Introduction
Primary mesenteric adenocarcinoma (PMA) is a rare
type of malignant tumor. A previous study has presented a case of
embryonal carcinoma originating in the mesentery (1). A further case study reported on poorly
differentiated adenocarcinoma of unknown primary site detected by
mesenteric abscess formation (2).
The present case study reports on a case of PMA that was covered by
an abscess of the mesocolon, and had the complication of intestinal
obstruction. The clinical data of the case are presented, the
relevant literature has been reviewed, and the management of PMA is
discussed.
Case report
First admission
A 49-year-old male patient was admitted to the
Affiliated Hospital of North Sichuan Medical College (Nanchong,
China) in February 2015 due to abdominal pain for >7 months,
aggravated by nausea and no defecation for 6 days. Physical
examination revealed a tenderness in the left side of the abdomen
with bowel sound hyperfunction, and a digital rectal examination
did not reveal any abnormalities. The white blood cell count was
12.96×109/l. Analysis of tumor markers showed that the
levels of carcinoembryonic antigen (CEA) and carbohydrate antigen
(CA)19-9 were 14.33 µg/l (normal, 0–5 µg/l) and 757.1 U/ml (normal,
0–37 U/ml), respectively. An abdominal X-ray plain film revealed
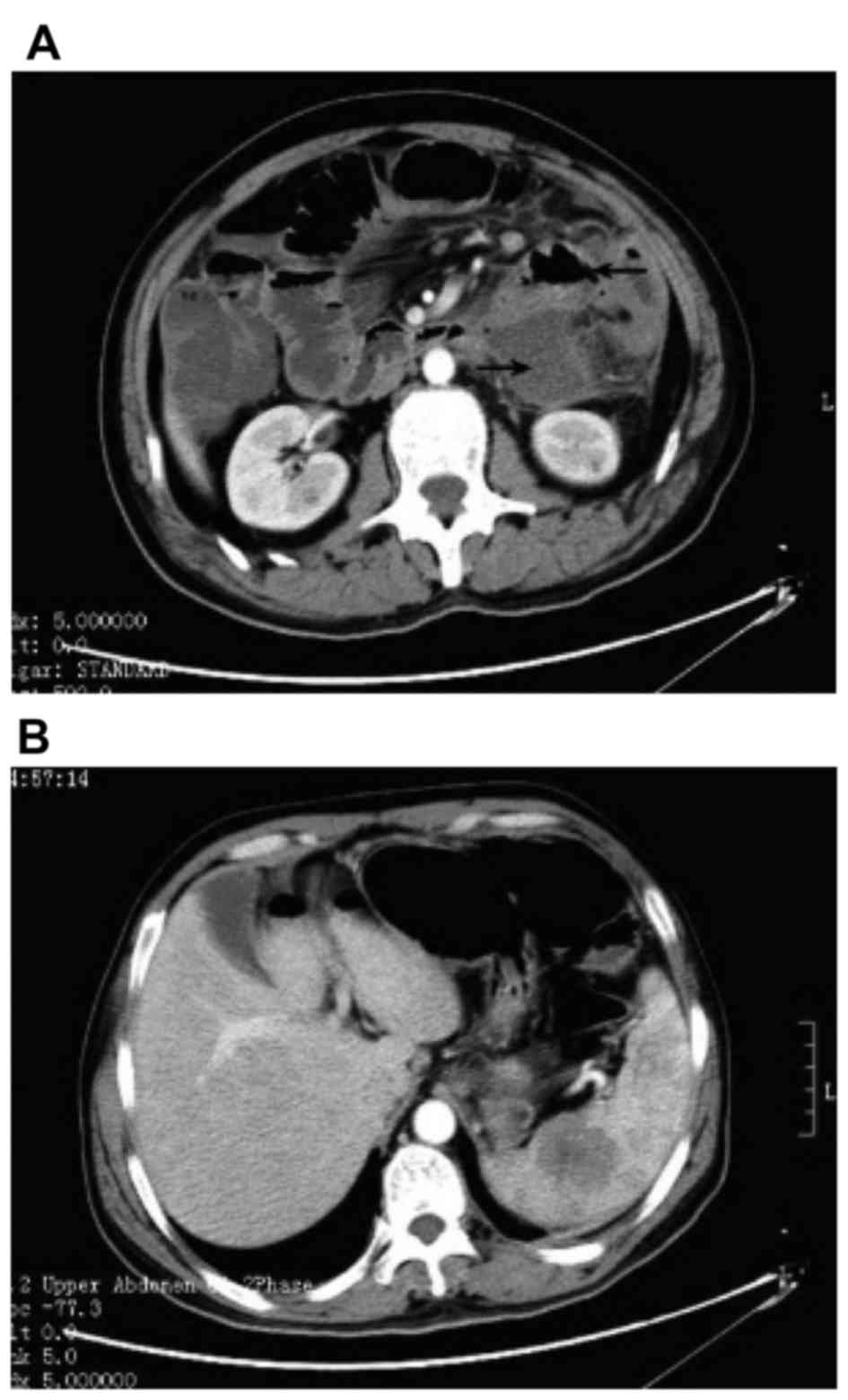
intestinal obstruction (Fig. 1), and
a computed tomography (CT) scan of the abdomen revealed an
incomplete ileus (Fig. 2A) and
low-density lesions in the spleen (Fig.
