Introduction
Intracranial meningiomas, the most common central
nervous system (CNS) tumors, account for ~30% of all CNS tumors in
adults, whereas pediatric intracranial meningiomas are rare,
comprising only 0.4–4.6% of all pediatric primary intracranial
tumors (1,2). As pediatric intracranial meningiomas
are rare, there is little available information on their
epidemiology, treatment and prognosis.
Pediatric intracranial meningiomas are characterized
by the presence of uncommon lesions within the intraventricular or
intraorbital locations. They are slightly more predominant in males
and appear to be more aggressive compared with adult cases of
meningioma. In the present case report, we present the clinical
course of a 3-year-old boy with anaplastic meningioma who developed
extracranial metastases.
Case report
A 3-year-old boy was admitted to the Department of
Pediatrics (University of Occupational and Environmental Health,
Kitakyushu, Japan) in April 2011, due to vomiting, fever and
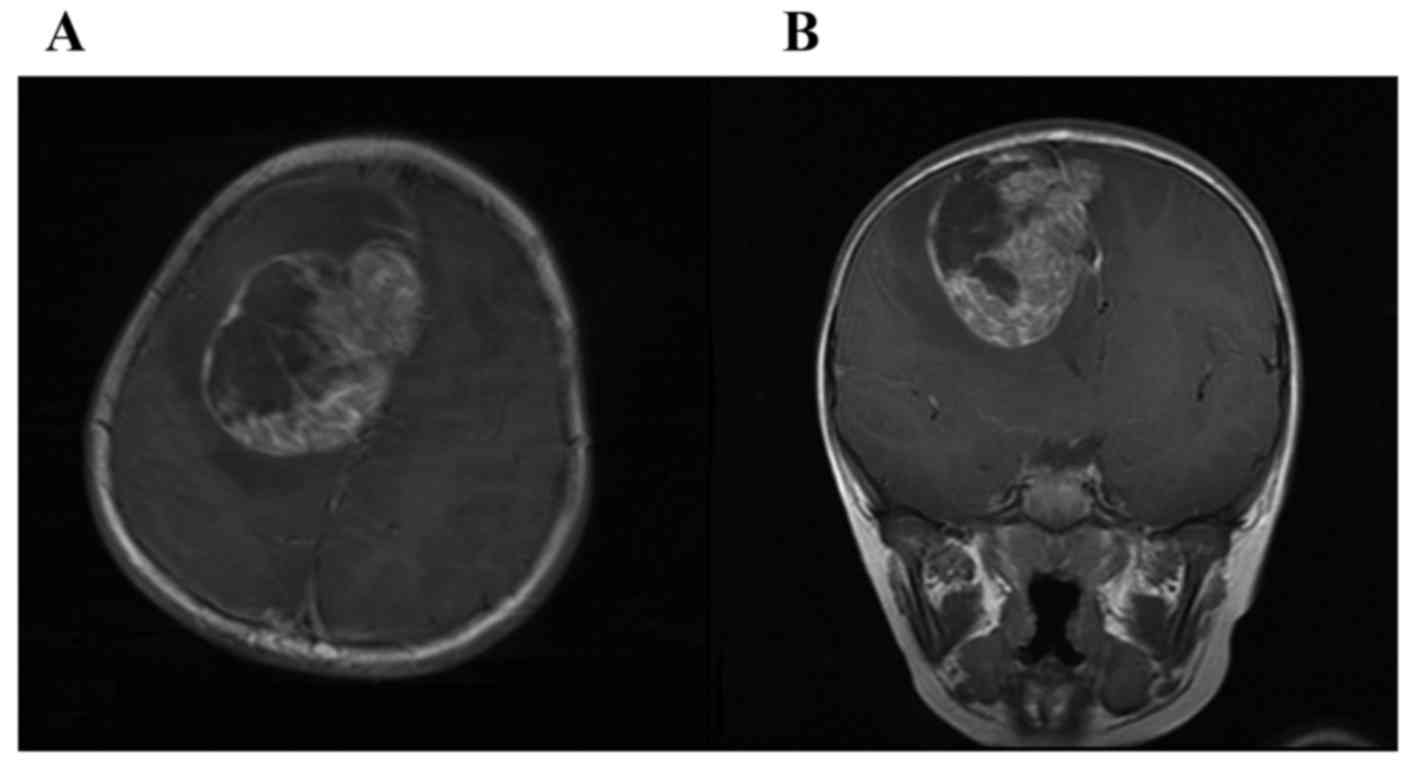
left-side weakness that had lasted for 10 days. A brain computed
tomography (CT) scan revealed an isodense mass lesion in the right
frontal lobe with severe peritumoral brain edema. Magnetic
resonance imaging (MRI) revealed a 70-mm mass lesion in the right
frontal lobe with heterogeneous intensity associated with
intratumoral hemorrhage (Fig. 1). On
the day after his admission, the patient's consciousness
progressively deteriorated. Emergency surgery was thus performed
and the tumor was removed in its entirety. The histological
diagnosis was anaplastic meningioma, World Health Organization
(WHO) grade III, and the MIB-1 labeling index was 25.4%.
