Introduction
Radiation therapy (RT) and concomitant
chemoradiotherapy (CHRT) in patients with head and neck cancer
(HNC) are commonly associated with complications such as mucositis
and dermatitis in the oral cavity and on the cervicofacial area.
Clinically, these adverse effects are able to cause severe pain and
odinophagia, increase the risk of infections, skin wounds and
inflammatory ulcers, limit deglutition, cause malnutrition and
negatively impact the diet and overall quality of life of patients
(1). The incidence rate of mucositis
varies between 85 and 100%, depending on the cancer treatment
regimen, with altered fractionated RT, CHRT or conventional RT
(2,3), whereas the incidence of acute
dermatitis varies between 7 and 25% (4,5),
reaching up to 49% in patients receiving RT in combination with
cetuximab (6).
Numerous efforts have been made to identify
effective agents for preventing and treating mucositis and
dermatitis induced by RT or CHRT. Although some standard guidelines
for management are available (7,8),
reliable and effective treatments are lacking (9). For mucositis, intensive oral care
protocols, antimicrobial agents, anti-inflammatory agents,
cytoprotective agents, recombinant keratinocyte growth factor-1,
nutritional supplements, biostimulant agents or natural and
homeopathic agents have been described (10–13). On
the other hand, several topical or systemic formulations have been
tried for dermatitis, all of them with ineffective results
(5,6). The ultimate goal of these treatments is
to allow patients to receive complete radiation doses while
improving their quality of life, as well as avoiding unplanned
discontinuation of treatments with a subsequent negative impact on
the final outcome.
Glutamine is a free primary amino acid precursor for
protein synthesis, involved in cell replication for rapid cell
turnover, primarily in the gastrointestinal mucosa and immune
system. In circumstances of intense catabolism and stress, this
organic molecule becomes indispensable as its production demand
exceeds the capacity of endogenous synthesis (14). In addition, patients with HNC often
have a glutamine deficit accentuated by the side effects of RT or
CHRT (15).
Since the first study by Skubitz and Anderson
(16) in 1996 on the role of
glutamine for the prevention and treatment of oral mucositis in
cancer treatments, a number of studies have demonstrated that
supplementation of this amino acid may reduce the incidence and
severity of mucositis during treatment by reversing cellular damage
and improving cellular recovery (17). Certain studies with animal models
indicated that glutamine supplementation was safe and reduced
cytotoxicity-induced mucositis (18,19).
However, others have found no conclusive outcomes, and pointed out
that more studies with higher consistency and methodological
validity were needed to find more solid evidence (7). The aim of this prospective study was to
determine whether oral glutamine administration was effective in
reducing the incidence and severity of oral mucositis and
cervicofacial dermatitis induced by RT or CHRT in patients with
HNC.
Patients and methods
Patients
Patients in this trial were recruited from the
Puerta del Mar University Hospital (Cadiz, Spain) between July 2010
and June 2012. The following inclusion criteria were applied:
Patients with primary cancer in any head and neck location with a
proven malignant biopsy, undergoing RT with or without concomitant
CHRT, and 0 and I performance status grade according to ECOG
(Eastern Cooperative Oncology Group Performance Status). The
exclusion criteria were: Patients with a previous history of
receiving RT, uncontrolled systemic or disseminated disease,
presence of synchronous double malignant tumor, hypersensitivity or
allergy to any of the components included in the study,
uncontrolled diabetes, severe kidney or liver failure, skin
diseases or autoimmune diseases.
Study design
The current study was a phase II randomized
double-blind controlled study. The eligible participants were
randomized into a control group or an experimental group to receive
daily administration of oral glutamine or placebo for assessment of
its efficacy in the management of mucositis and dermatitis
following RT or concomitant CHRT. A randomization in 5 blocks of 10
patients with 1-to-1 assignment to groups was computer-generated by
a statistician who was not working with the patients. These
allocations were placed in sealed masked envelopes with a specific
number group or an experimental group to receive a daily
administration of oral glutamine or placebo. The study protocol was
approved by the Ethics Committee of the Puerta del Mar University
Hospital, Cadiz, Spain and by the Spanish Agency for Drugs and
Health Products (number of trial registry 2009-018103-40). All
patients gave written informed consent to participate.
