Introduction
Epithelioid hemangioendothelioma (EHAE) is a rare
low-to-intermediate-grade malignant vascular tumor derived from
endothelial cells (1,2). EHAE was first described in 1975 by Dail
and Liebow as an aggressive bronchoalveolar cell carcinoma
(3). The term epithelioid
hemangioendothelioma was introduced in 1982 by Weiss and Enzinger,
who described the tumor as originating from blood vessels (1). The estimated incidence of EHAE is
<1/million, with a female:male ratio of 3:2 (4). Primary hepatic EHAE is an extremely
rare occurrence and was first reported in 1984 by Ishak et
al (5).
The aim of the present study was to report a case of
EHAE presenting with multiple lesions in the liver and a lesion in
the mesentery of the small intestine.
Case report
A 64-year-old woman was admitted to the Toyooka
Hospital (Toyooka, Japan) in November 2013 with elevated levels of
serum aspartate aminotransferase and alanine aminotransferase and
due to tumors in the liver, which were identified on a computed
tomography (CT) scan. The patient did not report any noticeable
symptoms related to the tumor; she had diabetes mellitus and
hypertension, and she was receiving treatment with estradiol
dipropionate and dydrogesterone for climacteric symptoms. The
patient's family cancer history was significant: Her father had
been diagnosed with gastric and lung cancer, her mother had been
diagnosed with pancreatic cancer, her older brother had been
