Introduction
Gastrointestinal stromal tumors (GISTs) are the most
common mesenchymal tumors of the GI tract. GISTs most commonly
develop in the stomach (50–60%) and small intestine (30–35%),
although they may also arise in the large intestine (5–10%),
esophagus (<1%) and, rarely, in locations outside the GI tract
(mesentery, omentum and retroperitoneum, <5%) (1,2). GISTs
originating from the vermiform appendix are rare, constituting only
0.1% of all GISTs, and they are sized <3 cm in 82.4% of the
reported cases. Several previous studies have reported the
usefulness of neoadjuvant therapy with imatinib mesylate, a
selective tyrosine kinase inhibitor, in locally advanced or
metastatic/recurrent GISTs (3). We
herein report a case of a giant GIST of the appendix with a single
peritoneal metastasis in a 67-year-old man, who subsequently
underwent neoadjuvant imatinib therapy, which resulted in effective
tumor shrinkage, allowing minimally invasive laparoscopic
surgery.
Case report
A 67-year-old man with a 6-month history of lower
abdominal pain due to a large abdominal mass lesion was referred to
the Department of Surgical Oncology (University of Tokyo Hospital,
Tokyo, Japan) in February, 2014. The patient's medical history
included chronic rhinosinusitis 30 years prior and endoscopic
colonic polypectomy 1 year prior. A physical examination revealed
that the patient was afebrile, with normal vital signs. Mild
tenderness was detected in the lower abdomen, with a palpable mass
sized >20 cm. Laboratory tests revealed mildly decreased
hemoglobin and albumin levels (11.0 and 3.4 g/dl, respectively),
mildly elevated C-reactive protein level (1.39 mg/dl), normal white
blood cell count (4,700/µl) and normal carcinoembryonic antigen
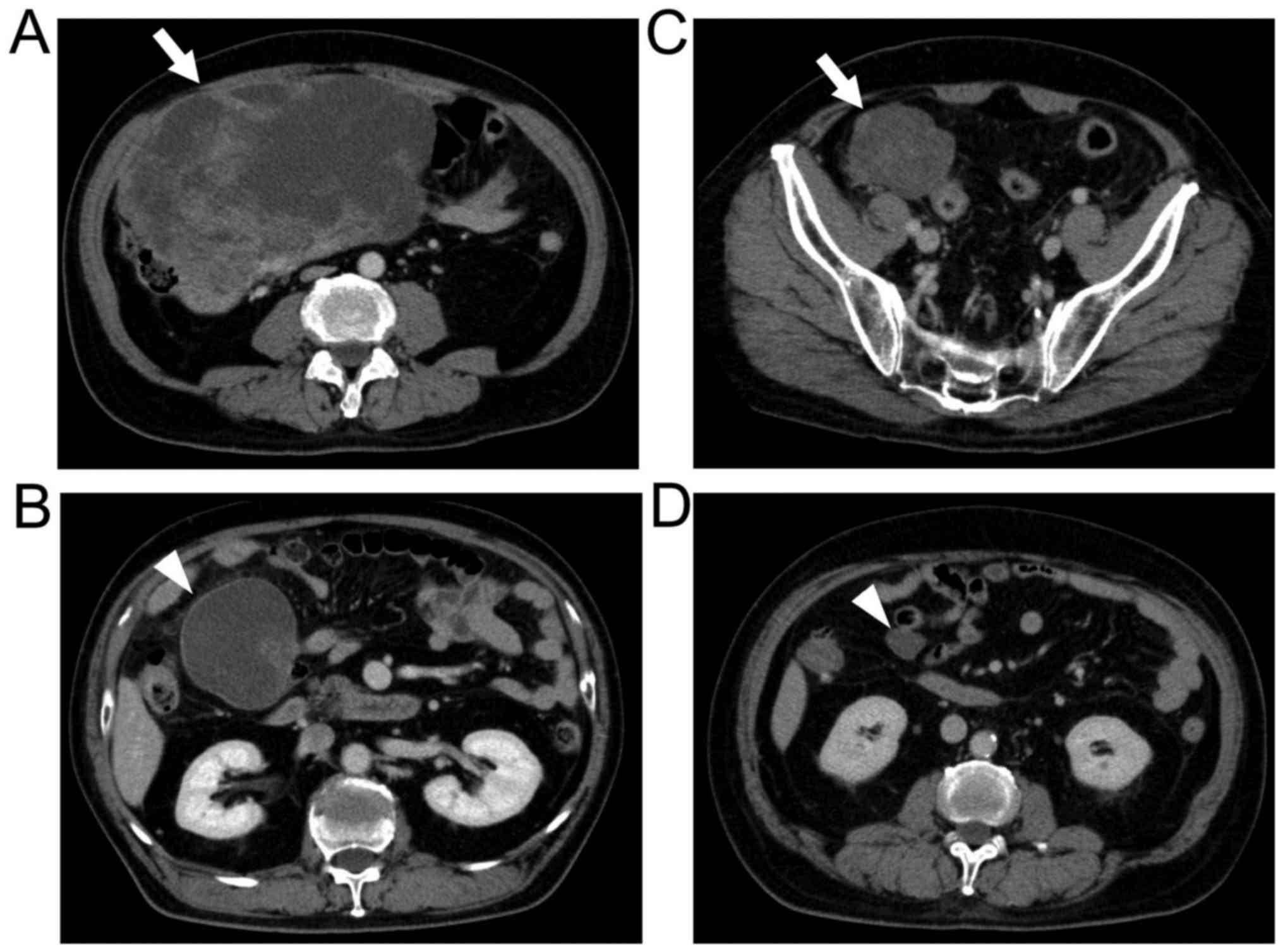
level (2.1 ng/ml; normal level, <5 ng/ml). An abdominal computed
tomography (CT) scan revealed a large mass (220×180×100 mm) with
heterogeneous enhancement in the right lower abdominal quadrant.