According to the institutional protocol, the total
radiation dose was fixed to 70 Gy in 35 fractions of 2 Gy, or 66 Gy
in 30–33 fractions of 2 Gy in postoperative RT. Depending on the
case, patients received cisplatin (100 mg/m2) or
cetuximab (400 mg/m2) based on renal function and the
presence of systemic complications. During the study, each patient
received three daily bags to be dissolved in a glass of water
(orally, distributed in the three meals), containing either 10 g of
maltodextrin as the placebo (control group) or 10 g of L-Glutamine
as the treatment (experimental group). Both supplements were
prepared by Nutricion Medica S.L. Laboratories (Madrid, Spain) in
powder form packaged in single dosage pouches indistinguishable
from each other, thus ensuring double-blind masking. The patients
were evaluated by the same observer at the 3rd and 6th weeks during
the treatment protocol, and at the 1st and 6th months
post-treatment. All patients had completed dental and oral
examination prior to treatment, and underwent oral care. For
symptomatic mucositis, oral paracetamol tablets 500 mg or tramadol
100 mg were administered according to the severity of pain. The
need for painkillers, adverse events associated with the study
drugs and patient non-adherence to treatment were recorded.
Endpoints and measures
The primary endpoint was the appearance of clinical
oral mucositis at the 6th week after treatment. Secondary endpoints
included evaluation of functional mucositis, onset of mucositis,
cervicofacial dermatitis, pain and weight loss. Oral mucositis and
cervicofacial dermatitis were assessed according to the Common
Terminology Criteria for Adverse Events version 3.0 (CTCAE v3.0).
Clinical mucositis was graded from grade 0 (no mucositis) to grade
4 (symptomatic associated with life threatening consequences,
tissue necrosis, significant spontaneous bleeding). Functional
mucositis was evaluated from grade 0 (no mucositis) to grade 4
(symptoms associated with life-threatening consequences).
Dermatitis on the cervicofacial area was assessed from grade 1
(faint erythema or dry desquamation) to grade 4 (skin necrosis or
ulceration of full thickness of dermis; spontaneous bleeding from
involved site). Data regarding pain were collected using a visual
analog scale (VAS) from 0 (‘no pain’) to 10 (‘insupportable pain’).
Evaluation of treatment tolerance was based on occurrence of
adverse events during the trial. Patients fulfilled the quality of
life questionnaire of the M.D. Anderson Symptom Inventory-Head and
Neck (MDASI-HN), comprising 3 subscales: 13 items that rated the
severity of general symptoms associated with cancer, 9 HNC-specific
items that rated the severity of symptoms particularly associated
with HNC and 6 items that assessed how severely symptoms interfered
with daily activities. The core and HNC-specific symptoms were
rated on a 0–10 scale to indicate the presence and severity of the
symptom, with 0 indicating ‘not present’ and 10 indicating ‘as bad
as you can imagine.’
Statistical analysis
The sample size was calculated according to an
expected clinical mucositis appearance of 100% at the 6th month.
Expecting to find a reduction of 75% after prescribing glutamine (δ
value of 25%), a 5% α error and an 80% β value (study power) were
selected, assuming a 5% loss. With these data, the necessary number
of participants to obtain statistical significance was 50 patients
(25 per group). Intention to treat and per protocol analyses were
performed on the population.
The results were analyzed using the SPSS version
15.0 (IBM Corp., Chicago, IL, USA). All statistical tests achieved
a significance level of P<0.05 for a bilateral significance. The
baseline characteristics of groups were compared using analysis of
variance for continuous variables. In the case of discrete
variables, the distribution of absolute frequencies and percentages
were obtained. Discrete variables were compared using the
χ2 statistic, and continuous variables using the
Student's t-test. Comparisons between the two groups were performed
using analysis of covariance. The results of VAS scores were
presented as the mean, median and standard deviation.
