markers or any
metastases on CT. At 45 months after the initial metformin
treatment, the patient had no complaints and maintained a good
quality of life, without signs of tumor progression.
Discussion
The mechanism underlying the antitumor effect of
metformin is considered to involve the activation of adenosine
monophosphate-activated protein kinase and inhibition of the
mammalian target of rapamycin, which reduces cell growth (9). Metformin arrests the cell cycle of EC
cells, decreases human telomerase reverse transcriptase mRNA
expression, and inhibits the phosphorylation of S6RP, resulting in
the inhibition of signaling downstream of the mRNA pathway
(10,11). Thus, in EC, cell cycle arrest by
metformin has been observed in vitro, and inhibition of
telomerase activity may be an important mechanism underlying the
antitumor activity of this drug (10).
Clinical evidence on the effect of metformin on EC
outcome is limited to retrospective data and does not generally
account for the effects of multiple covariates, such as pathology,
stage and treatment, on clinical outcome (12). It cannot be definitively concluded
that patients who receive metformin are less likely to succumb to
EC, as metformin may also reduce mortality from other causes (e.g.,
complications of diabetes and cardiovascular disease) (13).
In the present case, adjuvant chemotherapy and
radiotherapy could not be administered, but the patient remained
disease-free over a long period of time with metformin therapy
alone. The contribution of complete surgical resection to this
clinical benefit cannot be ruled out. Moreover, whether this was
the natural course of EC in our patient remains unclear. Despite
these limitations, this clinical case suggests that metformin is
potentially beneficial in the prevention or treatment of EC. This
finding deserves further validation in clinical studies (14–16).
References
|
1
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin 64. 9–29, 2014. Erratum in. CA
Cancer J Clin. 64:3642014. View Article : Google Scholar
|
|
2
|
Zhang Y, Liu Z, Yu X, Zhang X, Lü S, Chen
X and Lü B: The association between metabolic abnormality and
endometrial cancer: A large case-control study in China. Gynecol
Oncol. 117:41–46. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
American Diabetes Association, . Executive
summary: Standards of medical care in diabetes-2014. Diabetes Care.
37:(Suppl 1). S5–S13. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Febbraro T, Lengyel E and Romero IL: Old
drug, new trick: Repurposing metformin for gynecologic cancers?
Gynecol Oncol. 135:614–621. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Stine JE and Bae-Jump V: Metformin and
gynecologic cancers. Obstet Gynecol Surv. 69:477–489. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tan BK, Adya R, Chen J, Lehnert H, Cassia
LJ Sant and Randeva HS: Metformin treatment exerts antiinvasive and
antimetastatic effects in human endometrial carcinoma cells. J Clin
Endocrinol Metab. 96:808–816. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cantrell LA, Zhou C, Mendivil A, Malloy
KM, Gehrig PA and Bae-Jump VL: Metformin is a potent inhibitor of
endometrial cancer cell proliferation-implications for a novel
treatment strategy. Gynecol Oncol. 116:92–98. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ko EM, Walter P, Jackson A, Clark L,
Franasiak J, Bolac C, Havrilesky LJ, Secord AA, Moore DT, Gehrig
PA, et al: Metformin is associated with improved survival in
endometrial cancer. Gynecol Oncol. 132:438–442. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Riedmaier A Emami, Fisel P, Nies AT,
Schaeffeler E and Schwab M: Metformin and cancer: From the old
medicine cabinet to pharmacological pitfalls and prospects. Trends
Pharmacol Sci. 34:126–135. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ben Sahra I, Laurent K, Loubat A,
Giorgetti-Peraldi S, Colosetti P, Auberger P, Tanti JF, Le
Marchand-Brustel Y and Bost F: The antidiabetic drug metformin
exerts an antitumoral effect in vitro and in vivo through a
decrease of cyclin D1 level. Oncogene. 27:3576–3586. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tsuji K, Kisu I, Banno K, Yanokura M, Ueki
A, Masuda K, Kobayashi Y, Yamagami W, Nomura H, Susumu N, et al:
Metformin: A possible drug for treatment of endometrial cancer.
Open J Obstet Gynecol. 2:1–6. 2012. View Article : Google Scholar
|
|
12
|
Al Hilli MM, Bakkum-Gamez JN, Mariani A,
Cliby WA, Mc Gree ME, Weaver AL, Dowdy SC and Podratz KC: The
effect of diabetes and metformin on clinical outcomes is negligible
in risk-adjusted endometrial cancer cohorts. Gynecol Oncol.
140:270–276. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ezewuiro O, Grushko TA, Kocherginsky M,
Habis M, Hurteau JA, Mills KA, Hunn J, Olopade OI, Fleming GF and
Romero IL: Association of Metformin Use with Outcomes in Advanced
Endometrial Cancer Treated with Chemotherapy. PLoS One.
11:e01471452016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Amant F, Moerman P, Neven P, Timmerman D,
Van Limbergen E and Vergote I: Endometrial cancer. Lancet.
366:491–505. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mitsuhashi A, Kiyokawa T, Sato Y and Shozu
M: Effects of metformin on endometrial cancer cell growth in vivo:
A preoperative prospective trial. Cancer. 120:2986–2995. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Indraccolo S, Randon G, Zulato E, Nardin
M, Aliberti C, Pomerri F, Casarin A and Nicoletto MO: Metformin: A
modulator of bevacizumab activity in cancer? A case report. Cancer
Biol Ther. 16:210–214. 2015. View Article : Google Scholar : PubMed/NCBI
|