Introduction
Hepatocellular carcinoma (HCC) is the sixth most
common cancer worldwide in terms of number of cases (626,000, or
5.7% of new cancer cases) and it is the third most common cause of
death from cancer (1). There are a
variety of treatment guidelines for liver cancer, and their
applicability in individual cases depends on the tumor stage
(2–4).
Transarterial chemoembolization (TACE) is
recommended for the treatment of unresectable HCC. TACE is a
palliative rather than curative treatment. It can be carried out
repeatedly for unresectable HCC, but if the effect is judged to be
poor, or TACE-refractory, introduction of sorafenib is considered
(5,6). However, the safety and efficacy of
early sorafenib induction after TACE has yet to be established.
In the present study, we evaluated the safety and
efficacy of sorafenib therapy within three weeks after a second
TACE treatment was performed due to recurrence within six months of
the first TACE procedure.
Patients and methods
Study design
This prospective study initially enrolled 17
patients whose tumors were treated with sorafenib post-TACE from
July 2011 to March 2013 at Kagoshima University Hospital and
Kagoshima Teishin Hospital. For the final analysis we selected the
11 patients who met the following inclusion criteria: (1) Classification by the Barcelona clinic
liver cancer (BCLC) staging system (3) of stage B disease, which is generally
not considered an indication for curative-intent treatment;
(2) Eastern Cooperative Oncology
Group performance status 0–1; (3)
Child-Pugh grade A; and (4)
progressive disease (PD), confirmed within six months after being
treated with TACE. Exclusion criteria were as follows: (1) liver transplants at any time; (2) only nodal or distant metastases without
viable lesions in the liver; (3)
secondary malignancies; and (4) a
history of concomitant use of some other targeting agent,
chemotherapy, and immunotherapy.
All the patients were informed of the advantages and
disadvantages of the treatment options, including treatment
outcomes, treatment-related morbidities, and costs. The final
treatment decision was made jointly by each patient and his/her
physician, with full respect for the patient's option to decline
participation. The study protocol conformed to the ethical
guidelines of the World Medical Association Declaration of Helsinki
and was approved by the ethics committees of Kagoshima University
Medical and Dental Hospital and Kagoshima Teishin Hospital
(approval no. 23-53). All the cases were judged to have PD within
six months after TACE, and sorafenib administration was started
within three weeks after the second TACE treatment.
Of 113 patients who underwent initial TACE for HCC
in Child-Pugh grade A and BCLC Stage B from January 1995 to January
2013 at Kagoshima University Hospital, 23 patients who were treated
by TACE alone were selected, and the interval between the third
TACE to the second was <6 months (TACE alone group). We
calculated TTP in the fourth TACE with the third and compared each
group.
Evaluation of outcomes
Time to progression (TTP) based on the modified
Response Evaluation Criteria in Solid Tumors (mRECIST) (7) was the primary endpoint of the analysis.
The secondary endpoints were overall survival (OS), which was
defined as the time from enrolment to death from any cause or to
the last follow-up in censored patients, and treatment-related
adverse events (AEs), which were assessed using the Common
Terminology Criteria for AEs (CTCAE) version 4.0. (8).
Treatment protocol
TACE
We performed TACE using the Seldinger technique
according to the following protocol. After a 3.5- or 4-Fr-sheath
(Medikit Super Sheath; Medikit, Tokyo, Japan) was introduced into
the femoral artery, a 3.5- or 4-Fr preshaped catheter (Selecon-PA
Catheter; Terumo, Gifu, Japan) was inserted into a superior
mesenteric artery and 30–40 ml of 50% iopamidol (Iomeron 350;
Eisai, Osaka, Japan) was injected. Computed tomographic arterial
portography was performed to determine whether there were one or
more HCC lesions, and to assess the patency of the portal vein.