Results
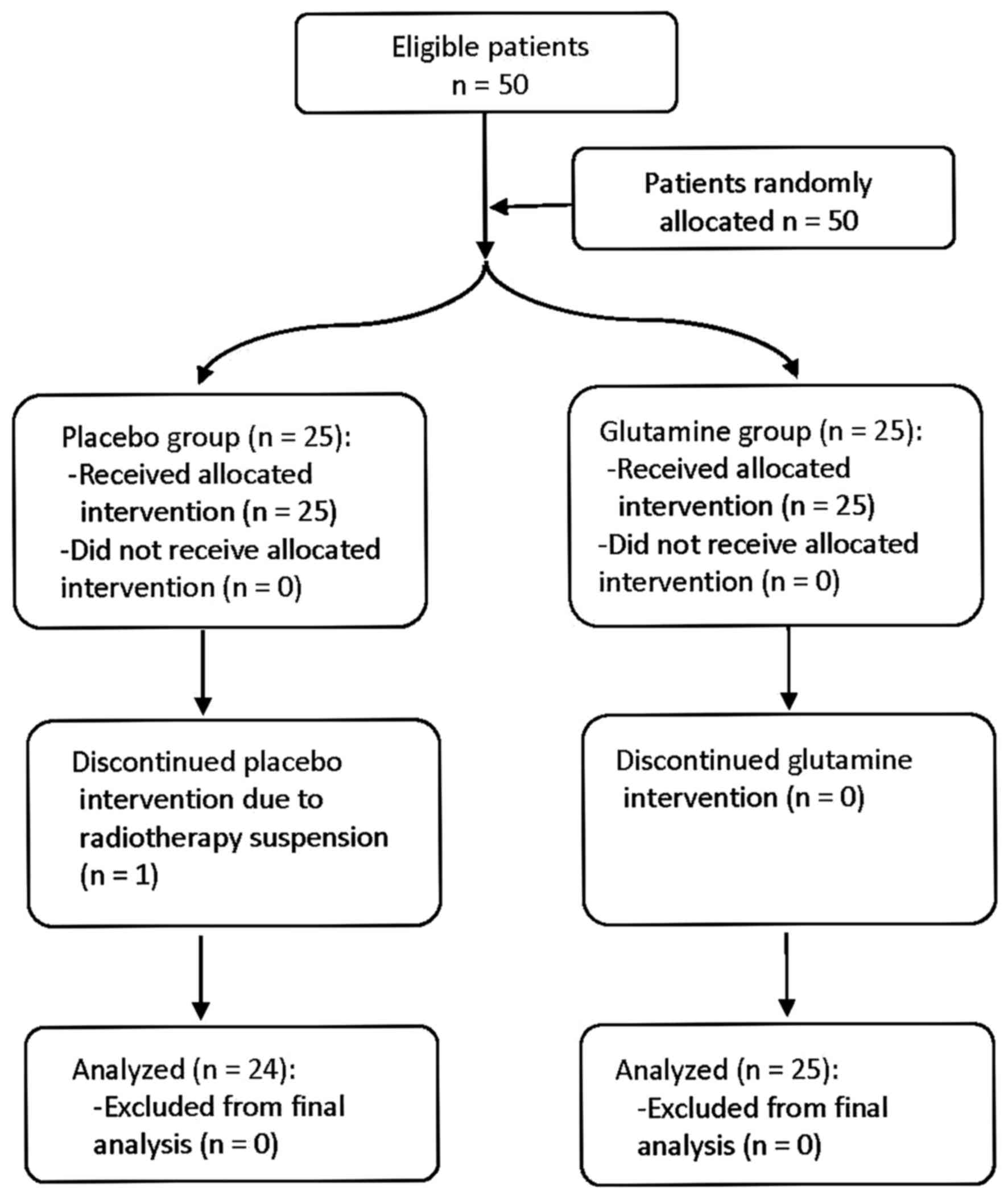
Fifty patients between 32 and 79 years of age (mean,
60.24) were included in the intention to treat analysis, 78% were
male and 22% were female. One female dropped out due to RT
suspension. As a result, 24 patients in the control group and 25
patients in the experimental group were included in the full per
protocol analysis (Fig. 1). On
conducting the statistical analysis, the intention to treat
analysis and per protocol analysis produced identical results for
all criterion measures; therefore, only the per protocol analysis
was used to describe the results.
