Introduction
In thyroid surgery, damage to the recurrent
laryngeal nerve (RLN) and superior laryngeal nerve external branch
(SLNEB) is the most serious complication. Therefore, it is
necessary to identify and preserve these nerves. The
electromyography (EMG) monitoring system represented by Nerve
Integrity Monitor (NIM) (Medtronic Xomed, Jacksonville, FL, USA) is
useful for RLN and SLNEB preservation in cases in which the tumor
is large, or if there is tumor invasion into the adjacent tissue.
Recently, RLN monitoring with an EMG has become widely applied
(1–9). Intraoperative nerve monitoring is
necessary for nerve function preservation. However, not all
hospitals are equipped with an EMG monitoring system and, as a
result, RLN and SLNEB monitoring is difficult. Therefore, an
alternative monitoring method is required, and it was this need
that drove us to design a novel RLN and SLNEB monitoring method.
When RLN and SLNEB are stimulated with a facial nerve stimulator
(FNS), movement of the vocal cord may be observed with an
Airwayscope™ (AWS; Ricoh, Tokyo, Japan), more efficiently compared
with the laryngeal fiberscope during surgery. The successful
combination of these devices was employed as a complete alternative
to EMG. In the present study, we were able to not only monitor and
preserve the nerves, but also to confirm the absence of RLN injury
following resection.
Materials and methods
Equipment
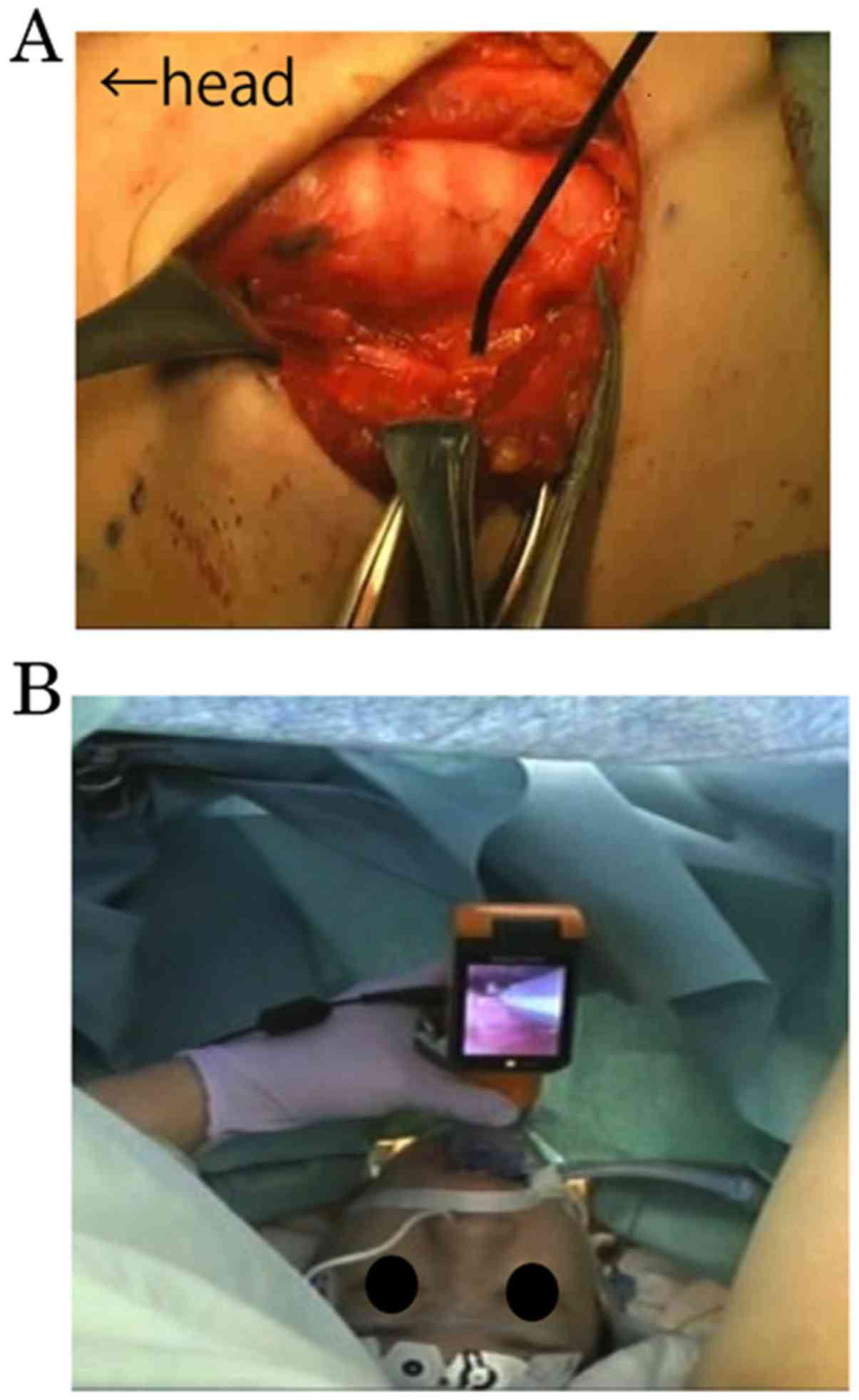
AWS is a laryngoscope currently being used for
difficult cases of endotracheal intubation under general
anesthesia. A fiberscope is attached to the tip of the laryngoscope
blade, from which an image is be observed via a 2.5-inch monitor
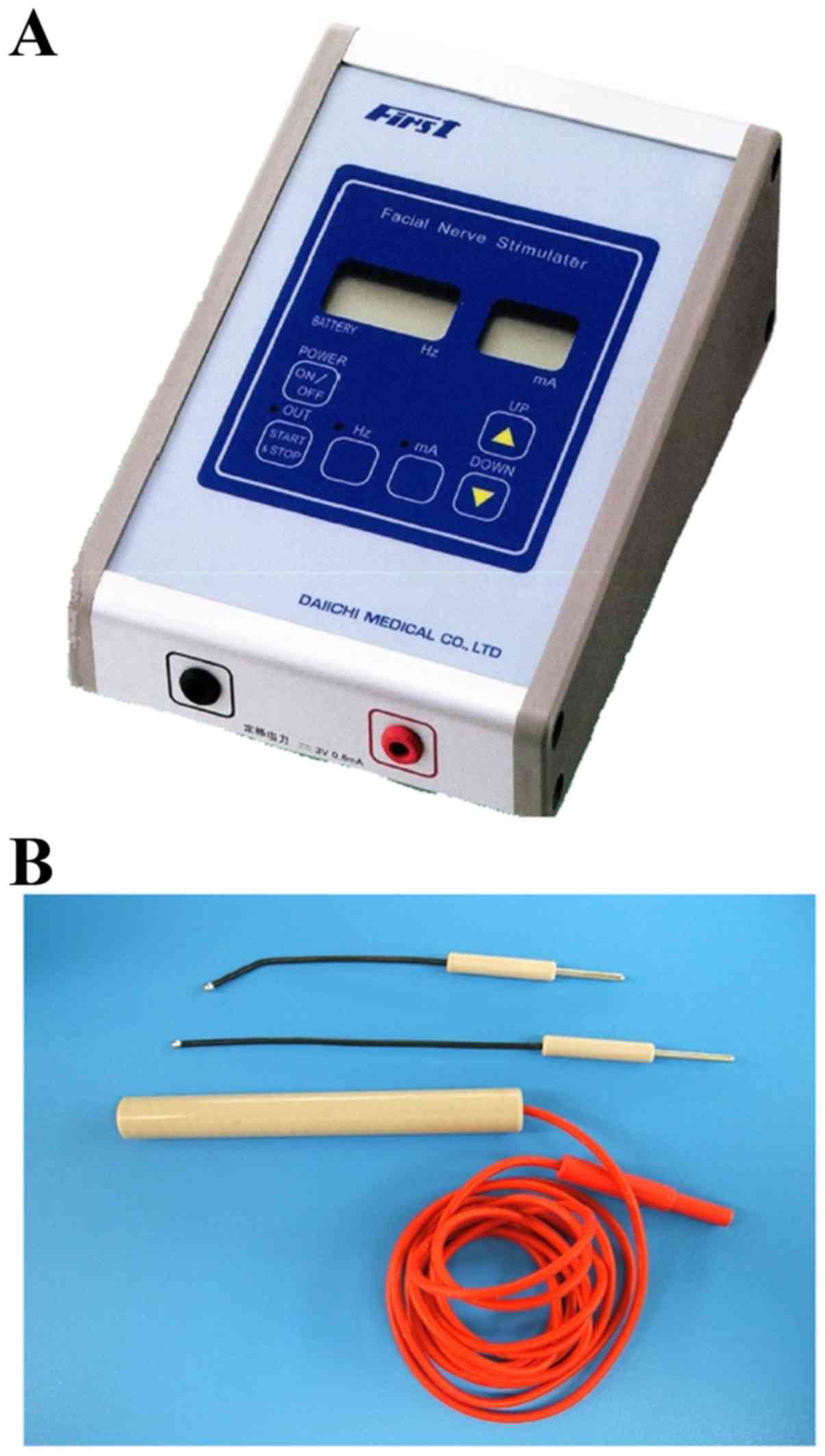
(Fig. 1). An FNS is commonly used in
parotid surgery and neurosurgery. The nerve is electrically
stimulated by the FNS probe during surgery (Figs. 2 and 3).