Computed tomographic arteriography was then performed to detect
HCC, and 15–20 ml of 50% iopamidol was injected via a common
hepatic artery. Additionally, we selectively placed a 2-Fr
microcatheter in the tumor-bearing artery of the HCC (nutrient
artery), and injected an emulsified formulation of iodized oil
(Lipiodol; Laboratoire Guerbet, AulnaySous-Bois, France) along with
the following three anti-cancer agents: i) 20 mg epirubicin
hydrochloride (Farmorubicin; Pfizer Japan, Tokyo, Japan) and 4 mg
mitomycin C (Kyowa-Kirin, Tokyo, Japan); ii) miriplatin hydrate
(Miripla®, Dainippon Sumitomo Pharma, Tokyo, Japan); and
iii) cisplatin (Nihon-Kayaku, Tokyo, Japan). After injecting the
emulsified formulation, we injected gelatin sponge particles
(Gelpart®, Nippon Kayaku, Tokyo, Japan) as an embolus
into the same location. We performed hepatic arteriography after
the embolus injection to confirm the loss of blood flow to the
tumor through the nutrient artery before performing the surgery.
Sorafenib was administered within one to three weeks after
TACE.
Re-TACE followed by sorafenib
All the patients were given detailed information
regarding sorafenib after TACE treatment, including its efficacy
and potential AEs. Patients received oral sorafenib (400 or 200 mg)
twice daily after TACE, except for those with a contraindication to
sorafenib treatment (e.g., insufficient liver function). For
patients treated with sorafenib after TACE, the efficacy of the
combined treatment was assessed using dynamic CT or MR imaging of
the liver 6–8 weeks after treatment.
Clinical characteristics of patients and
laboratory markers. The following patient clinical
characteristics and laboratory markers were assessed: age; sex;
tumor size; observation period; previous treatment; viral markers,
including hepatitis B virus (HBV), hepatitis C virus (HCV), and
NBNC [HBV (−) and HCV (−)]; hepatic function assessed using
Child-Pugh grades based on both clinical (ascites and
encephalopathy) and laboratory (serum albumin, total bilirubin and
prothrombin time) parameters; body mass index (BMI); aspartate
transaminase (AST); alanine aminotransferase (ALT); γ-glutamyl
transpeptidase (γ-GTP); serum albumin; total bilirubin; prothrombin