The distribution of patients according to baseline
patient characteristics, diagnostic and treatment parameters were
similar between the study groups (Table
I). In total, 45% of patients received RT and 55% concomitant
CHRT. The dose of radiation was 70 Gy in 91.8% of patients and 66
Gy in 8.2%. Cisplatin and cetuximab was indicated in 13 and 14
patients, respectively; 63.3% of patients had previously underwent
surgery.
 | Table I.Baseline patient characteristics and
diagnostic parameters. |
Table I.
Baseline patient characteristics and
diagnostic parameters.
|
| Placebo group
(n=25) | % | Glutamine group
(n=25) | % | P-value |
|---|
| Sex | 0.496 |
| Male | 20 | 80 | 18 | 72 |
|
|
Female | 5 | 20 | 7 | 28 |
|
| Median age,
years | 61.5 (32–81) |
| 59. (39–78) |
| 0.432 |
| Tobacco use | 0.358 |
| No
smoker | 6 | 24 | 7 | 28 |
|
| <20
cigarettes | 5 | 20 | 1 | 4 |
|
| 20–40
cigarettes | 6 | 24 | 7 | 28 |
|
| >40
cigarettes | 2 | 8 | 5 | 20 |
|
|
Ex-smoker | 5 | 20 | 5 | 20 |
|
| Alcohol | 0.368 |
| No | 11 | 44 | 10 | 40 |
|
| Yes | 12 | 48 | 11 | 44 |
|
|
Ex-alcoholic | 2 | 8 | 4 | 16 |
|
| Median weight,
kg | 76.7
(52.6–102.8) |
| 70.8 (37.6–96) |
|
|
| Median pain | 0.49 (0–8) |
| 0.61 (0–7) |
|
|
| Primary tumor
site | 0.621 |
| Oral
cavity | 9 | 36 | 8 | 32 |
|
|
Oropharynx | 5 | 20 | 6 | 24 |
|
|
Nasopharynx | 1 | 4 | 1 | 4 |
|
|
Hypopharynx | 2 | 8 | 1 | 4 |
|
|
Larynx | 8 | 32 | 9 | 36 |
|
| Tumor
histopathology | 0.594 |
|
Squamous cell carcinoma | 21 | 84 | 22 | 88 |
|
|
Adenocarcinoma | 2 | 8 | 1 | 4 |
|
|
Mucoepidermoid | 1 | 4 | 2 | 8 |
|
| Adenoid
cystic carcinoma | 1 | 4 | 0 | 0 |
|
| AJCC stage | 0.71 |
| I | 0 | 0 | 0 | 0 |
|
| II | 5 | 20 | 4 | 16 |
|
|
III | 7 | 28 | 5 | 20 |
|
| IV | 13 | 52 | 16 | 64 |
|
| ECOG-PS | 0.98 |
| 0 | 24 | 96 | 25 | 100 |
|
| 1 | 1 | 4 | 0 | 0 |
|
The incidence of clinical mucositis was 87.5% in the
placebo group and 76% in the glutamine group (81.6% of global
incidence) (Table II). The
incidence and severity grade of clinical and functional mucositis
at the 6th week did not exhibit statistically significantly
differences between the two groups. The comparison of clinical and
functional mucositis had a higher value in placebo group, although
without statistical difference. A direct significant statistical
correlation was found between the values of the clinical and
functional mucositis (P=0.01), with a coefficient of 0.71 and 0.597
at the 3rd and 6th week, respectively.
 | Table II.Incidence and severity of mucositis
and dermatitis. |
Table II.
