Introduction
Primary ureteral polyps are rare benign tumors,
comprising <1% of all genitourinary neoplasms (1). The presenting symptoms are vague; thus,
preoperative diagnosis may be difficult. According to a recent
systematic literature review, the median size of these polyps is
4.0 cm (2). However, polyps >15
cm have also been reported, although they are usually found in the
proximal ureter. Due to its rarity, there is no standard treatment
for this disease; however, complete excision is the optimal method
to avoid recurrence. We herein present the case of a patient with a
giant primary ureteral polyp located in the lower part of the
ureter in an older woman, and discuss the diagnostic and
therapeutic measures and related literature.
Case report
A 53-year-old woman was admitted to the Second
Clinical Hospital of North Sichuan Medical College (Nanchong,
China) with gross painless hematuria for ~2 years and frequency of
urination for ~1 month. The physical examination was unremarkable.
Multidetector computed tomography urography (CTU) revealed a
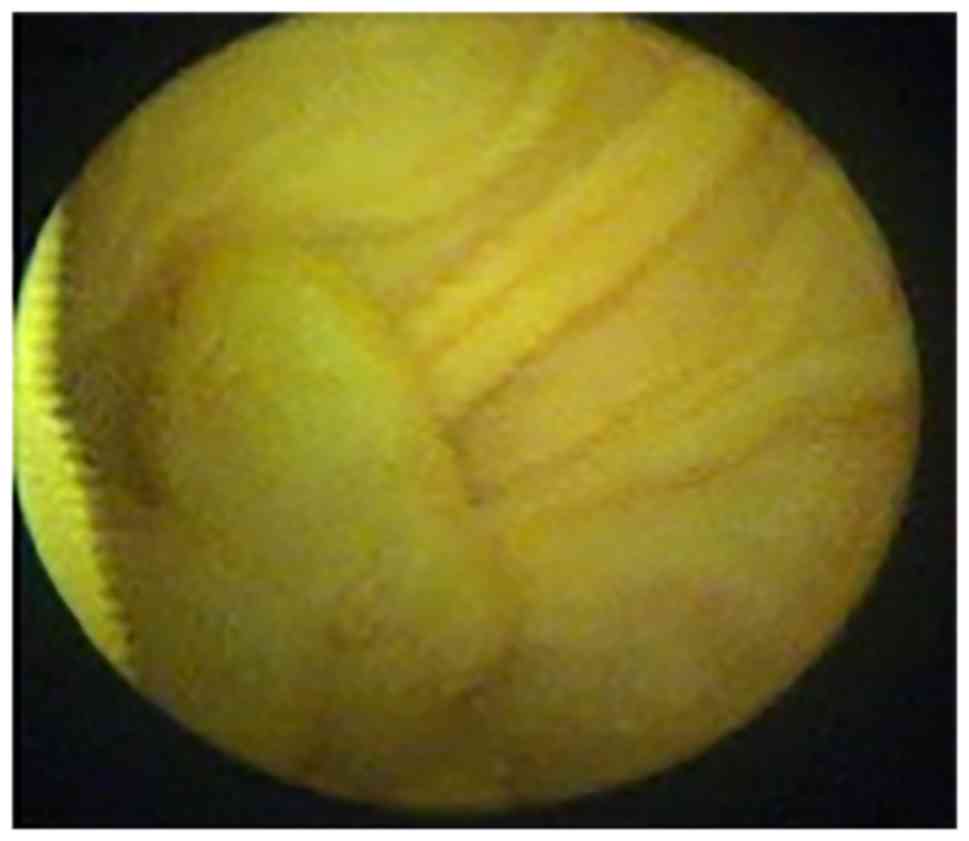
filling defect in the lower part of the right ureter (Fig. 1). Cystoscopy revealed a mass ~3 cm in
length, with a smooth surface, protruding from the ureteral orifice
into the bladder (Fig. 2).
Examination of a bioptic specimen suggested that the mass was an
inflammatory polyp. A 5F ureteral catheter was inserted from the
right ureteral orifice; ~10 cm after the insertion point,
resistance was encountered and the catheter could not be advanced
further. Retrograde urography was subsequently performed and the
contrast media failed to reach the upper part of the ureter and the
renal pelvis, whereas the lower part of the ureter exhibited a
filling defect (Fig. 3).
Ureteroscopic assessment was performed under general
anaesthesia and revealed a pedunculated tumor (~15 cm in length)
arising from the lower segment of the right ureter, with a smooth
surface, with the base of the tumor located ~13 cm from the
ureteral orifice. The tumor macroscopically resembled a long grape.
As we unable to find the upper ureteral orifice, the ureteroscope
and guidewire could not pass through the base of the tumor. A small
piece of tumor was resected by Holmium laser for histopathological
examination and a Double-J stent was inserted, with the upper end
of the stent located in the base of the tumor. Resectoscopy was
then performed to incise the portion of the polyp protruding into
the bladder. The histological examination of these two bioptic
specimens suggested that the tumor was a fibroepithelial polyp.
Kidney-ureter-bladder imaging was then performed, which revealed
that the Double-J stent was folded and twisted in the fifth lumbar
plane (Fig. 4).