diagnosed with cancer of the urinary bladder, her older sister had
been diagnosed with ovarian cancer, and her younger sister had been
diagnosed with breast cancer.
An enhanced CT scan revealed multiple low-density
tumors with an enhanced margin in the liver and a 30-mm irregular
tumor in the mesentery (Fig. 1).
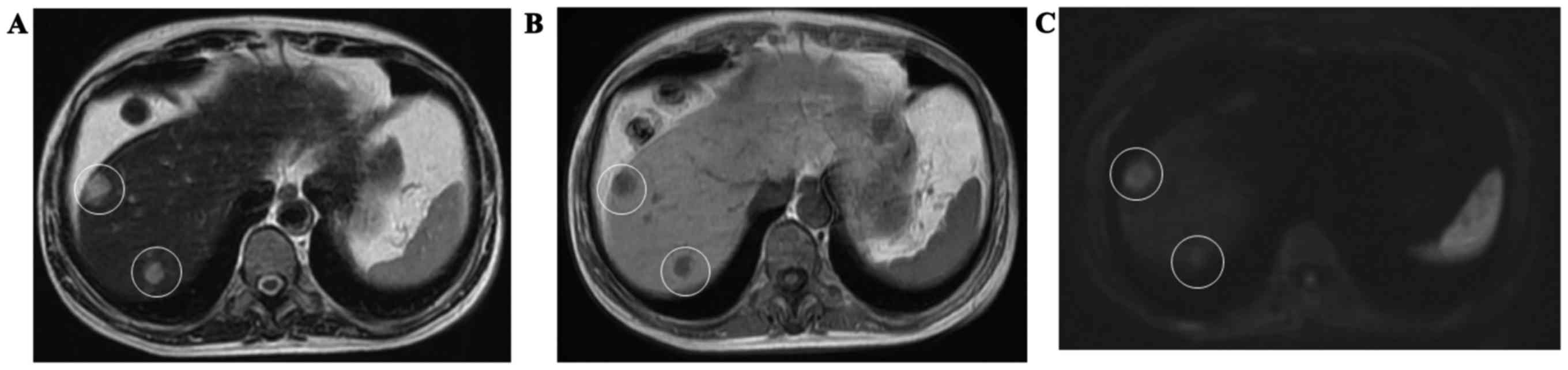
Ethoxybenzyl-magnetic resonance imaging revealed that the tumor had
high signal intensity on T2-weighted images (Fig. 2A), low signal intensity in
T1-weighted images (Fig. 2B) and
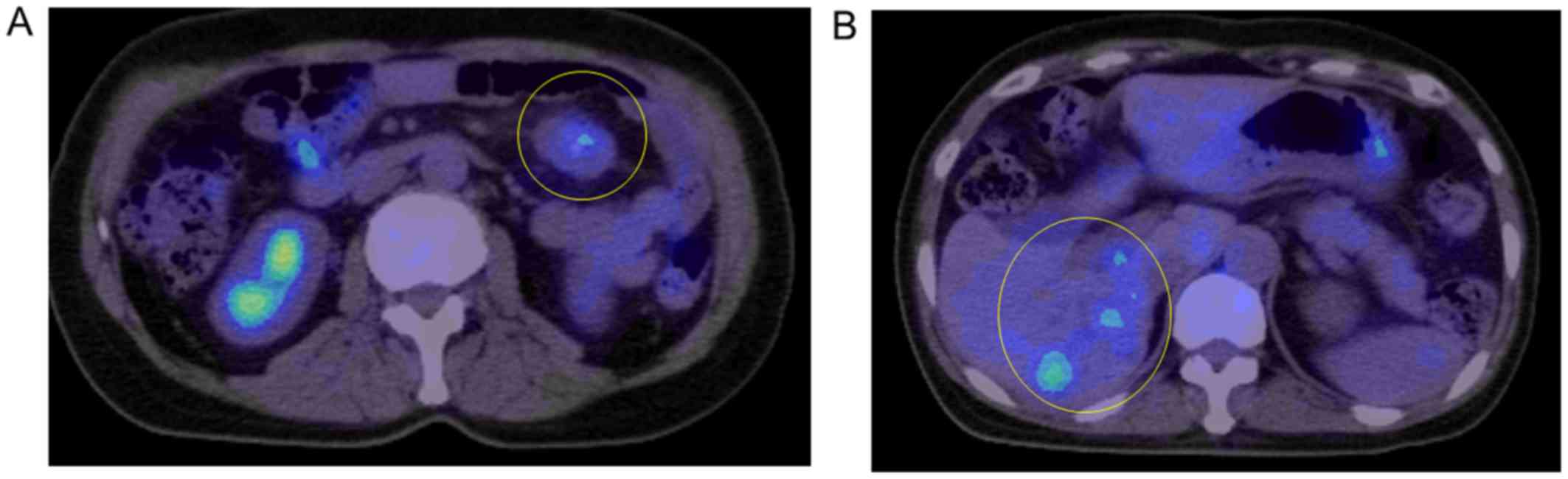
high signal intensity on diffusion-weighted images (Fig. 2C). These tumors also presented as hot
spots on positron emission tomography/CT scan (Fig. 3). Blood tests revealed normal levels
of carcinoembryonic antigen, α-fetoprotein and carbohydrate antigen
19–9. There were no abnormalities noted on the upper or lower
gastrointestinal endoscopic examinations.
On laparoscopic observation, several whitish tumors
were identified on the bilateral lobes of the liver and on the
mesentery of the small intestine. It was impossible to resect all
the tumors, since multiple lesions were present in both the left
and right lobes of the liver. As we were unable to determine
whether the hepatic and mesenteric tumors were of the same type by
diagnostic imaging alone, resection of the mesenteric tumor and one
of the hepatic tumors was attempted and the resected specimens were
sent for histological examination.