Two months after the first operation, an MRI of the
head revealed a local recurrence at the same site as the initial
tumor. Thus, a second operation was performed and the tumor was
completely removed. However, 10 days later, multiple tumors were
detected in other areas of the brain. Radiotherapy (6,120 cGy,
frontal region irradiation) was then administered, resulting in
disappearance of the recurrent tumors. The patient had no
neurological defects, and no further tumors were detected over the
subsequent 4 months, throughout which regular MRI examinations were
conducted.
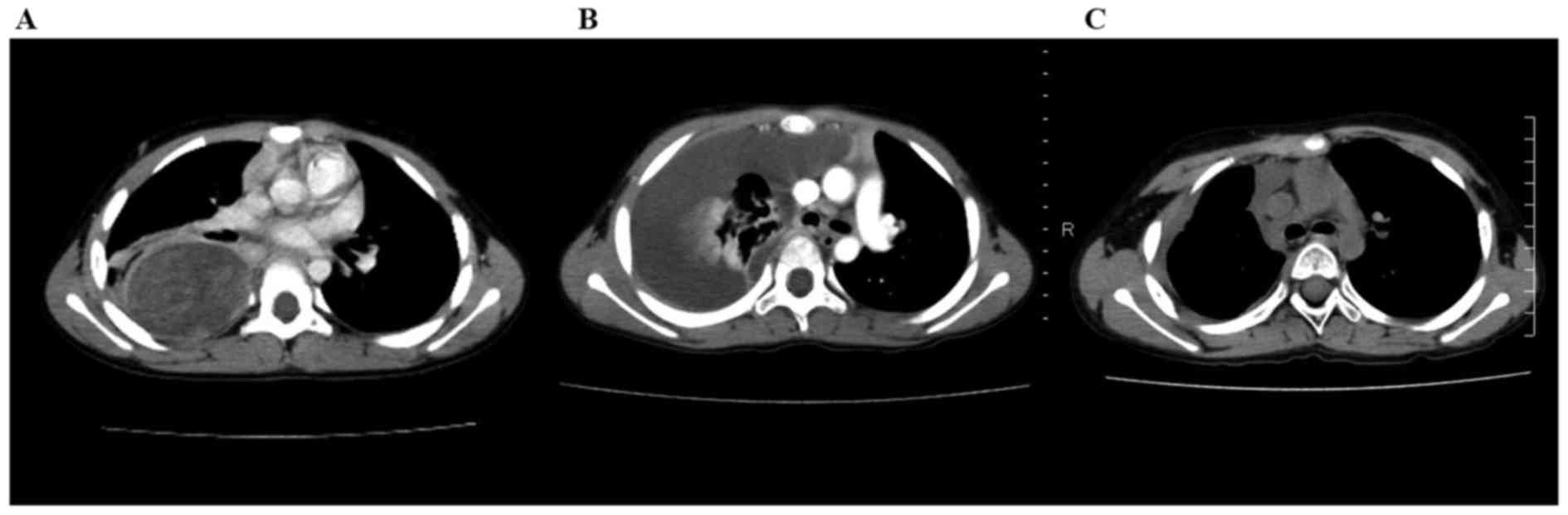
At 8 months after the initial operation, the patient
developed cough, fever, chest pain, and had difficulty breathing. A
CT scan of the thorax revealed a large mass (~85 mm) with pleural
effusion in the right lung (Fig.