Due to its size, the tumor origin was unclear. A CT scan also
revealed another mass (70×65×50 mm) located cranially to the main
tumor (Fig. 1A and B).
Esophagogastroduodenoscopy, colonoscopy and capsule endoscopy
revealed no evidence of other neoplastic lesions. CT-guided
fine-needle biopsy showed bundles of spindle cells stained positive
for c-KIT (Fig. 2), with 5 mitotic
cells per 50 high-power fields, and a Ki-67 (MIB-1) labeling index
of >10%. There was no desmin or protein S100 immunoreactivity.
On the basis of these findings, the tumors were diagnosed as GISTs,
possibly arising from the ileum, cecum or appendix, with a
peritoneal metastasis. The case was determined to be high-risk
according to criteria proposed by Miettinen et al (1) and Joensuu et al (4).
Due to the size of the tumor and the presence of
peritoneal metastasis, neoadjuvant therapy with imatinib 400 mg/day
was initiated; no imatinib-related adverse events were detected
during treatment. Follow-up imaging studies revealed a gradual
decrease in tumor size. After 26 months of imatinib treatment, a
final evaluation revealed 63×55-mm and 22×20-mm masses, without a
significant change in size over the prior 3 months (Fig. 1C and D). Subsequently, laparoscopic
exploration revealed that the main tumor originated from the tip of
the vermiform appendix (Fig. 3) and
that the peritoneal metastasis was located in the ascending
mesocolon. Consequently, appendectomy and grossly complete
resection of the peritoneal metastatic tumor were laparoscopically
performed, without tumor rupture. The gross specimen of the main
tumor was a whitish-gray hemorrhagic mass, sized 80×60×55 mm,
growing outward from the tip of the appendix (50 mm in length, 10
mm in diameter). The peritoneal metastatic tumor (22×18×14 mm) had
the same gross appearance. Microscopic examination revealed no
lymphovascular invasion and a mitotic count of 2/50 high-power
fields in the main tumor. The postoperative course was uneventful
and the patient was discharged without complications. The patient
commenced imatinib treatment 1 month after surgery and he remained
alive and disease-free at the last follow-up, 6 months after the
surgery. The date of the last follow-up was 8th March, 2017.
Written informed consent was obtained from the
patient for the publication of the case details and associated
images.
Discussion
GISTs of the vermiform appendix constitute only 0.1%
of all GISTs (1), with only 16 cases
reported in the English literature to date (5–16). The
characteristics of these 17 GIST cases (including the present case)
are listed in Table I. The median
patient age was 67 years (range, 7–88 years) and the male:female
ratio was 2.4:1. The tumor originated from the proximal end of the
appendix in 5 cases, from the middle in 5, from the tip in 5, and
information on the origin was unavailable in 2 cases. Seven
patients presented with appendicitis-like symptoms without
histological evidence of acute appendicitis, suggesting that the
symptoms were caused by the tumor. Two patients presented with
peritonitis, which was caused by acute appendicitis in one case,
and by formation of a peri-appendiceal abscess in the other case.
The remaining 6 tumors were incidentally discovered during surgery
for other diseases or during autopsy. The median size was 12.5 mm
(range, 0.5–220 mm). To the best of our knowledge, the present case
represents the largest appendiceal GIST reported to date. The tumor
was so large that the patient experienced pain in the entire lower
abdomen, and the origin of the tumor could not be determined by
preoperative investigation. Furthermore, our case was classified as
high-risk according to the criteria of Joensuu et al
(4), whereas 14 of the 17 reported
appendiceal GISTs (82.4%) were classified as very low- or
low-risk.
 | Table I.Characteristics of previously reported
cases of GIST originating in the vermiform appendix. |
Table I.