time; platelets; α-fetoprotein (AFP); and des-γ-carboxy prothrombin
(DCP).
During follow-up, the levels of AST, AST, γ-GTP,
serum albumin, total bilirubin, prothrombin time, platelets, AFP,
and DCP were determined every 4–6 weeks to evaluate liver function.
As mentioned above, dynamic liver CT or MR imaging was performed
every 6–8 weeks after treatment to evaluate the response.
Statistical analysis
Statistical analyses were performed using the
χ2-test or the Mann-Whitney U test, as appropriate. The
Kaplan-Meier method was used to estimate cumulative survival and
time to progression of local and other tumors. To ensure patient
safety, the dose of sorafenib was reduced or treatment was delayed
or temporarily discontinued when we observed clinically significant
toxicity (≥grade 3) based on the National Cancer Institute's CTCAE
version 4.0 (8) or at the
physician's discretion. P<0.05 was regarded as statistically
significant. All the statistical analyses were conducted using IBM
SPSS Statistics v. 20 (IBM SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics and rates of
TTP and OS in the 11 patients
Eleven patients met the aforementioned inclusion
criteria. Table I summarizes the
baseline clinical characteristics of the 11 patients treated with
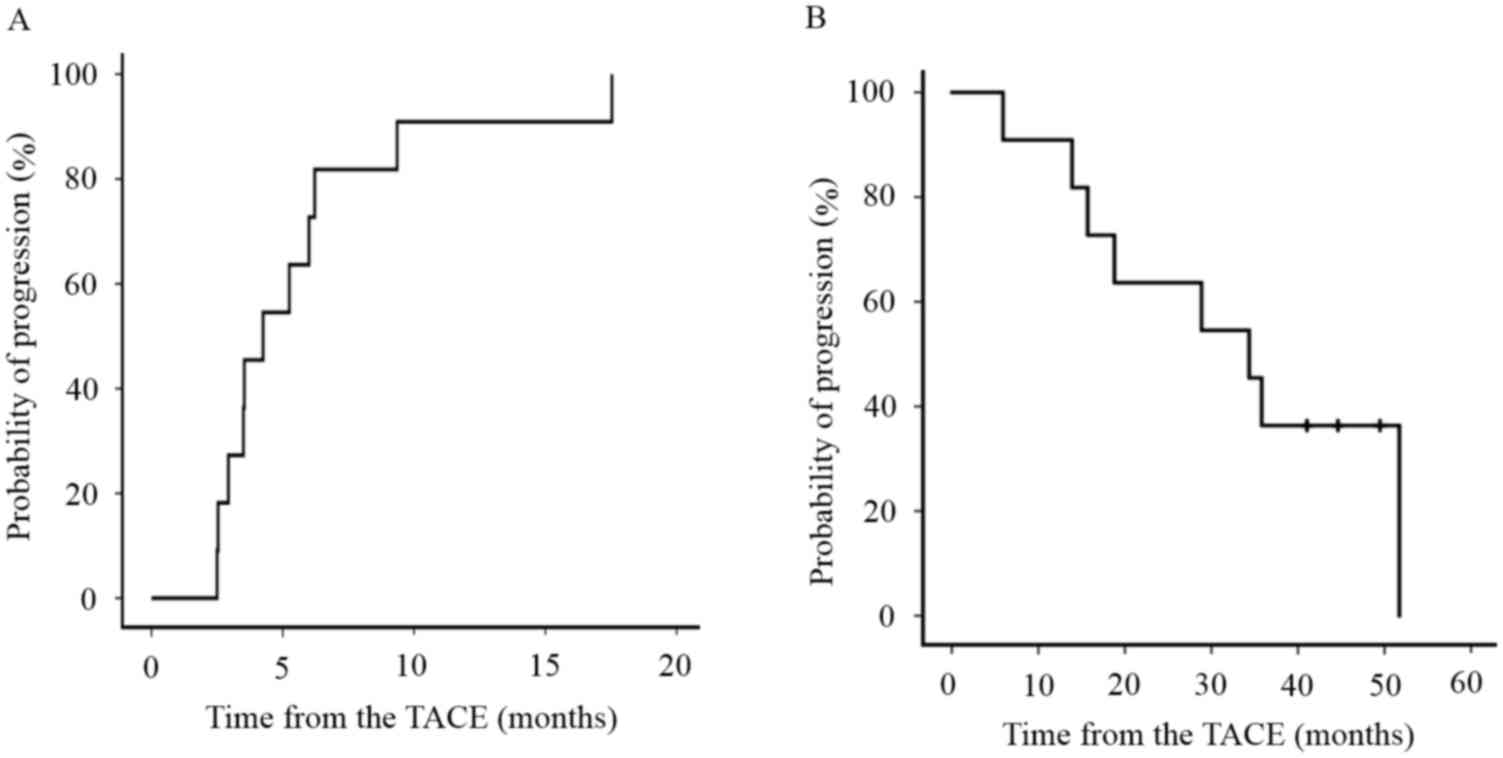
sorafenib after TACE for HCC. The median TTP of all the patients
during the follow-up period was 3.9 months (median range, 2.3–16.1)
(Fig. 1A) and the median OS of all
patients was 34.4 months (median range, 5.9–51.7) (Fig. 1B). The median underlying cause of HCC
was HBV in two patients, HCV in six patients, and NBNC in three
patients. The ECOG performance score was 0 in nine patients and 1
in one patient. Nine patients had chronic hepatitis and three had
liver cirrhosis. All the patients were Child-Pugh grade A. LCSGJ
stage was II in two patients and III in nine patients. AFP was 7.3
ng/ml (median range, 3.5–188 ng/ml) and DCP was 24.0 mAU/ml (median
range, 8–3589 mAU/ml). All the patients had pretreatment for HCC.
The initial sorafenib dose was 800 mg in nine patients and 400 mg
in two patients.
 | Table I.Baseline sorafenib after TACE
patient's characteristics. |
Table I.
Baseline sorafenib after TACE
patient's characteristics.