2A). As there was no evidence of other local recurrence or
malignant lesions in any other organs, a right middle and lower
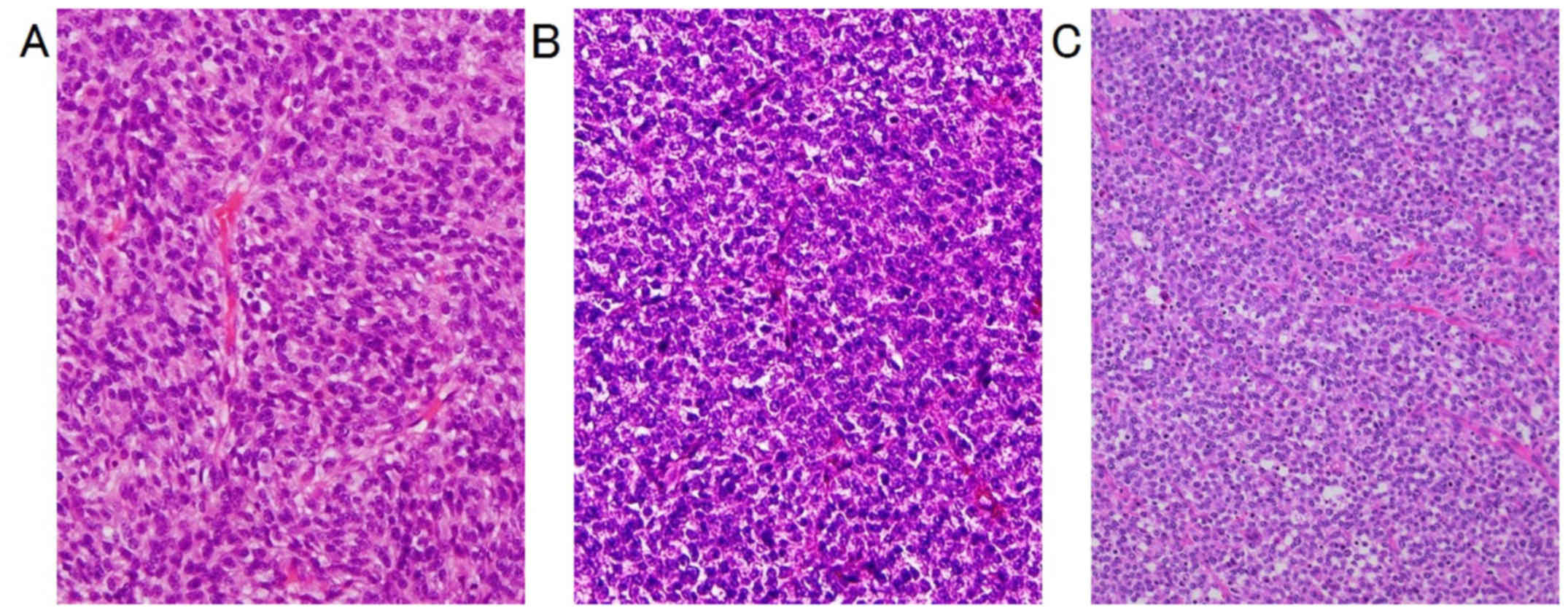
lobectomy was performed. Tissue specimens obtained from the lung
revealed that the tumor was well-demarcated from the adjacent lung
parenchyma and exhibited focal necrotic and hemorrhagic changes.