Characteristics of previously reported
cases of GIST originating in the vermiform appendix.
| Authors | Year | Case | Age, years | Gender | Location | Presentation | Tumor size, mm | Mitotic rate (/50
HPFs) | (Refs.) |
|---|
| Miettinen et
al | 2001 | 1 | 64 | M | Tip | Incidental
finding | 14 | <1 | (5) |
| Miettinen et
al | 2001 | 2 | 56 | M | Proximal | Appendicitis-like
symptoms | 12 | <1 | (5) |
| Miettinen et
al | 2001 | 3 | 59 | M | Middle | Incidental
finding | 9×5 | <1 | (5) |
| Miettinen et
al | 2001 | 4 | 72 | M | Proximal | Acute
appendicitis | 13 | <1 | (5) |
| Yap et al | 2005 | 5 | 66 | F | Middle | Appendicitis-like
symptoms | 2.5 | <1 | (6) |
| Kim et al | 2007 | 6 | 56 | M | Middle | Hematochezia | NA | NA | (7) |
| Rahimi et
al | 2008 | 7 | 65 | F | NA | Incidental
finding | 11 | <1 | (8) |
| Agaimy et
al | 2008 | 8 | 86 | F | NA | Incidental
finding | 0.5 | <1 | (9) |
| Agaimy et
al | 2008 | 9 | 78 | F | Proximal | Acute
appendicitis | 5 | <1 | (10) |
| Agaimy et
al | 2008 | 10 | 72 | M | Tip | Incidental
finding | 25 | <1 | (10) |
| Elazary et
al | 2010 | 11 | 57 | M | Tip | Acute
appendicitis | 200 | 9 | (11) |
| Chung et
al | 2012 | 12 | 67 | M | Middle | Appendicitis-like
symptoms | 60×40×30 | <5 | (12) |
| Bouassida et
al | 2013 | 13 | 75 | M | Middle | Acute
appendicitis | 20 | NA | (13) |
| Tran et
al | 2014 | 14 | 7 | M | Proximal | Appendicitis-like
symptoms | 5×3×2 | NA | (14) |
| Back et
al | 2015 | 15 | 88 | F | Tip | Incidental
finding | 5 | <1 | (15) |
| Chun et
al | 2016 | 16 | 68 | M | Proximal | Appendicitis-like
symptoms | 30×25×25 | <1 | (16) |
| Present case |
| 17 | 67 | M | Tip | Lower abdominal
pain | 220×180×100 | 5 |
|
Complete surgical resection is the only curative
treatment for GIST. However, the introduction of imatinib therapy,
which is established as an adjuvant therapy following surgery in
high-risk cases, as well as first-line therapy in metastatic cases,
has markedly improved the cure rate and the prognosis (17). In addition, several studies have
demonstrated that neoadjuvant therapy with imatinib for locally
advanced or metastatic/recurrent GISTs may offer advantages, such
as cytoreduction, in order to facilitate R0 resection, the
potential for organ preservation, a less invasive surgical approach
and a lower risk of intraoperative tumor rupture (3,18,19). As
the present case included a giant tumor with peritoneal metastasis,
tumor rupture or macroscopic residual tumor (R2 resection) was a
possible risk. Thus, neoadjuvant imatinib was administered to
decrease the tumor size in order to achieve complete resection
(R0/R1) (20). After 26 months of
imatinib treatment, the patient underwent laparoscopic appendectomy
and gross complete resection of the peritoneal metastatic tumor,
without tumor rupture. The optimal duration of neoadjuvant therapy
for GIST remains controversial. Theoretically, neoadjuvant therapy
may be continued until the tumor size decreases or its metabolic
activity reaches a plateau phase, but the development of resistance
due to secondary KIT mutations during this stage remains a risk
(21). The duration of neoadjuvant
imatinib therapy in a metastatic setting should be case-based,
depending on the response to treatment. The main aim of neoadjuvant
treatment is to convert unresectable/borderline-resectable disease
to resectable disease.
In conclusion, appendiceal GISTs sized >10 cm are
extremely rare. We herein reported a case of an unusually large
appendiceal GIST (22 cm) with a solitary peritoneal metastasis,
which was successfully treated with neoadjuvant imatinib therapy
and laparoscopic surgery. Therefore, in appropriately selected
patients, neoadjuvant imatinib for borderline resectable or
oligometastatic GISTs may be a reasonable choice.
References
|
1
|
Miettinen M and Lasota J: Gastrointestinal
stromal tumors: Pathology and prognosis at different sites. Semin
Diagn Pathol. 23:70–83. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Joensuu H, Hohenberger P and Corless CL:
Gastrointestinal stromal tumour. Lancet. 382:973–983. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ford SJ and Gronchi A: Indications for
surgery in advanced/metastatic GIST. Eur J Cancer. 63:154–167.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Joensuu H: Risk stratification of patients
diagnosed with gastrointestinal stromal tumor. Hum Pathol.
