Introduction
Extramammary Paget's disease (EMPD) is a rare
malignant skin tumor, which is considered to originate from
cutaneous appendages and occurs in cutaneous areas bearing apocrine
glands, such as the scrotum, vulva and axilla (1,2).
Generally, the prognosis of EMPD is favorable if the primary lesion
is completely resected and no metastases are present (1,2).
However, the prognosis of the progressive and metastatic disease is
poor (1,2), and data on the efficacy of cytotoxic
chemotherapeutic agents in cases of advanced and/or metastatic EMPD
are limited (3).
Several studies indicated that the tumor cells
occasionally overexpress human epidermal growth factor receptor 2
(HER2) in patients with EMPD, at rates ranging from 15 to 65%
(4–9). The humanized monoclonal antibody
against HER2, trastuzumab, is expected to be effective in such
cases. Indeed, several cases of advanced EMPD that exhibited a good
response to trastuzumab, alone or combined with chemotherapy, were
reported (10–14). However, there is currently
insufficient evidence on the efficacy of treatment due to the
rarity of the disease itself. We herein describe a case of
HER2-positive and advanced vulvar EMPD, in which the primary tumor
mass and lymph node metastasis regressed with combined trastuzumab
and paclitaxel therapy for >2 years after initiation of
treatment. The clinical course of this case is reported, along with
a review of the relevant literature.
Case report
A 58-year-old woman was referred to the Shinshu
University Hospital (Matsumoto, Japan) in August 2014 to receive
further treatment for previously diagnosed EMPD. The findings of
the physical examinations of the chest and abdomen were
unremarkable, but a giant, slightly raised, erythematous and
hemorrhagic granular lesion in the perineum and a mass on the inner
thigh were identified (Fig. 1).
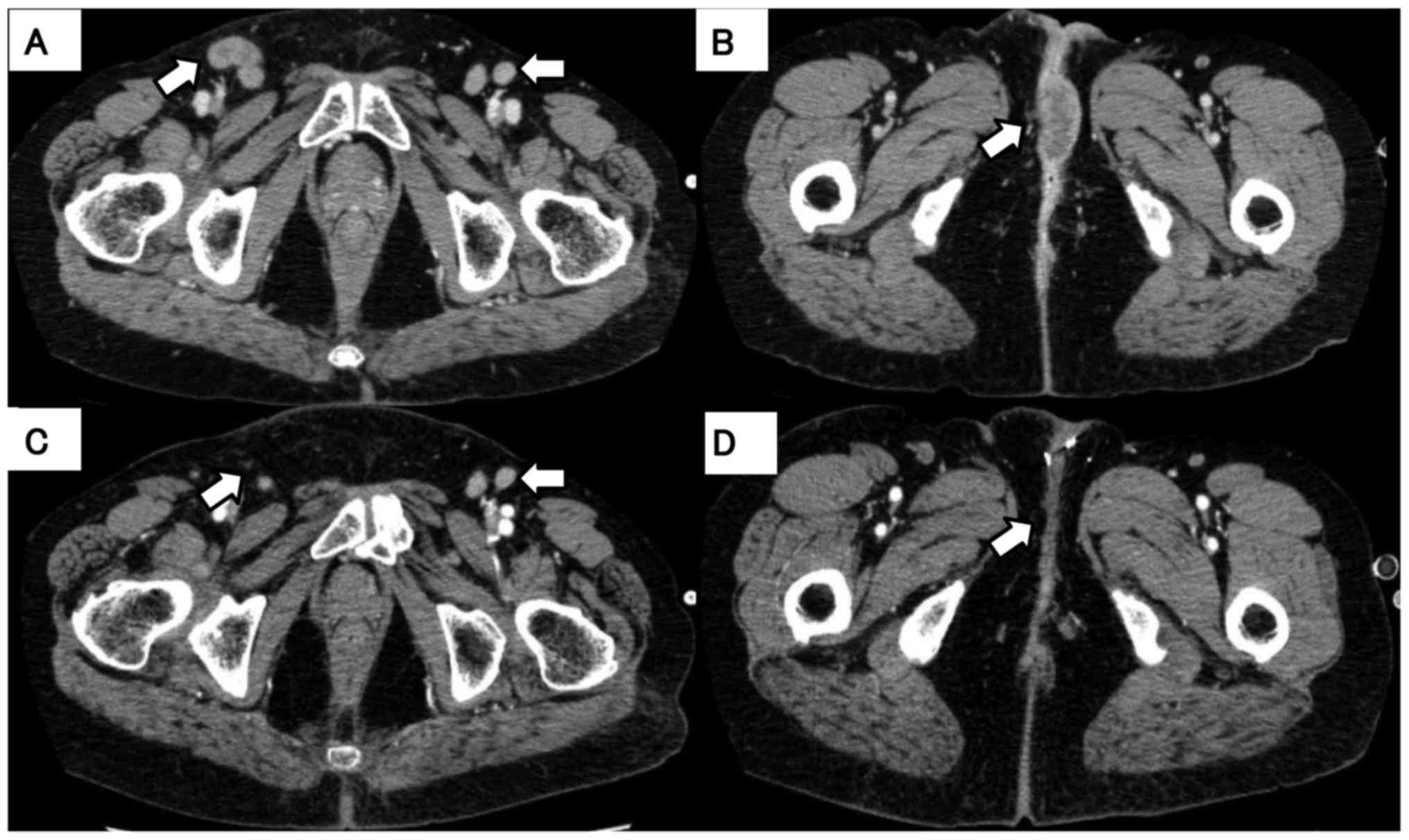
Lower abdominal computed tomography (CT) revealed enlargement of
the inguinal lesions, the mass in the perineum, and within the
vagina (Fig. 2, arrows). The disease