Method
In the present study, the method of RLN monitoring
was designed using these devices in unison. The FNS electrode
stimulates the RLN, and the resulting movement of the vocal cord is
observed with the AWS transorally. This method enables effective
monitoring of the RLN and SLNEB during thyroid surgery. The AWS
monitor and the fiber may be easily detached from the AWS blade,
thus allowing for only the blade to be kept for insertion into the
larynx during the operation. Moreover, an AWS is equipped with an
external connection terminal and all operation staff may observe
the movement of the vocal cord from an external TV monitor. The FNS
is used with an amplitude of 0.5–2.0 mA, and a stimulus duration of
0.5 sec.
The present study was approved by the Institutional
Review Board of Nagoya City University and all the participants
provided informed consent. All associated images are used with
permission of the companies.
Results
Patients
The present study was conducted on 10 patients
admitted to Nagoya City University Hospital (Nagoya, Aichi) in 2012
with an initial diagnosis of a thyroid tumor, who were considered
suitable to undergo surgery with AWS and FNS monitoring (Table I).
 | Table I.Patient and surgical characteristics
with nerve monitoring. |
Table I.
Patient and surgical characteristics
with nerve monitoring.
| Age, years | Sex | Pathology | Operation | Operative time,
min |
|---|
| 41 | Female | Benign | Lobectomy | 174 |
| 55 | Male | Malignant | Lobectomy + CND | 338 |
| 66 | Male | Malignant | Lobectomy + CND | 140 |
| 72 | Female | Benign | Lobectomy | 111 |
| 36 | Female | Benign | Lobectomy | 147 |
| 40 | Male | Benign | Lobectomy | 233 |
| 60 | Female | Malignant | Lobectomy + CND | 178 |
| 64 | Female | Malignant | Thyloidectomy +
CND | 291 |
| 67 | Female | Malignant | Thyloidectomy +
CND | 430 |
| 57 | Male | Benign | Lobectomy | 169 |
Procedure and outcome
At the nerve monitoring step, the surgeon delivered
the electrical stimulus to the RLN and SLNEB in the patient's
operative field. At the same time, the anesthesiologist inserted
the AWS blade into the larynx and positioned the fiberscope to
observe the area surrounding the vocal cord. All the surgical staff
was able to observe the response of the vocal cord to electrical
stimulus in all cases.
The view from the monitor revealed that the vocal
cord moved transversely in response to RLN stimulation. In
addition, with SLNEB stimulation, vocal cord expansion and
contraction were observed. The vocal cord movement was recorded to
a DVD or hard disk, so that it may be reviewed after the
operation.
In all cases, the RLN was preserved and the
normality of motor nerve function was confirmed during surgery. No
RLN palsy occurred postoperatively.
When assessing the vocal cord movement, the time
required to insert the AWS blade into the larynx was ~2–5 min,
apart from 1 case, in which 10 min were required to obtain a
sufficient view of the vocal cord movement, as the laryngeal space
was relatively narrow. The results were sufficient to confirm the
safety and validity of this new monitoring method.
Discussion
In the present study, a new RLN and SLNEB monitoring
procedure was designed, combining an AWS and an FNS during thyroid
surgery. Intraoperative identification and functional monitoring of
the RLN and SLNEB are crucial in thyroid surgery. Several reports
have proposed that EMG monitoring is an acceptable adjunct for
identification and preservation of the RLN. Most surgeons opt for
the EMG monitoring approach with a commercially prepared NIM EMG
endotracheal tube (1–9). There are, however, other alternatives
to EMG systems that are similar to an NIM (e.g., Lantern, Magstim
Co. Ltd., Carmarthenshire, UK; and Nerveana, Neurovision Medical
Products Inc., Ventura, CA, USA) However, the number of hospitals
that are equipped with an NIM or similar EMG system is limited. In
response, the present study used a combination of an AWS and an FNS
to develop an effective alternative to RLN and SLNEB monitoring
that differs from an EMG in how the vocal cord movement is
observed.