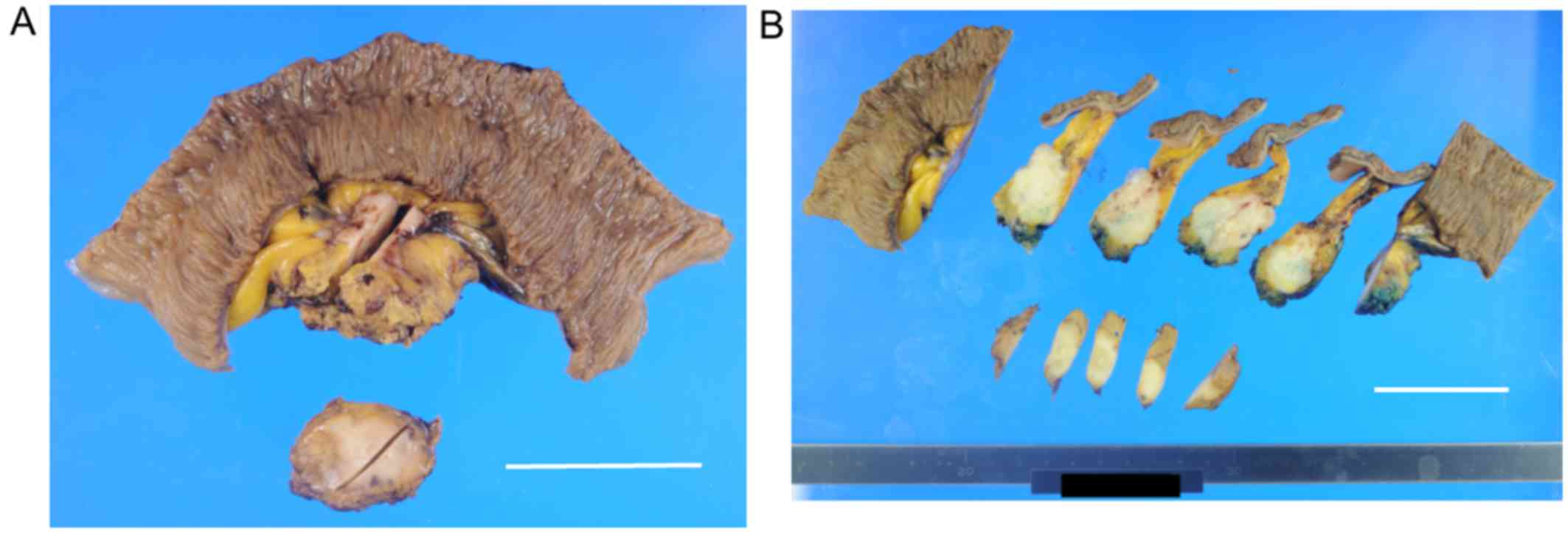
The size of the mesenteric and hepatic tumors was
33×28×25 and 25×25×10 mm, respectively (Fig. 4). The tumors were hard and whitish on
cross-section, and they were relatively well-defined, with
irregular margins. Histologically, the two tumors exhibited similar
characteristics, such as epithelioid and dendritic cells with
abundant cytoplasm and atypical nuclei (Fig. 5). In the periphery of the tumor, the
tumor cells proliferated along pre-existing sinusoids. In the
center of the tumor, the myxomatous stroma was conspicuous and
contained tumor cells that were present either as single cells or
in small groups. Some tumor cells were arranged in a trabecular
pattern.
Immunohistologically, the tumor was positive for
vimentin and vascular endothelial growth factor receptor (VEGFR)2,
partially positive for CD31, CD34 and factor VIII, and negative for
cytokeratin AE1/AE3, hepatocyte-specific antigen, c-Kit, α-smooth
muscle actin and S-100, suggesting that the tumor was derived from
the endothelial cells of the blood vessels (Fig. 5 and data not shown). Moreover, the
tumor was partially positive for CAM5.2.
Based on the macroscopic and microscopic
characteristics, as well as the results of the immunohistological
examination, the tumor was diagnosed as EHAE originating in the
liver with metastasis to the mesentery.
As the residual hepatic tumors were multiple and
were present in both the left and right lobes of the liver, they
could not all be resected. Therefore, radiofrequency ablation was
performed for the hepatic lesions and the patient was treated with
pazopanib, which is a potent and selective multi-targeted receptor
tyrosine kinase inhibitor that blocks tumor growth and inhibits
angiogenesis, as EHAE expresses VEGFR2 (Flk-1) and platelet-derived
growth factor receptor β. Approximately 3 years and 7 months after
the first hospital visit, the patient maintains stable disease
under pazopanib treatment (the hepatic tumors have not grown and
there are no additional metastatic lesions). The patient's last
follow-up was in June 2017.
Discussion
We herein described a case of EHAE arising in a
64-year-old woman presenting as multiple lesions in the liver and a
single lesion in the mesentery.
It has been reported that EHAE is a rare tumor, and
that its most common site of origin is the liver (4). However, some cases of EHAE originating
in the mesentery or peritoneum have been reported. It is
conceivable that, in the present case, the EHAE first developed in
the liver and then metastasized to other sites inside the liver and
to the mesentery, based on the most common EHAE site of origin and
the distribution and number of the lesions.