39:1411–1419. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Miettinen M and Sobin LH: Gastrointestinal
stromal tumors in the appendix: A clinicopathologic and
immunohistochemical study of four cases. Am J Surg Pathol.
25:1433–1437. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yap WM, Tan HW, Goh SG and Chuah KL:
Appendiceal gastrointestinal stromal tumor. Am J Surg Pathol.
29:1545–1547. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kim KJ, Moon W, Park MI, Park SJ, Lee SH
and Chun BK: Gastrointestinal stromal tumor of appendix
incidentally diagnosed by appendiceal hemorrhage. World J
Gastroenterol. 13:3265–3267. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rahimi K, Gologan A, Haliotis T, Lamoureux
E and Chetty R: Gastrointestinal stromal tumor with autonomic nerve
differentiation and coexistent mantle cell lymphoma involving the
appendix. Int J Clin Exp Pathol. 20:608–613. 2008.
|
|
9
|
Agaimy A, Wünsch PH, Dirnhofer S, Bihl MP,
Terracciano LM and Tornillo L: Microscopic gastrointestinal stromal
tumors in esophageal and intestinal surgical resection specimens: A
clinicopathologic, immunohistochemical and molecular study of 19
lesions. Am J Surg Pathol. 32:867–873. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Agaimy A, Pelz AF, Wieacker P, Roessner A,
Wünsch PH and Schneider-Stock R: Gastrointestinal stromal tumors of
the vermiform appendix: Clinicopathologic, immunohistochemical, and
molecular study of 2 cases with literature review. Hum Pathol.
39:1252–1257. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Elazary R, Schlager A, Khalaileh A,
Appelbaum L, Bala M, Abu-Gazala M, Khatib A, Neuman T, Rivkind AI
and Almogy G: Malignant appendiceal GIST: Case report and review of
the literature. J Gastrointest Cancer. 41:9–12. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chung JC and Song OP: Gastrointestinal
stromal tumor of the appendix. Turk J Gastroenterol. 23:303–304.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bouassida M, Chtourou MF, Chalbi E, Chebbi
F, Hamzaoui L, Sassi S, Charfi L, Mighri MM, Touinsi H and Sassi A:
Appendiceal GIST: Report of an exceptional case and review of the
literature. Pan Afr Med J. 15:852013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tran S, Dingeldein M, Mengshol SC, Kay S
and Chin AC: Incidental GIST after appendectomy in a pediatric
patient: A first instance and review of pediatric patients with
CD117 confirmed GISTs. Pediatr Surg Int. 30:457–466. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Back J, Jeanty J and Landas S:
Gastrointestinal stromal tumor of the appendix: Case report and
review of the literature. Hum Pathol Case Rep. 2:94–98. 2015.
View Article : Google Scholar
|
|
16
|
Chun JM and Lim KH: Gastrointestinal
stromal tumor of the vermiform appendix mimicking Meckel's
diverticulum: Case report with literature review. Int J Surg Case
Rep. 21:20–22. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Valsangkar N, Sehdev A, Misra S, Zimmers
TA, O'Neil BH and Koniaris LG: Current management of
gastrointestinal stromal tumors: Surgery, current biomarkers,
mutations, and therapy. Surgery. 158:1149–1164. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Andtbacka RH, Ng CS, Scaife CL, Cormier
JN, Hunt KK, Pisters PW, Pollock RE, Benjamin RS, Burgess MA, Chen
LL, et al: Surgical resection of gastrointestinal stromal tumors
after treatment with imatinib. Ann Surg Oncol. 14:14–24. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Benjamin RS, Choi H, Macapinlac HA,
Burgess MA, Patel SR, Chen LL, Podoloff DA and Charnsangavej C: We
should desist usingRECIST, at least in GIST. J Clin Oncol.
25:1760–1764. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bauer S, Rutkowski P, Hohenberger P,
Miceli R, Fumagalli E, Siedlecki JA, Nguyen BP, Kerst M, Fiore M,
Nyckowski P, et al: Long-term follow-up of patients with GIST
undergoing metastasectomy in the era of imatinib-analysis of
prognostic factors (EORTC-STBSG collaborative study). Eur J Surg
Oncol. 40:412–419. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Haller F, Detken S, Schulten HJ, Happel N,
Gunawan B, Kuhlgatz J and Füzesi L: Surgical management after
neoadjuvant imatinib therapy in gastrointestinal stromal tumours
(GISTs) with respect to imatinib resistance caused by secondary KIT
mutations. Ann Surg Oncol. 14:526–532. 2007. View Article : Google Scholar : PubMed/NCBI
|