Incidence and severity of mucositis
and dermatitis.
|
| Placebo group
(n=24) | % | Glutamine group
(n=25) | % | P-value |
|---|
| Incidence of
clinical mucositis | 21 | 87.5 | 19 | 76 | 0.324 |
| Grade of clinical
mucositis |
|
|
|
| 0.341 |
| Grade
0 | 3 | 12.5 | 6 | 24 |
|
| Grade
1 | 10 | 41.7 | 8 | 32 |
|
| Grade
2 | 9 | 36.4 | 10 | 40 |
|
| Grade
3 | 2 | 8.4 | 1 | 4 |
|
| Grade
4 | 0 | 0 | 0 | 0 |
|
| Incidence of
functional mucositis | 18 | 75 | 19 | 76 | 0.511 |
| Grade of functional
mucositis |
|
|
|
| 0.198 |
| Grade
0 | 6 | 25 | 6 | 24 |
|
| Grade
1 | 8 | 33.3 | 9 | 36 |
|
| Grade
2 | 10 | 41.7 | 7 | 28 |
|
| Grade
3 | 0 | 0 | 3 | 12 |
|
| Grade
4 | 0 | 0 | 0 | 0 |
|
| Incidence of
dermatitis | 24 | 100 | 21 | 84 | 0.038a |
| Grade of
dermatitis |
|
|
|
| 0.032a |
| Grade
0 | 0 | 0 | 4 | 16 |
|
| Grade
1 | 11 | 45.8 | 15 | 60 |
|
| Grade
2 | 12 | 50 | 5 | 20 |
|
| Grade
3 | 1 | 4.2 | 1 | 4 |
|
| Grade
4 | 0 | 0 | 0 | 0 |
|
A statistically significant reduction of the
incidence (P=0.038) and severity (P=0.032) of dermatitis was found
in the glutamine group at the 6th week. There were no differences
between groups in the mucositis appearance according to any of
treatment parameters (concomitant chemotherapy, radiation dose and
previous surgery). No statistically significant differences between
the two groups were identified for pain, weight loss and mucositis
onset (Table III). The analysis of
the quality of life questionnaire (MDASI-HN) revealed no
significant differences between groups in any items at the 6th
week. No patient discontinued the study medication due to adverse
effects.
 | Table III.Effect of glutamine on several
outcomes. |
Table III.
Effect of glutamine on several
outcomes.
| Variable | Units | Placebo group
(n=24) | Glutamine group
(n=25) | P-value |
|---|
| Pain | VAS (0–10) |
1.96 |
2.32 |
0.574 |
| Weight | Kg | −2.55 | −3.3 |
0.526 |
| Onset of
mucositis | Days | 29.91 | 28.38 |
0.726 |
| MDASI-HN
questionnaire |
|
| General items |
2.23 | 1.7 |
0.374 |
|
| Specific items | 2.6 | 2.6 | 0.48 |
|
| Impact on daily
activities |
3.05 |
2.58 | 0.54 |
|
| Global |
2.34 |
1.85 |
0.222 |
Discussion
The effectiveness of glutamine for the prevention
and treatment of oral mucositis induced by RT has been examined
recently in some meta-analyses. One meta-analysis (20) identified 5 clinical randomized
controlled trials that included 234 patients with HNC. The
conclusions of this meta-analysis revealed that glutamine
significantly reduced the risk and severity of oral mucositis
induced by RT or CHRT compared with either placebo or no treatment
(risk ratio 0.17; 95% CI 0.06–0.47) (21–25).
Another systematic review of well-designed studies in various solid
tumors and patients with hematological cancer revealed inadequate
or conflicting evidence (26), as
five studies did not find glutamine to be effective (27–30),
while four studies did (19,31–33),
suggesting a requirement for further studies on the use of oral
glutamine to guide clinicians on which interventions are truly
effective.
The findings of the present study did not
demonstrate the primary study endpoint in a statistically
significant manner. However, the incidence and severity of clinical
and functional mucositis tended to be clinically lower in the
glutamine group in comparison with the experimental group, although
it did not reach statistical significance. The frequency of
clinical mucositis was of 87.5% for the placebo group vs. 76% for
the glutamine group and, of a total of 9 patients who did not show
mucositis, 6 were found in the glutamine group. None of patients
presented with a severity grade of 4 at the 6th week, revealing a
homogeneous distribution of clinical mucositis between the two
groups.
Although the present study was unable to demonstrate
the effectiveness of the primary endpoint, oral glutamine
significantly reduced the incidence and severity of dermatitis
produced in the radiation fields, as a secondary endpoint. A
previous study reported that
β-hydroxy-β-methylbutyrate/arginine/glutamine supplementation was
potentially effective in the prevention of radiation dermatitis in
patients with HNC, as this supplementation was a protective
nutrient with anti-inflammatory effects favoring the healing of
inflammatory skin wounds (34).