Open surgery was employed under general anaesthesia,
Resection of the polyp and the narrow ureteral segment plus
V-shaped end-to-end ureteral anastomosis were performed. An oblique
incision on the right low abdomen was performed. Following exposure
of the ureter, taking the apex of the Double J-tube as the
longitudinal excision sign, the ureter was longitudinally opened
for ~2 cm, the root of the polyp was immediately identified, and
the ureter above the polyp was narrowed. The polyp was cut at the
base and was completely removed from the ureter (Fig. 5); the length of the polyp was ~12 cm
(Fig. 6). Approximately 0.5 cm of
the narrow ureteral segment was resected and end-to-end anastomosis
was performed. A Double-J stent was left in place.
The postoperative histopathological examination
findings revealed that the tumor was a ureteral fibroepithelial
polyp (UFP). The Double-J stent was removed 2 months after the
operation. The patient was asymptomatic, and no complications or
recurrence have occurred during the 12 months of follow-up. gave
their informed consent regarding the publication of the case
details.
Discussion
Primary ureteral tumors are among the rarest in the
spectrum of genitourinary tumors and are most commonly malignant.
Only one-fifth of these tumors are benign and, among those, UFPs
are considered to be the most common. The etiology of benign
ureteral polyps is unclear. They are considered to be the result of
various factors, including congenital (developmental anomaly),
obstruction, trauma, irritation, infection, and specific endogenous
hormonal imbalances (3). The
clinical presentation of primary UFPs is non-specific. They most
commonly present as a single, small polyp. Reports of multiple,
bilateral polyps are extremely rare, whereas the mean diameter of
UFPs was reported to be <5 cm; larger polyps may extend into the
bladder cavity and may be difficult to distinguish from bladder
tumors (4,5). In the majority of the cases, the upper
ureter is the most common site of origin of these tumors, whereas
polyps derived from the lower urinary tract are not as frequent
(6). UFPs most commonly occur
between the second and fourth decades, and they usually originate
from the left ureter. The clinical symptoms are non-specific and
the majority of the early primary UFPs are asymptomatic. Necrosis
and bleeding on the polyp surface may be expressed as gross
hematuria and, when obstruction occurs, hydronephrosis or renal
colic may develop. In the present case, the polyp occurred in the
lower part of the right ureter in a middle-aged woman; in addition,
it was broad-based and had a total length of ~15 cm (portion
removed by open surgery, ~12cm; and ureteroscopically removed
bladder part, ~3 cm). Previous reports of such lower-segment
ureteral giant primary UFPs are extremely rare.
Imaging examination (7) may be helpful and suggestive of a UFP
diagnosis. Intravenous pyelography or CTU may show a filling
defect, thereby hinting at the state of the renal function of the
patient, and may also reveal whether hydronephrosis may be present.
However, preoperative radiographic diagnosis may be challenging, as
UFPs usually present as a filling defect, which may be attributed
to blood clots, radiolucent calculi, neoplasms or a crossing
vessel. Moreover, it may be difficult to differentiate UFPs from
transitional cell carcinoma based only on imaging findings
(8), as preoperative diagnosis
confirmation is difficult and Li et al reported in 2014 that
none of the UFPs in their study were detected prior to surgery
(9). Mistaking these tumors for
transitional cell carcinomas may result in unnecessary
nephroureterectomy.
For patients with suspected UFPs who have been
evaluated by intravenous pyelography, CT, or retrograde urography,
a ureteroscopic examination is also required to confirm the
diagnosis. Ureteroscopy may be attempted to obtain a diagnosis and
determine the optimal treatment approach. Prior to ureteroscopy
becoming widespread, differentiating malignant from benign lesions
was difficult. The number of polyps, the diameter of the base and
the location of the obstruction may be determined through
ureteroscopy in the same session; ureteroscopic biopsy of the
lesion may be performed for larger tumors, whereas smaller tumors
may be completely resected during ureteroscopy, thus avoiding a
second surgery. In the present case, preoperative ureteroscopic
examination revealed that the polyp was extremely long, originated
from the lower part of the ureter and its base was wide; the biopsy
result revealed a benign fibroepithelial polyp, and surgical
resection was selected. At the same time, a Double-J stent was also
placed at the obstruction site, which was identified by searching
the base of the polyp during open surgery.