| Patient's
characteristics | All patients
(n=11) |
|---|
| Age (years), median
(range) | 70.6±7.5 |
| Gender |
|
| Male | 10 (90.9) |
|
Female | 1 (9.1) |
| TTP,
months | 3.9 (2.3–16.1) |
| OS,
months | 34.4 (5.9–51.7) |
| Underlying cause |
|
| HBV | 2 (18.2) |
| HCV | 6 (54.5) |
| NBNC | 3 (27.3) |
| ECOG performance
score |
|
| 0 | 10 (90.9) |
| 1 | 1 (9.1) |
| Child-Pugh score |
|
| A | 11 (100.0) |
| B | 0 (0.0) |
| C | 0 (0.0) |
| LCSGJ staging |
|
| II | 2 (18.2) |
| III | 9 (91.8) |
| AFP,
ng/ml | 7.3 (3.5–188.0) |
| DCP,
mAU/ml | 24.0
(8.0–3589.0) |
| Pretreatment HCC |
|
| Yes | 11 (100.0) |
| No | 0 (0.0) |
| Initial sorafenib
dose, mg |
|
| 800 | 9 (91.8) |
| 400 | 2 (18.2) |
Rates of TTP and OS in HCC patients
treated with sorafenib after TACE for more or less than 4 months,
and with TACE alone
Table II summarizes
the baseline clinical characteristics of the HCC patients treated
with sorafenib after TACE for more than 4 months, less than 4
months, and TACE alone.
 | Table II.Baseline clinical characteristics of
HCC patients treated with sorafenib after TACE for more than 4
months, less than 4 months, and with TACE alone. |
Table II.
Baseline clinical characteristics of
HCC patients treated with sorafenib after TACE for more than 4
months, less than 4 months, and with TACE alone.
| Patient
characteristic | Sorafenib after TACE
group (n=11) |
|
|---|
|
|
|
|---|
| Period of
sorafenib | <4 months
(n=6) | 4 months ≦ (n=5) | TACE alone group
(n=23) |
|---|
| Age, years | 72.8±6.4 | 68.0±8.6 | 67.4 ± 8.5 |
| Sex |
|
|
|
| Male | 6 (100.0) | 4 (80.0) | 16 (69.6) |
|
Female | 0 (0.0) | 1 (20.0) | 7 (30.4) |
| TTP,
months | 3.0 (2.3–3.9) | 5.7 (4.8–16.1) | 4.3 (0.7-
24.0) |
| OS,
months | 17.2
(5.9–38.9) | 35.9
(28.9–49.5) | – |