was initially diagnosed 12 years prior and the patient had
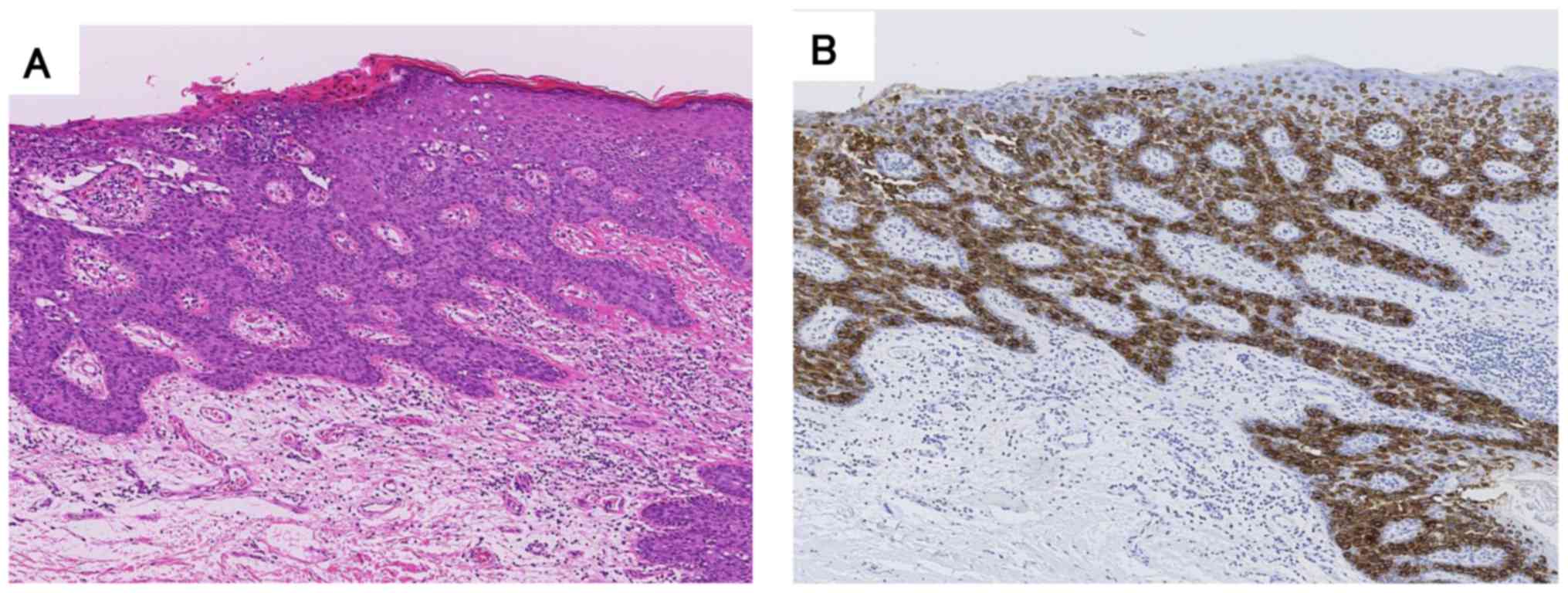
undergone simple vulvectomy. The histological and
immunohistochemical findings are presented in Fig. 3. However, the disease relapsed
locally within the subsequent 4 years and the patient underwent
vulvectomy twice and cystostomy. In addition, episioplasty was
performed for incontinence as a postoperative complication. Two
years after the last operation, the disease relapsed with a tumor
measuring 4 cm. The patient refused further surgical treatment and
was followed up. Four years later, the tumors had increased in size
and the patient experienced pain and difficulty walking; she was
then referred to our hospital to receive chemotherapy or
alternative therapy. The patient had a history of breast cancer
prior to the development of EMPD, which was completely resected,
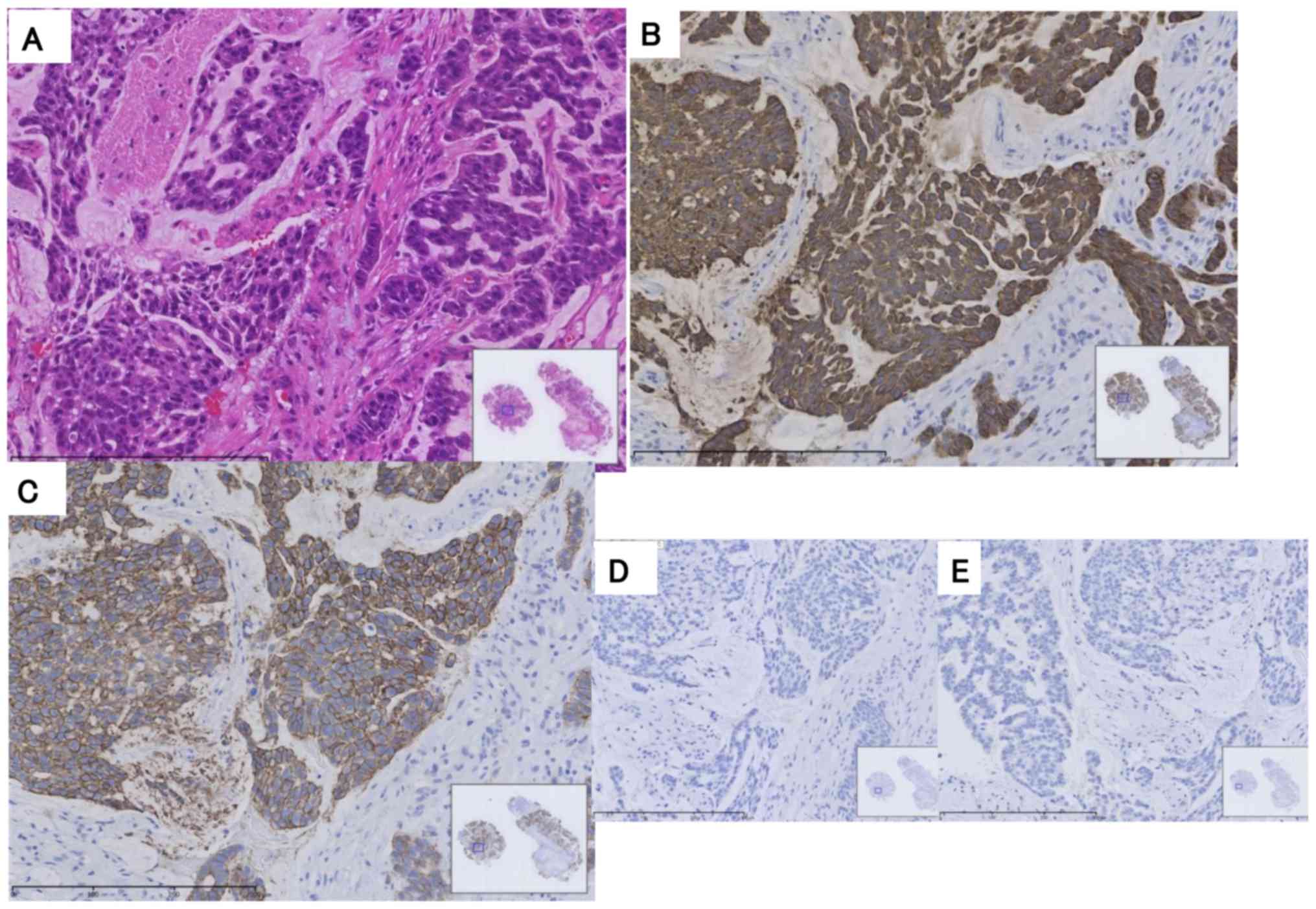
and has been followed up without any signs of relapse. Biopsy of
the vulval lesion was performed and the pathological findings
confirmed EMPD (Fig. 4A).