The management of UFPs currently depends on the
site, size and clinical expertise. Smaller lesions may simply be
fulgurated endoscopically, while larger lesions require proper
surgical excision. With the advent of new technology, minimally
invasive techniques have become popular. Previous reports have
described successful polypectomy through the use of ureteroscopy
and endoscopic treatment (5,10). However, ureteroscopy and endoscopic
resection may be difficult in patients with long or large polypoid
lesions, due to poor visualization of the base of the stalk and
limited working space, which make it difficult to differentiate the
ureteral wall from the polyp, leading to incomplete resection or
ureteral perforation. Laparoscopic surgery is another minimally
invasive method (11,12). Successful laparoscopic treatment has
been described in patients with large, long polyps, as well as in
those with multiple polyps. Kijvikai et al (13) described the transperitoneal
laparoscopic management of a 17-cm long fibroepithelial polyp in
the proximal ureter associated with ureteral obstruction. However,
this approach may not be suitable for polyps in the lower part of
the ureter, particularly in cases without hydronephrosis, and
laparoscopic surgery may cause difficulties in ureteral anastomosis
following ureteral resection, particularly in patients with a lower
ureteral polyp. Complete resection is considered the optimal method
for avoiding recurrence of UFPs, as incomplete resection may result
in recurrence. In our case, as the polyp was long, its stalk could
not be fully visualized via ureterorenoscopy; furthermore, it
occurred in an older woman and originated from the lower part of
the ureter. Our main objective was to ensure complete resection, so
open surgery was selected in this case. A small ureteral segment
was resected, including the narrowed potion of the ureter and the
entire stalk of the polyp, followed by end-to-end ureteral
anastomosis.
In summary, an extremely long pedunculated UFP of
the distal ureter, which protruded into the bladder, was excised
via open surgery. Pedunculated urothelial polyps originating from
the ureter should be taken into consideration in the differential
diagnosis of a bladder mass on imaging. Primary ureteral polyps are
benign and the prognosis is usually good. Ureteroscopy is not only
a useful diagnostic method, but may also be an effective treatment
for smaller, solitary ureteral polyps. For larger polyps, in
patients with obstruction, ureteroscopy may help determine the
polyp size, its location, the location of the ureteral stenosis, as
well as the base of the polyp, which may help determine the optimal
surgical approach.
Acknowledgements
The authors would like to thank Anguo Wang for
assisting with the surgical procedure. This study was supported by
the North Sichuan Medical College (grant no. 20131252).
References
|
1
|
Piovesan AC, Torricelli FC, Borges LL,
Chambô JL, Mesquita JL and Srougi M: Ureteral fibroepithelial
polyps in a pregnant woman: Case report. Sao Paulo Med J.
127:238–240. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ludwig DJ, Buddingh KT, Kums JJM, Kropman
RF, Roshani H and Hirdes WH: Treatment and outcome of
fibroepithelial ureteral polyps: A systematic literature review.
Can Urol Assoc J. 9:E631–E637. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ye L, Zhao LJ, Yue F, Song XS, Wei W,
Jiang XJ and Yang JY: Large ureteral fibroepithelial polyp lacking
epithelium due to ischemic infarction. Kaohsiung J Med Sci.
28:457–461. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kaba M, Kaba S, Kaya TY, Eren H and
Pirincci N: A giant pedunculated urothelial polyp imicking bladder
mass in a child: a rare case. Case Rep Pediatr 2014. 2014.1–3.
View Article : Google Scholar
|
|
5
|
Liu C, Liu XJ, Liu D and Yao DW: A giant
ureteral polyp mimicking as a bladder mass resected
ureteroscopically by diode laser: A case report and literature
review. Int J Clin Exp Pathol. 8:14580–14583. 2015.PubMed/NCBI
|
|
6
|
Childs MA, Umbreit EC, Krambeck AE, Sebo
TJ, Patterson DE and Gettman MT: Fibroepithelial polyps of the
ureter: A single-institutional experience. J Endourol.
23:1415–1419. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xu C, Zhang Z, Ye H, Wu C, Zhang C, Zhang
Y, Wang Y, Cao Z, Wang H, Xu W, et al: Imaging diagnosis and
endoscopic treatment for ureteral fibroepithelial polyp prolapsing
into the bladder. J Xray Sci Technol. 21:393–399. 2013.PubMed/NCBI
|
|
8
|
Patheyar V, Venkatesh SK, Siew EP,
Consiglieri DT and Putti T: MR imaging features of fibroepithelial
ureteral polyp in a patient with duplicated upper urinary tract.
Singapore Med J. 52:e45–e47. 2011.PubMed/NCBI
|
|
9
|
Li R, Lightfoot M, Alsyouf M, Nicolay L,
Baldwin DD and Chamberlin DA: Diagnosis and management of ureteral
fibroepithelial polyps in children: A new treatment algorithm. J
Pediatr Urol. 11:22.e1–22.e6. 2015. View Article : Google Scholar
|
|
10
|
Hubosky SG and Bagley DH: Laser Resection
of Fibroepithelial Polyps with Digital Ureteroscopy. J Endourol
Case Rep. 1:36–38. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dai LN, Chen CD, Lin XK, Wang YB, Xia LG,
Liu P, Chen XM and Li ZR: Retroperitoneal laparoscopy management
for ureteral fibroepithelial polyps causing hydronephrosis in
children: A report of five cases. J Pediatr Urol. 11:257.e1–257.e5.
2015. View Article : Google Scholar
|
|
12
|
Bian Z, Liu X, Hua Y, Liu F, Lin T and He
D: Laparoscopic management of multiple ureteral polyps in children.
J Urol. 186:1444–1449. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kijvikai K, Maynes LJ and Herrell SD:
Laparoscopic management of large ureteral fibroepithelial polyp.
Urology. 70:3732007. View Article : Google Scholar : PubMed/NCBI
|