2B). The preliminary diagnosis of acute complete intestinal
obstruction, and possibly of gastrointestinal carcinoma, was
considered. Upon laparotomy, an abscess of the mesocolon of ~6×5×4
cm in size was found below the splenic flexure of the colon, the
transverse colon was expanded and the regions surrounding the
intestinal wall had a lot of pus associated with edema. The left
colon mesentery with surrounding tissue adhesion showed hyperemia,
edema and hardness. After the abscess was resected, 20 ml pus was
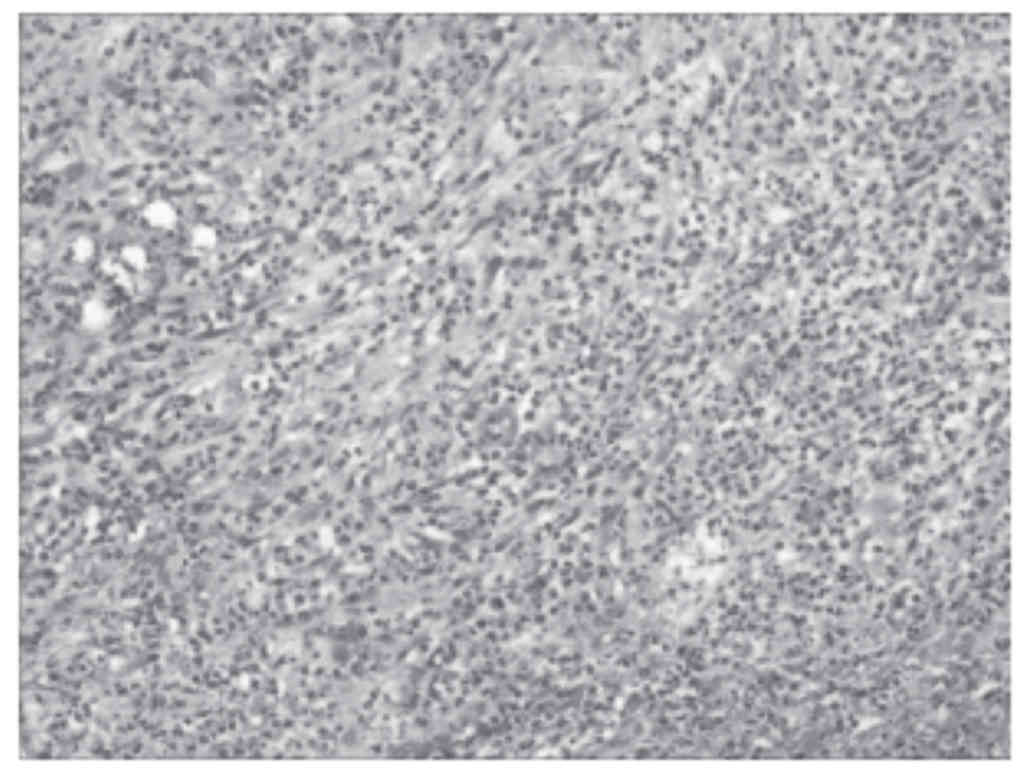
obtained for bacterial culture and drug sensitivity testing. Biopsy
of the full thickness of the abscess base and a qualitative biopsy
of the hard mesentery revealed acute gangrenous inflammation
(Fig. 3). Terminal ileum colostomy
was subsequently performed, following which the patient recovered
well after fighting infection and symptomatic treatment.
Specifically, the infection was treated with Cefotiam antibiotics,
and after 6 days of anti-infection treatment with Cefotiam, the
patient's condition gradually improved; he was discharged from
hospital after recovery.