In the current study, there were no differences in
other outcomes including pain, weight loss and mucositis onset, and
in treatment parameters such as concomitant chemotherapy, radiation
dose and previous surgery. This study was not able to demonstrate
an improvement in the quality of life of patients as no statistical
differences were also found between the two groups in the
assessment of cancer-associated symptoms with the MDASI-HN quality
of life questionnaire.
Very few clinical trials on oral glutamine
administration for the prevention of oral mucositis in patients
with HNC have been reported (21–24). In
general terms, the majority of studies have described favorable
results concerning oral glutamine administration, and consequently
the findings of the present study are not fully consistent with the
indexed literature. However, the comparison with these previous
studies is challenging, as the choice of the primary endpoint, the
δ value and the magnitude of the clinically relevant difference,
were not revealed in the previous studies. In the present study,
mucositis and dermatitis were considered as qualitative variables,
which gave more verisimilitude to clinical reality unlike other
studies in which they were classified as quantitative, thus losing
much data analysis.
The results of the present study must be interpreted
with caution due to the short follow-up period and the reduced
study sample size. The sample size depended upon the 25% δ value,
estimated based on the assumption that the placebo group should
have a 100% incidence of clinical mucositis at the 6th week, which
did not occur. Consequently, a lower δ value may have favored a
larger sample size. This study was a single center study performed
in the authors' setting. Although the distribution of patients was
similar between groups and treatment parameters such as
chemotherapy, radiation dose or previous surgery showed no
difference between groups, a subgroup of analysis could have been
performed if the number of subjects were not too low. Consequently,
multicenter and large-scale studies are warranted. The strengths of
this study were based on its randomized double-blind
placebo-controlled study design. Throughout the trial, the main
researcher monitored the patient test adherence, which resulted in
a 100% adherence, and also performed a count of bags used and
surplus.
Therefore, it is only possible to conclude that, in
this double-blind, randomized study, oral glutamine provided slight
clinical effects compared with placebo in reducing oral mucositis
induced by RT or CHRT in patients with HNC at the 6th week,
although the results were not statically significant. While the
findings of the study suggested a significant benefit in reducing
the incidence and severity of dermatitis, further confirmatory
studies with a new primary endpoint and a larger sample size are
required.
Acknowledgements
The present study formed part of a thesis and
L-glutamine and oral nutrition supplements were gifts of Nutrition
Medica S.L. Laboratories (Madrid, Spain).
References
|
1
|
Moslemi D, Nokhandani AM, Otaghsaraei MT,
Moghadamnia Y, Kazemi S and Moghadamnia AA: Management of
chemo/radiation-induced oral mucositis in patients with head and
neck cancer: A review of the current literature. Radiother Oncol.
120:13–20. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Trotti A, Bellm LA, Epstein JB, Frame D,
Fuchs HJ, Gwede CK, Komaroff E, Nalysnyk L and Zilberberg MD:
Mucositis incidence, severity and associated outcomes in patients
with head and neck cancer receiving radiotherapy with or without
chemotherapy: A systematic literature review. Radiother Oncol.