The tumor cells had oval nuclei with a high nuclear-cytoplasmic
ratio and large, prominent nucleoli (Fig. 3). Immunohistochemical examination
revealed strong expression of anti-cytokeratin (CAM5.2) and CD99;
furthermore, the MIB-1 (Ki-67) proliferation index was 80%. Based
on these findings, the diagnosis was lung metastasis of anaplastic
meningioma, in agreement with the pathological characteristics of
the primary intracranial anaplastic meningioma. The tumor was then
completely surgically removed; however, multiple pleural-based
tumors were detected during a follow-up MRI 1 month after the
lobectomy (Fig. 2B) and local
radiotherapy was administered. Although the pleural-based tumors
disappeared following administration of radiotherapy (Fig. 2C), they reappeared shortly after the
completion of radiation therapy in the right lung and right frontal
lobe. In response to this finding, 4 additional courses of
radiotherapy were administered for these lesions. Unfortunately,
the radiotherapy was ultimately unsuccessful in the treatment of
these metastases and the patient succumbed to the disease ~1 year
and 4 months after the initial diagnosis. The patient's family has
consented to the publication of the case details and associated
images.
Discussion
As cases of pediatric intracranial meningioma are
rare, only small single-center and retrospective studies of these
neoplasms have been published to date (1–3).
Furthermore, all these studies have consistently found that the
clinical and biological aspects of pediatric intracranial
meningioma cases differ from those of adult cases.
According to the WHO classification system, there
are 15 subtypes of meningioma (4).
In adults, ~90% of meningiomas are benign (grade I), with 5–7%
classified as aggressive (grade II) and the remaining 1–3% graded
as malignant (grade III) (5). By
contrast, higher grades are more common in pediatric meningiomas. A
meta-analysis determined the incidence of WHO grade II and III
meningiomas to be 9.9 and 8.9%, respectively. Furthermore, it has
been reported that WHO grade III pediatric meningioma cases, had a
significantly worse relapse-free survival (RFS) rate compared with
WHO grade I tumors (5-year RFS rates: 40.7 vs. 81.2%,
respectively). However, the WHO grading system does not account for
the overall survival rate for pediatric meningiomas (6). Thus, the biological behavior of
pediatric meningiomas is notoriously difficult to predict on the
basis of the WHO grade alone.
Kotecha et al reported that the extent of the
initial surgical resection was the strongest independent prognostic
factor (6). However, some reports
indicated that recurrence was very common for high-grade lesions,
even following complete resection (1,7,8). Our case is consistent with these latter
reports, as, although gross total excision of the tumor was
possible, the tumor reappeared in the same location 2 months
later.
The MIB-1 index is an important prognostic factor
for meningiomas. In adults, the MIB-index is well-correlated with
the histological grade and the rate of tumor recurrence. However,
conversely, there is a lack of corresponding data on pediatric
meningiomas due to the limited number of cases. Wang et al
reported that the association between the MIB-1 index and the
pathological grade was generally weak for intracranial pediatric
meningiomas. Moreover, pediatric meningiomas with an MIB-1 index
>3% appeared to have a worse prognosis (9). In the present case, the patient's MIB-1
index was relatively high at diagnosis and increased progressively,
reaching 80% at the lung metastasis stage. This progression of the
MIB-1 index was associated with the proliferative potential of the
tumor and the time interval to the next recurrence or lung
metastasis. For malignant meningiomas, it is difficult to make a
reliable prognosis on the basis of the MIB-1 index at the time of
diagnosis, or based on the results of surgical resection alone.
Therefore, pediatric patients with malignant meningioma or a high
MIB-1 index must be carefully monitored, as physicians must be
aware of the possibility of an extracranial metastasis in such
cases.
Although metastasis of meningioma is a rare
phenomenon in adult patients, it has been well-documented and its
incidence has been estimated to be 0.1% (10,11).