Second admission
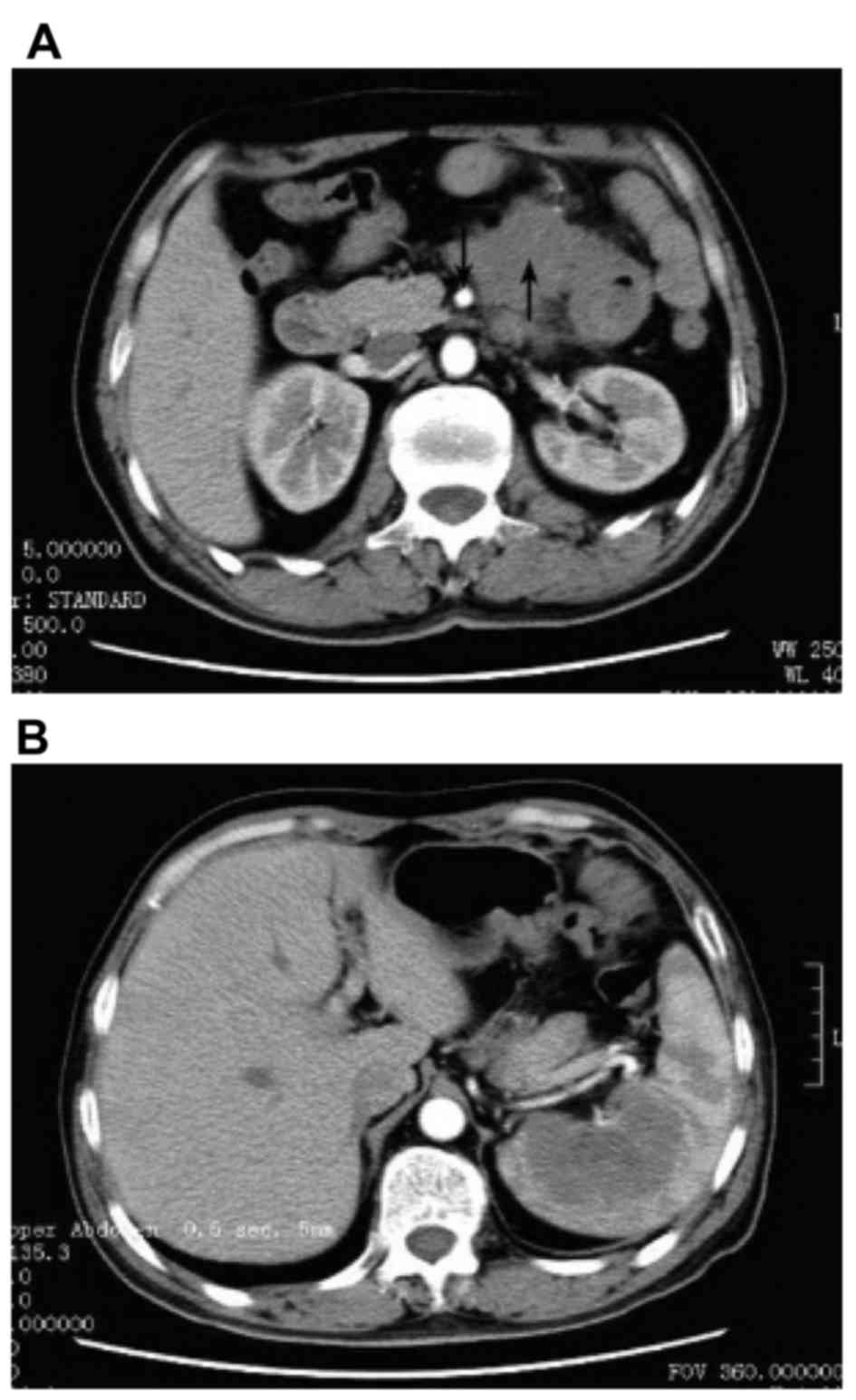
The patient was admitted to hospital again in
September 2015 due to ileum colostomy closure. The serum
concentrations of CEA and CA19-9 were elevated (49.44 µg/l and
2,569 U/ml, respectively), and compared with that on first
admission, the CT scan showed that the left side of the abdomen
featured an irregular soft-tissue shadow (Fig. 4A) and the shadow of the lesions of
the spleen was significantly increased (Fig. 4B). A second laparotomy was performed.