66:253–262. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Harada K, Ferdous T, Horinaga D, Uchida K,
Mano T, Mishima K, Park S, Hanazawa H, Takahashi S, Okita A, et al:
Efficacy of elemental diet on prevention for
chemoradiotherapy-induced oral mucositis in patients with oral
squamous cell carcinoma. Support Care Cancer. 24:953–959. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cooper JS, Pajak TF, Forastiere AA, Jacobs
J, Campbell BH, Saxman SB, Kish JA, Kim HE, Cmelak AJ, Rotman M, et
al: Postoperative concurrent radiotherapy and chemotherapy for
high-risk squamous-cell carcinoma of the head and neck. N Engl J
Med. 350:1937–1944. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Elliott EA, Wright JR, Swann RS,
Nguyen-Tân F, Takita C, Bucci MK, Garden AS, Kim H, Hug EB, Ryu J,
et al: Phase III trial of an emulsion containing trolamine for the
prevention of radiation dermatitis in patients with advanced
squamous cell carcinoma of the head and neck: Results of radiation
therapy oncology group trial 99–13. J Clin Oncol. 24:2092–2097.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Giro C, Berger B, Bölke E, Ciernik IF,
Duprez F, Locati L, Maillard S, Ozsahin M, Pfeffer R, Robertson AG,
et al: High rate of severe radiation dermatitis during radiation
therapy with concurrent cetuximab in head and neck cancer: Results
of a survey in EORTC institutes. Radiother Oncol. 90:166–171. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mead GM: Management of oral mucositis
associated with cancer chemotherapy. Lancet. 359:815–816. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vélez I, Tamara LA and Mintz S: Management
of oral mucositis induced by chemotherapy and radiotherapy: An
update. Quintessence Int. 35:129–136. 2004.PubMed/NCBI
|
|
9
|
Lalla RV, Bowen J, Barasch A, Elting L,
Epstein J, Keefe DM, McGuire DB, Migliorati C, Nicolatou-Galitis O,
Peterson DE, et al: MASCC/ISOO clinical practice guidelines for the
management of mucositis secondary to cancer therapy. Cancer.
120:1453–1461. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stokman MA, Spijkervet FK, Boezen HM,
Schouten JP, Roodenburg JL and de Vries EG: Preventive intervention
possibilities in radiotherapy- and chemotherapy-induced oral
mucositis: Results of meta-analyses. J Dent Res. 85:690–700. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Keefe DM, Schubert MM, Elting LS, Sonis
ST, Epstein JB, Raber-Durlacher JE, Migliorati CA, McGuire DB,
Hutchins RD and Peterson DE: Mucositis Study Section of the
Multinational Association of Supportive Care in Cancer and the
International Society for Oral Oncology: Updated clinical practice
guidelines for the prevention and treatment of mucositis. Cancer.
109:820–831. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Henke M, Alfonsi M, Foa P, Giralt J,
Bardet E, Cerezo L, Salzwimmer M, Lizambri R, Emmerson L, Chen MG
and Berger D: Palifermin decreases severe oral mucositis of
patients undergoing postoperative radiochemotherapy for head and
neck cancer: A randomized, placebo-controlled trial. J Clin Oncol.
29:2815–2820. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xu JL, Xia R, Sun ZH, Sun L, Min X, Liu C,
Zhang H and Zhu YM: Effects of honey use on the management of
radio/chemotherapy-induced mucositis: A meta-analysis of randomized
controlled trials. Int J Oral Maxillofac Surg. 45:1618–1625. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wischmeyer PE: Clinical applications of
L-glutamine: Past, present, and future. Nutr Clin Pract.
18:377–385. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Neu J, DeMarco V and Li N: Glutamine:
Clinical applications and mechanisms of action. Curr Opin Clin Nutr
Metab Care. 5:69–75. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Skubitz KM and Anderson PM: Oral glutamine
to prevent chemotherapy induced stomatitis: A pilot study. J Lab
Clin Med. 127:223–228. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Silverman S Jr: Diagnosis and management
of oral mucositis. J Support Oncol. 5 2 Suppl 1:S13–S21. 2007.