| Underlying
cause |
|
|
|
|
HBV | 1 (16.7) | 1 (20.0) | 1 (4.3) |
|
HCV | 4 (66.6) | 2 (40.0) | 21 (83.3) |
|
NBNC | 1 (16.7) | 2 (40.0) | 1 (4.3) |
| Child-Pugh
score |
|
|
|
| A | 6 (100.0) | 5 (100.0) | 23 (100.0) |
| B | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| C | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| LCSGJ staging |
|
|
|
| II | 1 (16.7) | 1 (20.0) | 10 (43.5) |
|
III | 5 (83.3) | 4 (80.0) | 13 (56.5) |
| AFP,
ng/ml | 12.1
(3.5–137.0) | 7.3
(4.9–188.0) | 110.0 (1.7-
67996.0) |
| DCP,
mAU/ml | 41.0
(15.0–3589.0) | 20.0
(8.0–67.0) | 29.0 (11.0-
7200.0) |
| Pretreatment
HCC |
|
|
|
|
Yes | 6 (100.0) | 5 (100.0) | 30 (100.0) |
| No | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sorafenib, mg |
|
|
|
|
800 | 3 (50.0) | 5 (100.0) | – |
|
400 | 3 (50.0) | 0 (0.0) | – |
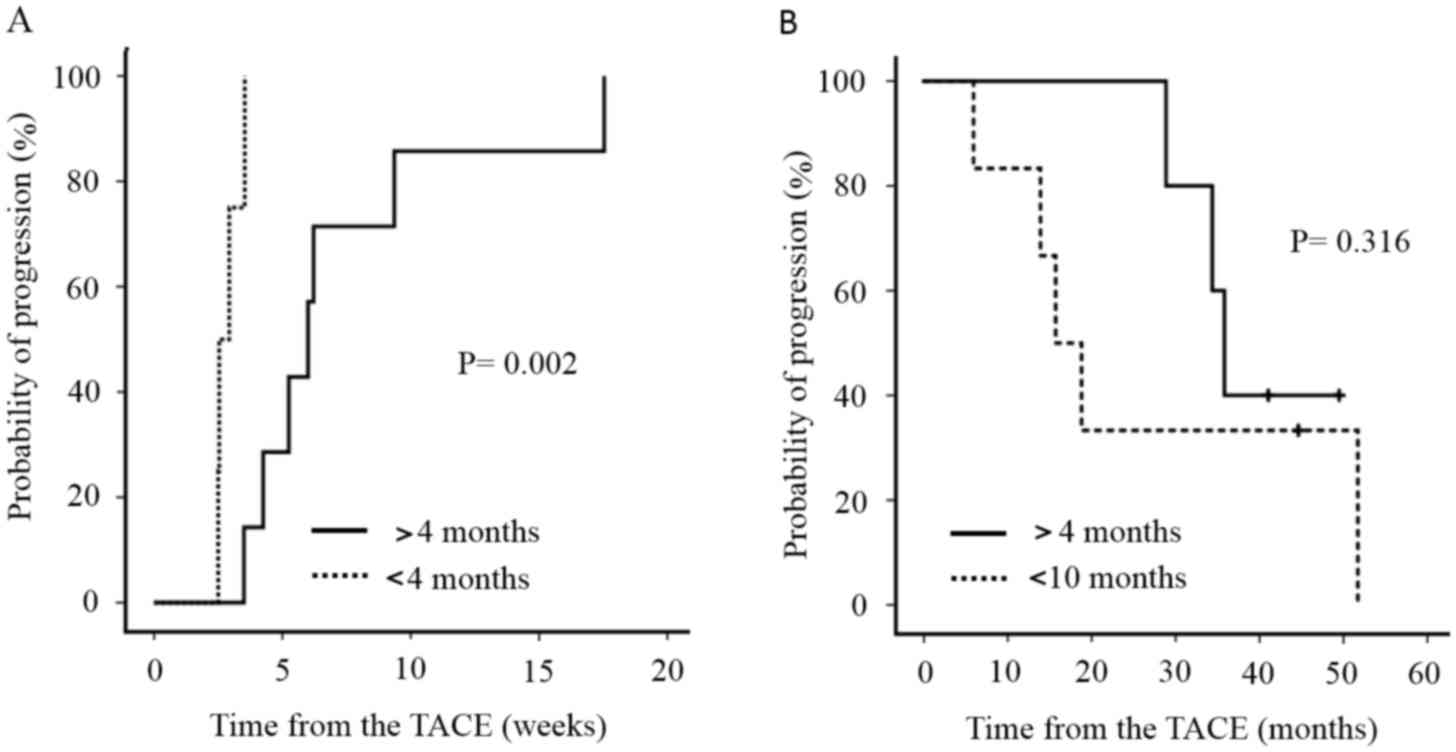
We divided the patients into two groups based on
whether sorafenib was administered for more or less than 4 months.
TTP in patients treated with sorafenib for >4 months was 5.7
months (median range, 4.8–16.1), while that in patients receiving
sorafenib for <4 months was 3.0 months (median range, 2.3–3.9),
indicating a significant difference (P=0.002) (Fig. 2A). OS in patients treated with
sorafenib for >4 months was 35.9 (median range, 28.9–49.5)
months, while that in patients receiving sorafenib for <4 months
was 17.2 months (median range, 5.9–38.9). There was no significant
difference in OS between the two groups (Fig. 2B). In the TACE alone group, the
interval (TTP) between the third and fourth TACE treatments was 4.3
months (range, 0.7–24.0). Thus, TTP decreased among the groups in
the following order: Sorafenib for more than 4 months > TACE
alone > sorafenib for <4 months.