Pale yellow ascites (~100 ml) were obtained. A mesenteric solid
tumor of the colon of ~8×6×6 cm in size was present near the left
side of the superior mesenteric artery root, and the tumor, with
qualitative hardness (hard texture), poor activity and unclear
boundaries, infiltrated areas including the surrounding mesenteric
vessels, small intestine and transverse colon. A hard mass with a
diameter of ~6 cm was palpitated in the spleen. There were no
abnormal findings in the gastrointestinal tract, liver, pancreas,
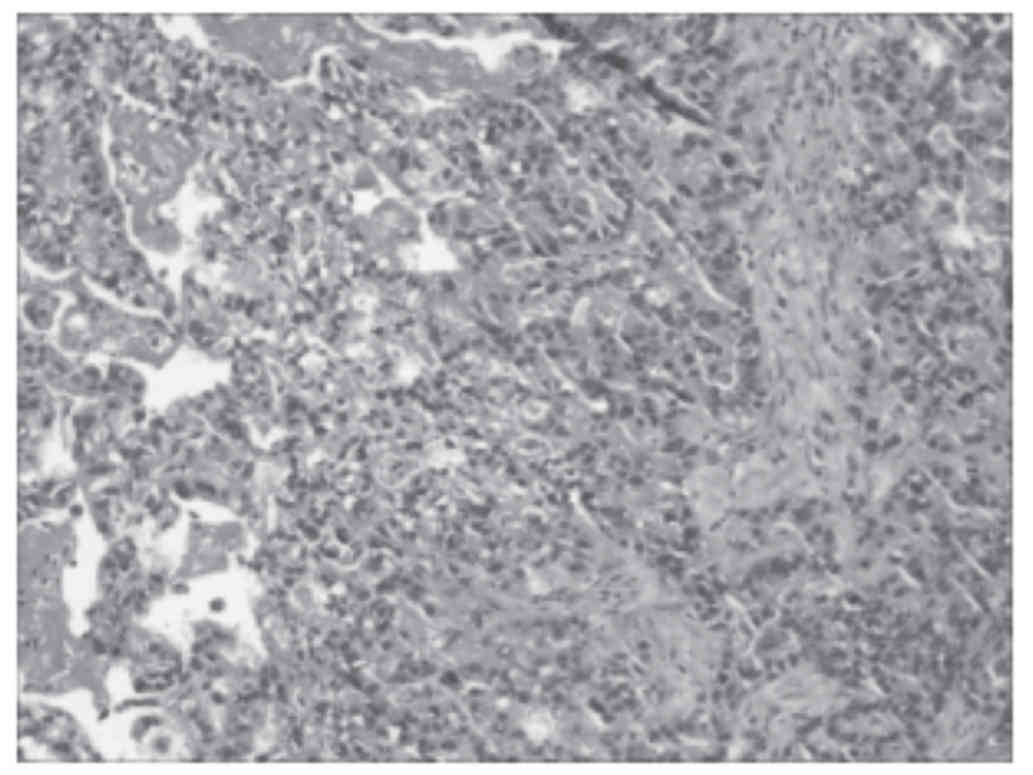
kidney and other organs. Three tissue samples of ~0.5×0.5×0.5 cm in
size from different parts of the mesenteric tumor were used for
diagnosis based on intraoperative frozen section analysis, which
revealed adenocarcinoma (Fig. 5).
Owing to the difficulties in resecting the tumor, no further
surgery was performed on the patient following communication with
his family. During the 3 months of follow-up, the patient did not
receive any adjuvant chemotherapy and his cancer cachexia
worsened.
Discussion
Primary mesenteric tumors (PMT) are encountered in
~l/10,000-1/25,000 of the total number of hospitalized patients. In
patients with PMT, the cystic/solid ratio was reported to be 2:1
and the former type was more common for benign tumors, while the
latter type was mainly encountered in malignant cases (3). The World Health Organization lists 34
different pathological classifications for PMT, among which
adenocarcinoma is a rare type. The present study reported on a
unique and rare case of PMA, which was covered by an abscess of the
mesocolon and featured intestinal obstruction.