|
|
18
|
Savarese DM, Savy G, Vahdat L, Wischmeyer
PE and Corey B: Prevention of chemotherapy and radiation toxicity
with glutamine. Cancer Treat Rev. 29:501–513. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Choi K, Lee SS, Oh SJ, Lim SY, Lim SY,
Jeon WK, Oh TY and Kim JW: The effect of oral glutamine on
5-fluorouracil/leucovorin-induced mucositis/stomatitis assessed by
intestinal permeability test. Clin Nutr. 26:57–62. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Leung HW and Chan AL: Glutamine in
alleviation of radiation-induced severe oral mucositis: A
meta-analysis. Nutr Cancer. 68:734–742. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Huang EY, Leung SW, Wang CJ, Chen HC, Sun
LM, Fang FM, Yeh SA, Hsu HC and Hsiung CY: Oral glutamine to
alleviate radiation-induced oral mucositis: A pilot randomized
trial. Int J Radiat Oncol Biol Phys. 46:535–539. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cerchietti LC, Navigante AH, Lutteral MA,
Castro MA, Kirchuk R, Bonomi M, Cabalar ME, Roth B, Negretti G,
Sheinker B and Uchima P: Double-blinded, placebo-controlled trial
on intravenous L-alanyl-L-glutamine in the incidence of oral
mucositis following chemoradiotherapy in patients with head
and-neck cancer. Int J Radiat Oncol Biol Phys. 65:1330–1337. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chattopadhyay S, Saha A, Azam M, Mukherjee
A and Sur PK: Role of oral glutamine in alleviation and prevention
of radiation-induced oral mucositis: A prospective randomized
study. South Asian J Cancer. 3:8–12. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tsujimoto T, Yamamoto Y, Wasa M, Takenaka
Y, Nakahara S, Takagi T, Tsugane M, Hayashi N, Maeda K, Inohara H,
et al: L-glutamine decreases the severity of mucositis induced by
chemoradiotherapy in patients with locally advanced head and neck
cancer: A double-blind, randomized, placebo-controlled trial. Oncol
Rep. 33:33–39. 2015.PubMed/NCBI
|
|
25
|
Vidal-Casariego A, Calleja-Fernández A,
Ballesteros-Pomar MD and Cano-Rodríguez I: Efficacy of glutamine in
the prevention of oral mucositis and acute radiation induced
esophagitis: A retrospective study. Nutr Cancer. 65:424–429. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yarom N, Ariyawardana A, Hovan A, Barasch
A, Jarvis V, Jensen SB, Zadik Y, Elad S, Bowen J and Lalla RV:
Mucositis Study Group of the Multinational Association of
Supportive Care in Cancer/International Society of Oral Oncology
(MASCC/ISOO): Systematic review of natural agents for the
management of oral mucositis in cancer patients. Support Care
Cancer. 21:3209–3221. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jebb SA, Osborne RJ, Maughan TS, Mohideen
N, Mack P, Mort D, Shelley MD and Elia M: 5-fluorouracil and
folinic acid induced mucositis: No effect of oral glutamine
supplementation. Br J Cancer. 70:732–735. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Anderson PM, Schroeder G and Skubitz KM:
Oral glutamine reduces the duration and severity of stomatitis
after cytotoxic cancer chemotherapy. Cancer. 83:1433–1439. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Okuno SH, Woodhouse CO, Loprinzi CL, Sloan
JA, LaVasseur BI, Clemens-Schutjer D, Swan D, Axvig C, Ebbert LP,
Tirona MR, et al: Phase III controlled evaluation of glutamine for
decreasing stomatitis in patients receiving fluorouracil
(5-FU)-based chemotherapy. Am J Clin Oncol. 22:258–261. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ward E, Smith M, Henderson M, Reid U,
Lewis I, Kinsey S, Allgar V, Bowers D and Picton SV: The effect of
high-dose enteral glutamine on the incidence and severity of
mucositis in paediatric oncology patients. Eur J Clin Nutr.
63:134–140. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Rubio IT, Cao Y, Hutchins LF, Westbrook KC
and Klimberg VS: Effect of glutamine on methotrexate efficacy and
toxicity. Ann Surg. 227:772–778; 778–780. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cockerham MB, Weinberger BB and Lerchie
SB: Oral glutamine for the prevention of oral mucositis associated
with high-dose paclitaxel and melphalan for autologous bone marrow
transplantation. Ann Pharmacother. 34:300–303. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Peterson DE, Jones JB and Petit RG II:
Randomized, placebo-controlled trial of Saforis for prevention and
treatment of oral mucositis in breast cancer patients receiving
anthracycline-based chemotherapy. Cancer. 109:322–331. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Imai T, Matsuura K, Asada Y, Sagai S,
Katagiri K, Ishida E, Saito D, Sadayasu R, Wada H and Saijo S:
Effect of HMB/Arg/Gln on the prevention of radiation dermatitis in
head and neck cancer patients treated with concurrent
chemoradiotherapy. Jpn J Clin Oncol. 44:422–427. 2014. View Article : Google Scholar : PubMed/NCBI
|