Treatment-related AEs
Treatment-related AEs, which were assessed using the
CTCAE version 4.0, (8) are shown in
Table III. The most common AEs
were hand-foot skin reactions (27%); these occurred at grade 1 (G1)
in seven patients and G2 in three patients. The second most common
AE was hypertension (10.8%), which occurred at G1 in two patients
and G2 in two patients. One patient each had G3 increased serum
amylase, decreased platelet count and white blood cells. In
Table IV, AEs are divided into two
groups based on whether they initially developed within 2 weeks of
the start of sorafenib treatment or >2 weeks later. Hand-foot
skin reactions occurred in each group, whereas hypertension was
only observed within 2 weeks. The G3 increased serum amylase and
decreased G3 white blood cells occurred within 2 weeks, whereas the
G3 decreased platelet count occurred after >2 weeks. Total
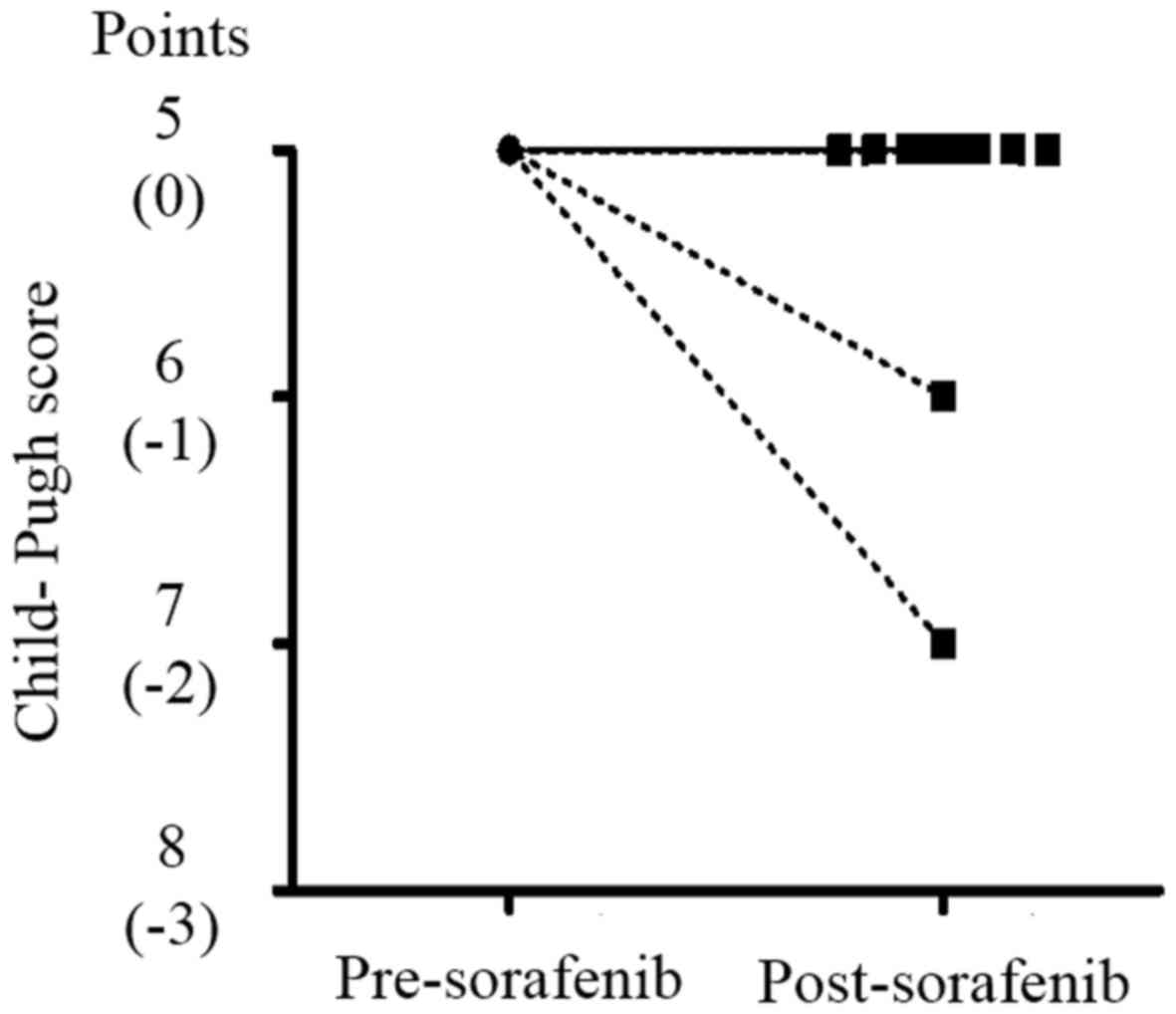
Child-Pugh scores decreased in only two patients by the end of
sorafenib treatment (Fig. 3), but
these improved immediately after sorafenib administration was
stopped.
 | Table III.Drug-related, treatment-emergent
adverse events. |
Table III.