As a functional monitoring method, our technique has
limitations compared with an EMG, as caution is required for there
is no warning sound of mechanical damage when the nerve is
stimulated. Furthermore, unlike EMG, our method is unable to track
electromyographic activity numerically. However, the primary goal
of nerve monitoring is to evaluate neuro-functional status during
surgery. In all 10 cases in this study, confirmation of the
normality of vocal cord movement and the identification of the RLN
were achieved. However, dysfunction of the NIM-EMG tube has been
reported in 3.8–23% of the cases (1). In our method, the setup failure is
zero, as a sensing electrode is not used. In addition, vocal cord
movement may be better observed with AWS rather than with a
laryngeal fiberscope in the supine position. As regards the cost of
the monitoring, a previous study reported that the use of an EMG
tube for thyroid surgery increases the cost of each surgery, as the
attached equipment is non-reusable and must be disposed of
(8). Our method only requires an AWS
blade and an FNS electrode, which is more cost-effective for each
surgery when compared with an EMG tube and FNS electrode. In a
previous report, the EMG response to stimulation of the vagus nerve
was correlated with the postoperative functional status of the
patients (10). With our method, at
the end of surgery, patients exhibited a normal response to RLN
stimulation and had no vocal cord palsy. In addition, no other
complications were observed intra- or postoperatively.
The method described herein is a readily available
alternative to an EMG when laryngeal nerve monitoring is
unexpectedly required, such as in cases where a surgery suddenly
reveals a non-recurrent laryngeal nerve. The AWS and FNS may be
easily and quickly set up during surgery with the cooperation of
the anesthesiologist.
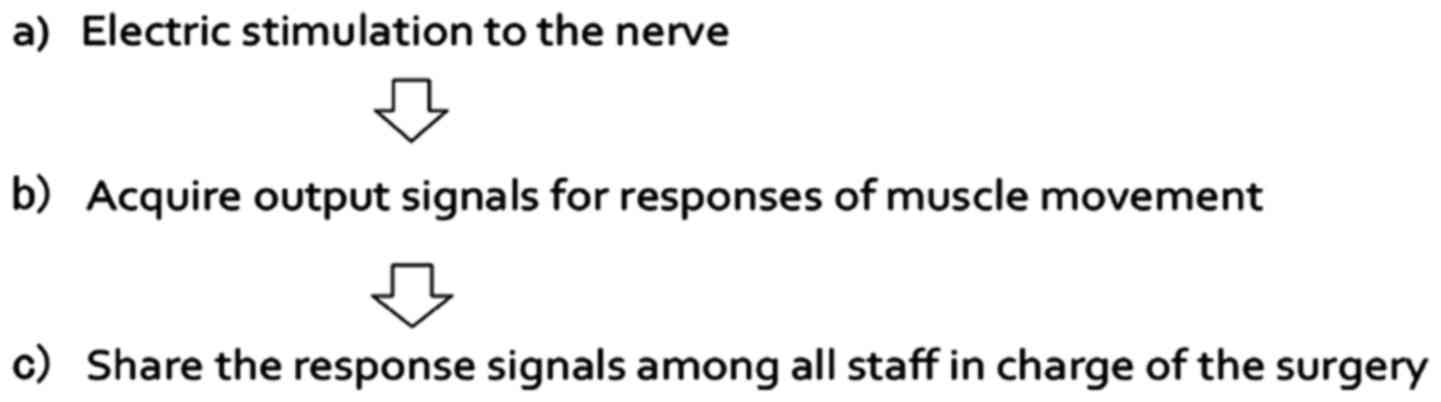
Motor nerve monitoring consist of three steps: i)
Electric stimulation of the nerve, ii) acquiring output signals for
responses of muscle movement and iii) sharing the response signals
among all surgical staff involved in the surgery (Fig. 4). This monitoring method has two
benefits regarding the flow of medical information: First, the
movie of the vocal cord movement may be exported to an external TV
monitor connected to the AWS. The AWS may be connected by a plug
into a jack on a side. All the surgical stuff can share the
information of laryngeal nerve function in real time. Second, this
movie may be recorded onto a DVD or hard disk drive, so that
laryngeal nerve preservation may be reconfirmed postoperatively.