A case of hepatic EHAE metastasizing to the
mesentery was previously reported (6). In that case, there were multiple EHAE
lesions in the liver and the EHAE had also metastasized to the
peritoneum, omentum and mesentery, resulting in multiple organ
dysfunction syndrome. In the present case, several lesions were
identified in the liver but the only metastatic lesion was observed
in the mesentery. The mesenteric lesion and one of the hepatic
lesions were resected. As there were multiple hepatic lesions in
both the left and right lobes of the liver, the resection of all
the tumors was not feasible.
Epidemiologically, the estimated prevalence of EHAE
is <1/million (4). EHAEs present
mainly in the liver alone (21%), in the liver and the lung (18%),
in the lung alone (12%), or in the bone alone (14%) (7). Mehrabi et al reviewed 434 cases
of primary hepatic EHAE (8). The age
of the patients ranged from 3 to 86 years, with a mean age of 41.7
years, and the male:female ratio was 2:3., The major symptoms of
hepatic EHAE were upper abdominal pain, hepatomegaly and weight
loss, although the majority of the patients were asymptomatic at
the time of diagnosis. Of the hepatic EHAE patients, 87% exhibited
multifocal tumors that involved the bilateralliver lobes.
The patient presented herein was female,
asymptomatic, and had multifocal hepatic tumors with metastasis to
the mesentery. It has been reported that extrahepatic involvement
at the time of diagnosis is observed in 36.6% of hepatic EHAE
patients, and that the lung (8.5%), regional lymph nodes (8.5%),
peritoneum (6.1%), bone (4.9%), spleen (3.2%) and diaphragm (1.6%)
are the most common sites of extrahepatic involvement (8).
In the present case, extrahepatic involvement of the
mesentery was observed. These results suggest that hepatic EHAE may
easily metastasize to other sites of the liver, but do not readily
metastasize to other organs.
The patient was receiving estradiol dipropionate and
dydrogesterone for climacteric symptoms. Factors possibly involved
in the etiology of EHAE include oral contraceptives (9), vinyl chloride (10), asbestos (11), thorotrast (12), liver trauma (13), viral hepatitis (14), primary biliary cirrhosis (15) and alcohol-related hepatic disorders
(6). These findings suggest that
inflammation or female hormones may be associated with the
development of EHAE. It has been also reported that long-term
administration of female hormones, such as oral contraceptive
pills, is associated with the development of liver tumors (16).
Chromosomal and genetic abnormalities have also been
reported to be associated with EHAE (17–19).
Errani et al reported that the WWWTR1-CAMTA1 fusion
gene was present in EHAE, and that the same pattern of
WWWTR1-CAMTA1 fusion genes occurred in each tumor of each
patient with multiple EHEAs (18,19).
These results suggest that the WWWTR1-CAMTA1 fusion gene may
be associated with the development of EHEA, and that multiple EHAE
lesions may originate from a single lesion. Further research on the
association between EHAE and genetic abnormalities, as well as
other contributing factors, is required to optimize treatment.
In conclusion, we herein present a case of EHAE that
presented as multiple lesions in the liver and a lesion in the
mesentery, in a woman who had been receiving estradiol dipropionate
and dydrogesterone for several years. Approximately 3 years and 7
months have passed since the patient's first hospital visit; she
remains alive and the EHEA has not progressed. More effective
therapeutic options must be developed for EHAE in the future. This
case report was approved by the Ethics Committee of Toyooka
Hospital and the patient consented to the publication of the case
details and associated images.
Acknowledgements
The authors would like to thank Ms. H. Ogaki, Mr. K.
Nagaoka, Mr. T. Kuge, Mr. H. Takenaka and Ms. S. Eriguchi of the
Toyooka Hospital for their expert technical assistance. The Ethics
Committee of the Toyooka Hospital and the patient approved the
publication of this case report.