According to the results of the systematic review by Surov et
al (12), metastatic lesions
were localized most frequently in the lungs (37.2%), bones (16.5%),
intraspinally (15.2%) and in the liver (9.2%). Unlike adult cases,
metastatic meningioma is extremely rare in pediatric cases; thus,
there are only few reports on extracranial metastases (6,12) and
the corresponding rate has not yet been determined. To the best of
our knowledge, prior to our report, a total of 4 cases of pediatric
meningioma with lung metastases have been published (Table I) and our report presents the
youngest such patient. Moreover, all 5 cases, including ours, were
classified as WHO grade III, and the mean patient age was 9 years
(range, 3–14 years). Although the intracranial tumors were
completely resected in 3 of the 5 cases (60%), they all recurred.
The time interval between the initial diagnosis and the occurrence
of lung metastases ranged from 8 to 18 months. All the patients
succumbed to lung metastasis, and their survival times ranged from
8 to 30 months. Therefore, based on the present case and the few
preceding reported cases, it is our conclusion that meningioma
cases that progress to metastasis are very resistant to treatment,
even following gross total resection.
 | Table I.Characteristics of pediatric
meningiomas that developed lung metastases. |
Table I.
Characteristics of pediatric
meningiomas that developed lung metastases.
| Age, sex | Location at Dx | Pathology | GTR | Recurrence | Time interval between
Dx and lung metastasis | Outcome (months) | (Refs.) |
|---|
| 5, f | Right occipital | Papillary | Yes | Yes | 18 months | Deceased (23) | (9) |
| 9, m | Right parietal | Anaplastic | No | Yes | 8 months | Deceased (8) | (9) |
| 12, f | Parasagittal | Malignant | ND | Yes | ND | Deceased (14) | (2) |
| 14, m | Parietal scalp and
skull | Malignant | Yes | Yes | ND | Deceased (30) | (13) |
| 3, m | Right frontal | Anaplastic | Yes | Yes | 9 months | Deceased (15) | Present case |
There is currently no standard treatment for
metastatic meningioma, and there are no particularly effective
medications for this disease. Although surgical excision is the
treatment of first choice for pediatric and adult meningiomas,
complete tumor resection cannot prevent recurrence or metastasis.
Furthermore, radiotherapy is currently considered by the National
Institute for Health and Clinical Excellence to be a plausible form
of treatment for adults with WHO grade II or III tumors, multiple
relapses, contraindication to surgery, invasion of adjacent brain,
or extensive invasion of other tissues (14). Conversely, according to the
Children's Cancer and Leukemia Group (CCLG) guidelines, the data
supporting the use of adjuvant radiotherapy for pediatric high-risk
cases are scant; however, radiotherapy should be considered at the
time of the primary diagnosis, regardless of the surgical outcome,
particularly in cases of WHO grade III anaplastic meningioma
(15).
In the present case, the patient ultimately
succumbed to disease progression, despite radiotherapy treatment.
However, it should be noted that radiotherapy was somewhat
effective initially in preventing local recurrence and it also
prolonged the patient's survival time. Furthermore, no further
intracranial tumors were detected even 2 months after the
occurrence of metastases to the lungs, and the patient survived for
a further 7 months after the metastases. Therefore, although there
is no conclusive data regarding the benefit of adjuvant
radiotherapy in pediatric meningioma cases, it may be associated
with some benefits in malignant cases of pediatric meningioma.
Furthermore, although the mechanism of pulmonary
metastases from intracranial meningiomas is unclear, it is thought
that the main dissemination pathway is through the CSF and venous
sinus invasion (12,16). If surgical resection of a tumor has
the potential to damage the blood brain barrier and, thus,
instigate distant metastasis, radiotherapy may be useful at the
time of primary diagnosis in WHO grade III pediatric anaplastic
meningioma cases.
To reiterate, the number of cases of pediatric
meningioma are extremely rare and only small single-center and
retrospective studies are currently available. Thus, in order to
assess the positive effects of radiotherapy, prospective clinical
trials are required.
In conclusion, the occurrence of metastatic
meningiomas is possible, although rare, in young children.