This method fulfills all the steps required for nerve monitoring as
outlined above. Alternative laryngoscopes to an AWS include
GlideScope (Verathon Inc., Bothell, WA, USA) and McGrath (Aircraft
Medical Ltd., Edinburgh, UK), both of which are equipped with a
monitor. However, at the time of this report, only an AWS was able
to export the movie of the vocal cord movement to an external TV
monitor.
Our method may allow assessment of neural integrity
in parapharyngeal and cervical surgery, neurosurgery and thoracic
surgery, with good approximation to the NIM system (11,12).
However, in the case of neural tumor invasion or a large tumor
around the nerve, nerve monitoring with an AWS and FNS is
difficult.
In conclusion, the AWS and FNS method described
herein is useful for conventional thyroid surgery, with an
effectiveness similar to that of EMG monitoring.
Thus, the new RLN and SLNEB monitoring method using
AWS and FNS is useful in thyroid surgery if only a confirmation of
normal function of vocal cord is required. This method is more
likely to be readily available and the results are similar to that
of EMG monitoring, although there is no alert of mechanical damage
to the nerve with this method. Moreover, this monitoring method
also offers a more cost-effective alternative, with no loss of
reliability, and it enables valuable sharing and reconfirmation of
information on laryngeal nerve function during the surgery through
the TV monitor.
References
|
1
|
Lu IC, Chu KS, Tsai CJ, Wu CW, Kuo WR,
Chen HY, Lee KW and Chiang FY: Optimal depth of NIM EMG
endotracheal tube for intraoperative neuromonitoring of the
recurrent laryngeal nerve during thyroidectomy. World J Surg.
32:1935–1939. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Donnellan KA, Pitman KT, Cannon CR,
Replogle WH and Simmons JD: Intraoperative laryngeal nerve
monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg.
135:1196–1198. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Julien N, Mosnier I, Grayeli Bozorg A, Nys
P, Ferrary E and Sterkers O: Intraoperative laryngeal nerve
monitoring during thyroidectomy and parathyroidectomy: A
prospective study. Eur Ann Otorhinolaryngol Head Neck Dis.
129:69–76. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chiang FY, Lee KW, Chen HC, Chen HY, Lu
IC, Kuo WR, Hsieh MC and Wu CW: Standardization of intraoperative
neuromonitoring of recurrent laryngeal nerve in thyroid operation.
World J Surg. 34:223–229. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tomoda C, Hirokawa Y, Uruno T, Takamura Y,
Ito Y, Miya A, Kobayashi K, Matsuzuka F, Kuma K and Miyauchi A:
Sensitivity and specificity of intraoperative recurrent laryngeal
nerve stimulation test for predicting vocal cord palsy after
thyroid surgery. World J Surg. 30:1230–1233. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Schneider R, Bures C, Lorenz K, Dralle H,
Freissmuth M and Hermann M: Evolution of nerve injury with
unexpected EMG signal recovery in thyroid surgery using continuous
intraoperative neuromonitoring. World J Surg. 37:364–368. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chiang FY, Lu IC, Kuo WR, Lee KW, Chang NC
and Wu CW: The mechanism of recurrent laryngeal nerve injury during
thyroid surgery-the application of intraoperative neuromonitoring.
Surgery. 143:743–749. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gremillion G, Fatakia A, Dornelles A and
Amedee RG: Intraoperative recurrent laryngeal nerve monitoring in
thyroid surgery: Is it worth the cost? Ochsner J. 12:363–366.
2012.PubMed/NCBI
|
|
9
|
Mikuni N, Satow T, Taki J, Nishida N,
Enatsu R and Hashimoto N: Endotracheal tube electrodes to map and
monitor activities of the vagus nerve intraoperatively. Technical
note. J Neurosurg. 101:536–540. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morota N, Deletis V, Epstein FJ, Kofler M,
Abbott R, Lee M and Ruskin K: Brain stem mapping:
Neurophysiological localization of motor nuclei on the floor of the
fourth ventricle. Neurosurgery. 37:922–930. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao J, Xu H, Li W, Chen L, Zhong D and
Zhou Y: Intraoperative recurrent laryngeal nerve monitoring during
surgery for left lung cancer. J Thorac Cardiovasc Surg.
140:578–582. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ito E, Ichikawa M, Itakura T, Ando H,
Matsumoto Y, Oda K, Sato T, Watanabe T, Sakuma J and Saito K: Motor
evoked potential monitoring of the vagus nerve with transcranial
electrical stimulation during skull base surgeries. J Neurosurg.
118:195–201. 2013. View Article : Google Scholar : PubMed/NCBI
|