Drug-related, treatment-emergent
adverse events.
| AE | Grade 1 n=23 | Grade 2 n=11 | Grade 3 n=3 | Total n (%) |
|---|
| Hand-foot skin
reaction | 7 (30.4) | 3 (27.2) | 0 (0.0) | 10 (27.0) |
| Diarrhea | 3 (13.0) | 0 (0.0) | 0 (0.0) | 3 (8.1) |
| Alopecia | 3 (13.0) | 0 (0.0) | 0 (0.0) | 3 (8.1) |
| Pruritus | 2 (8.7) | 0 (0.0) | 0 (0.0) | 2 (5.4) |
| Hypertension | 2 (8.7) | 2 (18.2) | 0 (0.0) | 4 (10.8) |
| Hoarseness | 2 (8.7) | 0 (0.0) | 0 (0.0) | 2 (5.4) |
| Serum amylase
increased | 1 (4.3) | 1 (9.0) | 1 (33.3) | 3 (8.1) |
| Platelet count
decreased | 1 (4.3) | 1 (9.0) | 1 (33.3) | 3 (8.1) |
| Hepatobiliary
disorders | 1 (4.3) | 1 (9.0) | 0 (0.0) | 2 (5.4) |
| Anorexia | 1 (4.3) | 0 (0.0) | 0 (0.0) | 1 (5.4) |
| White blood cell
decreased | 0 (0.0) | 1 (9.0) | 1 (33.3) | 2 (5.4) |
| Blood bilirubin
increased | 0 (0.0) | 1 (9.0) | 0 (0.0) | 1 (2.7) |
| Acute coronary
syndrome | 0 (0.0) | 1 (9.0) | 0 (0.0) | 1 (2.7) |
 | Table IV.Drug-related adverse events within 2
weeks or more than 2 weeks after initiating sorafenib
treatment. |
Table IV.
Drug-related adverse events within 2
weeks or more than 2 weeks after initiating sorafenib
treatment.
| Within 2 weeks | More than 2
weeks |
|---|
|
|
|---|
| AE | Any Grade
(n=21) | AE | Any Grade
(n=15) |
|---|
| Hand-foot skin
reaction | 5 (23.8) | Hand-foot skin
reaction | 5 (33.3) |
| Hypertension | 4 (19.0) | Diarrhea | 3 (20.0) |
| Serum amylase
increased | 3 (14.3) | Alopecia | 3 (20.0) |
| Hoarseness | 2 (9.5) | Platelet count
decreased | 1 (6.7) |
| White blood cell
decreased | 2 (9.5) | Blood bilirubin
increased | 1 (6.7) |
| Acute coronary
syndrome | 1 (4.8) | Hepatobiliary
disorders | 1 (6.7) |
| Anorexia | 1 (4.8) | Pruritus | 1 (6.7) |
| Hepatobiliary
disorders | 1 (4.8) |
|
|
| Platelet count
decreased | 1 (4.8) |
|
|
| Pruritus | 1 (4.8) |
|
|
Discussion
The present study investigated a loco-regional
control of early induction of sorafenib after transarterial
chemoembolization for unresectable hepatocellular carcinoma in
relapsed patients within six months after the TACE procedure. We
evaluated how early induction of sorafenib after TACE contributes
to prolonging the interval between TACE treatments (TTP). TTP in
patients treated with sorafenib for >4 months was 5.7 months and
<4 months was 3.0 months. TTP in patients treated with sorafenib
for >4 months was significantly higher than that. OS in patients
treated with sorafenib for >4 months was 35.9 months and for
<4 months was 17.2 months. There was no significant difference
in OS between the two groups. In the TACE alone group, the interval
(TTP) between the third and the fourth TACE treatments was 4.2
months. Sorafenib administered for >4 months resulted in longer
TTP than TACE alone. In addition, early induction of sorafenib
after TACE within three weeks was identified; however, only two
patients experienced mild reduction in liver reserve function
during the course of sorafenib treatment, but we did not observe
any other severe AEs, only G1 and G2 hand-foot skin reactions
(27.0%) and hypertension (10.8%) were observed. We considered
sorafenib after TACE was generally well tolerated.