Furthermore, high-grade pediatric meningiomas are associated with
high recurrence and mortality rates, and there are currently no
definitive criteria for estimating the probability of recurrence or
metastasis. Therefore, such patients should be closely monitored
throughout the follow-up period. Moreover, due to the rarity of
pediatric meningioma, there is currently no standard treatment for
metastatic meningioma. Thus, the true incidence and impact of
distant metastases in this subset of patients should be
corroborated through prospective clinical trials.
References
|
1
|
Ravindranath K, Vasudevan MC, Pande A and
Symss N: Management of pediatric intracranial meningiomas: An
analysis of 31 cases and review of literature. Childs Nerv Syst.
29:573–582. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rushing EJ, Olsen C, Mena H, Rueda ME, Lee
YS, Keating RF, Packer RJ and Santi M: Central nervous system
meningiomas in the first two decades of life: A clinicopathological
analysis of 87 patients. J Neurosurg. 103 (6 Suppl):S489–S495.
2005.
|
|
3
|
Lakhdar F, Arkha Y, EI Ouahabi A, Melhaoui
A, Rifi L, Derraz S and El Khamlichi A: Intracranial meningioma in
children: Different from adult forms? A series of 21 cases.
Neurochirurgie. 56:309–314. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Commins DL, Atkinson RD and Burnett ME:
Review of meningioma histopathology. Neurosurg Focus. 23:E32007.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kotecha RS, Pascoe EM, Rushing EJ,
Rorke-Adams LB, Zwerdling T, Gao X, Li X, Greene S, Amirjamshidi A,
Kim SK, et al: Meningiomas in children and adolescents: A
meta-analysis of individual patient data. Lancet Oncol.
12:1229–1239. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Arivazhagan A, Devi BI, Kolluri SV,
Abraham RG, Sampath S and Chandramouli BA: Pediatric intracranial
meningiomas-do they differ from their counterparts in adults?
Pediatr Neurosurg. 44:43–48. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Greene S, Nair N, Ojemann JG, Ellenbogen
RG and Avellino AM: Meningiomas in children. Pediatr Neurosurg.
44:9–13. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang XQ, Jiang CC, Zhao L, Gong Y, Hu J
and Chen H: Clinical features and treatment of World Health
Organization grade II and III meningiomas in childhood: Report of
23 cases. J Neurosurg Pediatr. 10:423–433. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Alexandru D, Glantz MJ, Kim L, Chamberlain
MC and Bota DA: Pulmonary metastases in patients with recurrent,
treatment-resistant meningioma: Prognosis and identification by
111Indium-octreotide imaging. Cancer. 117:4506–4511.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rhim JK, Sheen SH, Noh JS and Chung SB:
Pulmonary metastasis of malignant meningioma. J Korean Neurosurg
Soc. 35:533–535. 2004.
|
|
12
|
Surov A, Gottschling S, Bolz J, Kornhuber
M, Alfieri A, Holzhausen HJ, Abbas J and Kösling S: Distant
metastases in meningioma: An underestimated problem. J Neurooncol.
112:323–327. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Baumgartner JE and Sorenson JM: Meningioma
in the pediatric population. J Neurooncol. 29:223–228. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
National Institute for Health and Clinical
Excellence: Improving Outcomes for People with Brain and Other CNS
Tumours: Guidance on Cancer Services. NICE. http://www.nice.org.uk/guidance/csgbraincns/evidence/improving-outcomes-for-people-with-brain-and-other-cns-tumours-the-manual2Accessed.
20–March;2015.
|
|
15
|
Traunecker H, Mallucci C, Grundy R, Pizer
B and Saran F: Children's Cancer and Leukaemia Group: Children's
Cancer and Leukaemia Group (CCLG): Guidelines for the management of
intracranial meningioma in children and young people. Br J
Neurosurg. 22:13–25. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Forest F, Berremila SA, Gyenes C, Ginguéné
C, Kassir R, Sulaiman A, Pasquier B, Porcheron J and Péoc'h M:
Metastatic meningiomas: An unusual clinical and pathological
diagnosis with highly variable outcome. J Neurooncol. 120:411–421.
2014. View Article : Google Scholar : PubMed/NCBI
|