References
|
1
|
Weiss SW and Enzinger FM: Epithelioid
hemangioendothelioma: A vascular tumor often mistaken for a
carcinoma. Cancer. 50:970–981. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Makhlouf HR, Ishak KG and Goodman ZD:
Epithelioid hemangioendothelioma of the liver: A clinicopathologic
study of 137 cases Cancer. 85:562–582. 1999.
|
|
3
|
Dail DH and Liebow AA: Intravscular
bronchioloalveolar tumor. Am J Pathol. 78:6a–7a. 1975.
|
|
4
|
Lau K, Massad M, Pollak C, Rubin C, Yeh J,
Wang J, Edelman G, Yeh J, Prasad S and Weinberg G: Clinical
patterns and outcome in epithelioid hemangioendothelioma with or
without pulmonary involvement: Insights from an internet registry
in the study of a rare cancer. Chest. 140:1312–1318. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ishak KG, Sesterhenn IA, Goodman ZD, Rabin
L and Stromeyer FW: Epithelioid hemangioendothelioma of the liver:
A clinicopathologic and follow-up study of 32 cases. Hum Pathol.
15:839–852. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gurung S, Fu H, Zhang WW and Gu YH:
Hepatic epithelioid hemangioendothelioma metastasized to the
peritoneum, omentum and mesentery: A case report. Int J Clin Exp
Pathol. 8:5883–5889. 2015.PubMed/NCBI
|
|
7
|
Sardaro A, Bardoscia L, Petruzzelli MF and
Portaluri M: Epithelioid hemangioendothelioma: An overview and
update on a rare vascular tumor. Oncol Rev. 8:2592014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mehrabi A, Kashfi A, Fonouni H, Schemmer
P, Schmied BM, Hallscheidt P, Schirmacher P, Weitz J, Friess H,
Buchler MW and Schmidt J: Primary malignant hepatic epithelioid
hemangioendothelioma: A comprehensive review of the literature with
emphasis on the surgical therapy. Cancer 10Í7. 2108–2121. 2006.
View Article : Google Scholar
|
|
9
|
Dean PJ, Haggitt RC and O'Hara CJ:
Malignant epithelioid hemangioendothelioma of the liver in young
women. Relationship to oral contraceptive use. Am J Surg Pathol.
9:695–704. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Darras T, Moisse R and Colette JM:
Epithelioid hemangioendothelioma of the liver. J Belge Radiol.
71:722–723. 1988.PubMed/NCBI
|
|
11
|
de Man RA, Bac DJ, van Blankenstein M and
Zondervan PE: Sterile necrosis of the liver due to primary
epithelioid haemangio-endothelioma presenting as fever of
undetermined origin. Neth J Med. 45:25–29. 1994.PubMed/NCBI
|
|
12
|
Soslow RA, Yin P, Steinberg CR and Yang
GC: Cytopathologic features of hepatic epithelioid
hemangioendothelioma. Diagn Cytopathol. 17:50–53. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Banerjee B and Rennison A: Epitheloid
haemangioendothelioma of liver: A vascular tumour easily mistaken
for metastatic carcinoma on ultrasound imaging. Br J Radiol.
65:611–613. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Läuffer JM, Zimmermann A, Krähenbühl L,
Triller J and Baer HU: Epithelioid hemangioendothelioma of the
liver. A rare hepatic tumor. Cancer. 78:2318–2327. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Terada T, Hoso M, Kono N, Watanabe K and
Nakanuma Y: Epithelioid hemangioendothelioma of the liver in
primary biliary cirrhosis. A case report. Acta Pathol Jpn.
39:607–611. 1989.PubMed/NCBI
|
|
16
|
Kapp N and Curtis KM: Hormonal
contraceptive use among women with liver tumors: A systematic
review. Contraception. 80:387–390. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Boudousquie AC, Lawce HJ, Sherman R, Olson
S, Magenis RE and Corless CL: Complex translocation [7;22]
identified in an epithelioid hemangioendothelioma. Cancer Genet
Cytogenet. 92:116–121. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Errani C, Zhang L, Sung YS, Hajdu M,
Singer S, Maki RG, Healey JH and Antonescu CR: A novel WWTR1-CAMTA1
gene fusion is a consistent abnormality in epithelioid
hemangioendothelioma of different anatomic sites. Genes Chromosomes
Cancer. 50:644–653. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Errani C, Sung YS, Zhang L, Healey JH and
Antonescu CR: Monoclonality of multifocal epithelioid
hemangioendothelioma of the liver by analysis of WWTR1-CAMTA1
breakpoints. Cancer Genet. 205:12–17. 2012. View Article : Google Scholar : PubMed/NCBI
|