Immunohistochemical analysis revealed that tumor cells were
positive for HER2 and cytokeratin (CK) 7, and were negative for
estrogen and progesterone receptors (Fig. 4B-E).
The patient was treated with trastuzumab plus
paclitaxel. Trastuzumab was administered at a loading dose of 4
mg/kg followed by 2 mg/kg weekly in combination with weekly
paclitaxel at 80 mg/m2. No adverse effects, such as
cardiotoxicity, neurotoxicity, or hematotoxicity, have been
observed to date. The tumors decreased in size and the inguinal
lymph nodes disappeared 6 months after the initiation of
chemotherapy (Fig. 2C and D). This
treatment has been continued for 2 years and 6 months, with partial
response and good control of the clinical condition.
Discussion
We herein reported a case of HER2-positive advanced
EMPD that responded successfully to trastuzumab and paclitaxel
chemotherapy, achieving a prolonged disease-free period of >2
years after initiation of therapy. Kang et al (6) analyzed 246 Chinese male EMPD patients
and reported that HER2-positive EMPD was observed at a rate of
65.1% based on immunohistological staining. Richter et al
(7) also studied 39 patients with a
histologically confirmed diagnosis of vulvar EMPD and reported that
immunohistologically HER2-positive disease was observed in 58% of
the cases. Two Japanese studies reported HER2 overexpression in 16
of 104 cases (15%) and 7 of 34 cases (19.4%) (4,5). Thus,
the frequency of HER2 overexpression in Japanese patients appeared
to be lower compared with that in reports from other countries.
However, HER2 overexpression in these studies was correlated with
biologically aggressive EMPD, i.e., local invasion and lymph node
metastasis (4–9).
The patient presented herein had a history of
resected breast cancer. The immunohistological findings were
examined and the resected breast cancer was found to be negative
for HER2 and CK7, suggesting that the EMPD was not a distant
metastasis from the breast cancer and the biological profile was
different between breast cancer and EMPD in the present case.
EMPD is a rare cutaneous malignant tumor, and
analyses of HER2 overexpression or gene amplification in EMPD were
performed in previously reported patients with surgically resected
EMPD (4–9). Thus, there has been little clinical
experience with advanced or metastatic EMPD. Indeed, there have
been few reports regarding trastuzumab treatment in HER2-positive
advanced or metastatic EMPD, with only five case reports identified
in PubMed using the search terms ‘EMPD’ and ‘trastuzumab’ or ‘HER2’
(10–14). These previously reported cases are
summarized in Table I. All the
patients achieved a good response, but the observation time of
treatment varied widely. Three cases involved trastuzumab
monotherapy. It remains unclear whether the combination of
cytotoxic drugs is beneficial for overall survival,
progression-free survival, or response rate. Thus, further case
studies of trastuzumab treatment for HER2-positive advanced EMPD
are warranted, particularly focusing on the toxicities and/or time
to progression.
 | Table I.Previous cases of extramammary Paget's
disease treated with trastuzumab reported in the English
literature. |
Table I.
Previous cases of extramammary Paget's
disease treated with trastuzumab reported in the English
literature.
| Case | Age, years | Sex | Combination | Duration of
observation, months | Others | (Refs.) |
|---|
| 1 | 68 | Female | – | 12 |
| (10) |
| 2 | 71 | Male | – | 12 | Patient under
hemodialysis | (11) |
| 3 | 52 | Female | – | 12 |
| (12) |
| 4 | 70 | Female | Paclitaxel | 6 |
| (13) |
| 5 | 75 | Male | Docetaxel followed by
paclitaxel | 6 |
| (14) |
In summary, we herein described a case of advanced
EMPD with a long disease-free survival period of 2 years and 6
months after the initiation of combination therapy with trastuzumab
and paclitaxel. Our observations suggest that HER2 expression
should be determined in patients with advanced and/or metastatic
EMPD, and therapy with HER2 inhibitors should be considered as an
option for the treatment of HER2-positive EMPD.