As the onset site of PMT is often obscured or
hidden, patients in the early stage have no clinical symptoms. Only
when the tumor size is sufficiently large for it to burst or to
exert effects including bowel compression or torsion of the
mesentery, may it induce intestinal obstruction, perforation,
bleeding, volvulus and secondary abdominal infections. Therefore,
patients with clinical symptoms have reached the advanced stage
with a pre-operative diagnosis rate of only 9.38–40.2% (4). CT, ultrasound and other imaging
techniques are able to provide a reference for tumor shape, size,
borders, bleeding, breakage and metastasis. However, the clinical
features of patients with PMT are complex. In CT images, tumors
with certain characteristics can be identified prior to surgery,
while other non-specific tumors can only be diagnosed by
intraoperative frozen or post-operative pathological examination
(5). At the first laparotomy of the
present case, only an abscess of the mesocolon near the splenic
flexure was identified, in which acute gangrenous inflammation was
confirmed by biopsy. Abdominal abscesses concomitant with malignant
tumors are more common in patients with gastrointestinal cancer
associated with chronic perforation (6,7);
however, in the present case, no gastrointestinal tumor was
present. Finally, the patient was diagnosed with an abscess of the
mesocolon and intestinal obstruction, while PMA was overseen.
The pre-operative diagnosis of PMT is often
challenging and affected patients are easily misdiagnosed for the
following reasons: First, patients at early stages do not have any
specific clinical symptoms. Furthermore, CT and other auxiliary
examinations can localize the tumor, but cannot provide any
qualitative diagnosis. When PMT invades or adheres to adjacent
structures, unclear tumor boundaries may reduce the accuracy of CT
localization and obstruct diagnosis. In addition, PMT is rare and
clinicians are often not sufficiently aware of the disease.
Finally, clinicians may be contented with the diagnosis of
complications or comorbidities, and ignore PMT as the fundamental
cause. In the present case, the patient with acute abdominal
manifestation of intestinal obstruction was admitted, the
pre-operative leucocyte count and tumor marker levels were high, CT
indicated intestinal obstruction, and the intraoperative diagnosis
was an abscess of the mesocolon with pathological examination
revealing inflammation. As concomitant diseases were more apparent,
the diagnosis of PMT was not considered.
Surgical resection is predominant as the most
effective method for the treatment of PMT, with resection rates of
benign and malignant tumors of 81.9 and 55.0%, respectively. Most
malignant tumors are located in the root of the mesentery and
infiltrate major mesenteric blood vessels (8), which is the main reason for the low
resection rates of malignant PMT. To predict whether patients with
PMT may benefit from adjuvant radiation and chemotherapy, factors
including the degree of malignancy, histological type and age may
be considered.
In conclusion, the present study presented a rare
and unique case of PMA, which was covered and misdiagnosed as an
abscess of the mesocolon and intestinal obstruction. An increased
understanding of PMT among clinicians may reduce the rate of
misdiagnosis of PMT. When a patient is suspected of having
malignancies, and gastrointestinal cancer and other malignancies of
the digestive organs may be excluded, the possibility of PMA should
be considered.
References
|
1
|
Ohshima T, Imada T, Nozawa A, Rino Y and
Takanasi Y: A case of primary mesenteric embryonal carcinoma.
Hepatogastroenterology. 51:983–986. 2004.PubMed/NCBI
|
|
2
|
Yamagata Y, Ando Y, Matsusaka K, Karube H,
Onoyama H, Aikou S, Yamashita H, Mori K, Nomura S, Fukayama M and
Seto Y: Poorly differentiated mesenteric carcinoma of unknown
primary site detected by abscess formation: Case report. World J
Surg Oncol. 12:42014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shao-Yun C, Shi-De L and Hong X: The
diagnosis and treatment of primary mesenteric tumor. Progr Mod
Biomed. 7:1182–1183. 2007.
|
|
4
|
Cheng L: Diagnosis and treatment of
primary intestinal mesentery tumor. Chin J Gen Surg. 13:395–396.
2004.
|
|
5
|
Cuiping Z, Wenfeng Z, Mingwei L, Zhihun Y
and Danling N: CT findings of primary mesenteric tumors. J Clin
Radiol. 31:1131–1134. 2012.
|
|
6
|
Chen HS and Sheen-Chen SM: Obstruction and
perforation in colorectal adenocarcinoma: An analysis of prognosis
and current trends. Surgery. 127:370–376. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Alcobendas F, Jorba R, Poves I, Busquets
J, Engel A and Jaurrieta E: Perforated colonic cancer. Evolution
and prognosis. Rev Esp Enferm Dig. 92:326–333. 2000.PubMed/NCBI
|
|
8
|
Ru Z: Research and progress of primary
intestinal mesentery tumor. Med Rev. 8:278–279. 2002.
|