The patient provided written informed consent
regarding the publication of the case details and associated
images.
References
|
1
|
Kyriazanos ID, Stamos NP, Miliadis L,
Noussis G and Stoidis CN: Extra-mammary Paget's disease of the
perianal region: A review of the literature emphasizing the
operative management technique. Surg Oncol. 20:e61–e71. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parker LP, Parker JR, Bodurka-Bevers D,
Deavers M, Bevers MW, Shen-Gunther J and Gershenson DM: Paget's
disease of the vulva: Pathology, pattern of involvement, and
prognosis. Gynecol Oncol. 77:183–189. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tokuda Y, Arakura F and Uhara H:
Combination chemotherapy of low-dose 5-fluorouracil and cisplatin
for advanced extramammary Paget's disease. Int J Clin Oncol.
20:194–197. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tanaka R, Sasajima Y, Tsuda H, Namikawa K,
Tsutsumida A, Otsuka F and Yamazaki N: Human epidermal growth
factor receptor 2 protein overexpression and gene amplification in
extramammary Paget disease. Br J Dermatol. 168:1259–1266. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ogawa T, Nagashima Y, Wada H, Akimoto K,
Chiba Y, Nagatani T, Inayama Y, Yao M, Aoki I and Ikezawa Z:
Extramammary Paget's disease: Analysis of growth signal pathway
from the human epidermal growth factor receptor 2 protein. Hum
Pathol. 36:1273–1280. 2005.PubMed/NCBI
|
|
6
|
Kang Z, Zhang Q, Zhang Q, Li X, Hu T, Xu
X, Wu Z, Zhang X, Wang H, Xu J, et al: Clinical and pathological
characteristics of extramammary Paget's disease: Report of 246
Chinese male patients. Int J Clin Exp Pathol. 8:13233–13240.
2015.PubMed/NCBI
|
|
7
|
Richter CE, Hui P, Buza N, Silasi DA,
Azodi M, Santin AD, Schwartz PE and Rutherford TJ: HER-2/NEU
overexpression in vulvar Paget disease: The Yale experience. J Clin
Pathol. 63:544–547. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Keatings L, Sinclair J, Wright C, Corbett
IP, Watchorn C, Hennessy C, Angus B, Lennard T and Horne CH:
c-erbB-2 oncoprotein expression in mammary and extramammary Paget's
disease: An immunohistochemical study. Histopathology. 17:243–247.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Plaza JA, Torres-Cabala C, Ivan D and
Prieto VG: HER-2/neu expression in extramammary Paget disease: A
clinicopathologic and immunohistochemistry study of 47 cases with
and without underlying malignancy. J Cutan Pathol. 36:729–733.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wakabayashi S, Togawa Y, Yoneyama K,
Suehiro K, Kambe N and Matsue H: Dramatic cinical response of
relapsed metastatic extramammary Paget's disease to trastuzumab
monotherapy. Case Rep Dermatol Med. 2012:4013622012.PubMed/NCBI
|
|
11
|
Barth P, Dulaimi Al-Saleem E, Edwards KW,
Millis SZ, Wong YN and Geynisman DM: Metastatic extramammary
Paget's disease of scrotum responds completely to single agent
trastuzumab in a hemodialysis patient: Case report, molecular
profiling and brief review of the literature. Case Rep Oncol Med.
2015:8951512015.PubMed/NCBI
|
|
12
|
Karam A, Berek JS, Stenson A, Rao J and
Dorigo O: HER-2/neu targeting for recurrent vulvar Paget's disease
A case report and literature review. Gynecol Oncol. 111:568–571.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hanawa F, Inozume T, Harada K, Kawamura T,
Shibagaki N and Shimada S: A case of metastatic extramammary
Paget's disease responding to trastuzumab plus paclitaxel
combination therapy. Case Rep Dermatol. 3:223–227. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Takahagi S, Noda H, Kamegashira A,
Madokoro N, Hori I, Shindo H, Mihara S and Hide M: Metastatic
extramammary Paget's disease treated with paclitaxel and
trastuzumab combination chemotherapy. J Dermatol. 36:457–461. 2009.
View Article : Google Scholar : PubMed/NCBI
|