TACE is recommended for unresectable HCC by the
Japan Society of Hepatology Consensus-Based Clinical Practice
Guidelines for the management of HCC (2) and intermediate BCLC stages (3). Ikeda et al reported that the
median OS of patients with unresectable HCC was 3.1 years, the
one-year OS was 89.9%, and the two-year OS was 75.0% (9). There were no significant differences
between Japanese and Korean patients. The use of TACE is beneficial
in patients with intermediate stage HCC, but TACE is a palliative
treatment. When TACE is performed repeatedly, its effect can
gradually wane as patients become refractory (10). The treatment of TACE-refractory
patients is controversial and there is no globally established
approach to the problem. Several studies have reported the
beneficial effects of sorafenib for TACE-refractory patients, and
the relatively early administration of sorafenib extended overall
survival (5,6,11). The
development of sorafenib as a systemic chemotherapy is essential
for patients who have no choice but to repeat TACE. However, a
phase III clinical trial in the Asia-Pacific region revealed that
the median TTP was 2.8 months and the median OS was only 6.5 months
in HCC patients with sufficient liver function who were treated
with sorafenib after TACE (12).
Currently, local treatments, i.e., TACE and
radiofrequency ablation, have been shown to induce the production
of VEGF (13–16), which may facilitate disease
progression and metastasis. Additionally, VEGF is elevated after
TACE, but to a lesser extent in patients who respond more poorly to
TACE therapy (17). Sorafenib
monotherapy appears to be inferior to TACE in terms of local
control of HCC; however, the antiangiogenic and antiproliferative
effects of sorafenib may inhibit VEGF production and multikinase
signaling and prevent angiogenesis when administered after TACE
(17–19). We planned this study with this
background in mind, and expected prolongation of TTP and OS. There
have been several trials based on the same concept, namely the
antiangiogenic and antiproliferative effects of sorafenib after
TACE. A double-blind and placebo-controlled phase III trial from
Japan and Korea, the so-called post-TACE trial (20), found that the addition of sorafenib
provided no additional benefit to TTP in HCC patients who responded
to TACE. One of the most significant problems with this trial was
that the median duration from TACE to the onset of sorafenib
therapy was 9.3 weeks. Previous findings have shown that the
transient elevation of VEGF occurs within seven days after TACE
therapy (14,15). Therefore, it is unlikely that
sorafenib contributed to TTP and OS as sorafenib was introduced
after the seventh day. We took this into consideration and
sorafenib was initially administered within three weeks of TACE in
this study. We used a single-arm prospective design, and used
historical data as controls (in other words, patients with
intermediate BCLC Stage and less than six months between the second
and third TACE) for comparison to TTP between the third and fourth
TACE treatments. Patients who took sorafenib for more than 4 months
demonstrated significantly longer TTP than those who received TACE
alone.
There was concern about AEs given the short duration
between TACE and the introduction of sorafenib, but the combination
of these treatments was well tolerated and did not appear to lead
to worse AEs than were observed with either TACE or sorafenib
therapy alone. While a previous combination trial reported a higher
incidence of AEs when TACE was administered before sorafenib
(20), and a European study
evaluating the combination of TACE and sorafenib was stopped
prematurely because of safety concerns (21), the AE profile and incidence observed
in this study were similar to those in several trials of TACE plus
sorafenib combination therapy (22,23), and
did not differ from those observed in the SHARP (24) and Asia-Pacific (12) sorafenib-only trials. In this study,
the most common AE was hand-foot skin reaction, occurring in 27% of
patients, and the second most common was hypertension, experienced
by 10.8% of patients. Moreover, the AE profile differed slightly
depending on whether sorafenib was administered within two weeks or
after two weeks, but severe reactions were not observed in either
case. Sorafenib eventually became ineffective in all the patients
in this study; however, only two cases demonstrated mild declines
in liver reserve, and the remainder maintained their baseline
Child-Pugh scores after they stopped taking sorafenib. All the
patients were able to undergo further TACE after sorafenib
discontinuation because sufficient liver reserve function was
maintained.
This clinical study was useful because of its
prospective nature, as many previous reports have used a
retrospective design. Nevertheless, there were some limitations to
our study. First, our sample size was relatively small. Since the
efficacy, side effects, and cost-benefit of sorafenib after TACE
were unknown because of the prospective nature of the study, we
could not obtain informed consent from many patients. Second, this
was not a placebo-controlled randomized clinical trial. Ideally, a
phase III clinical trial is needed with appropriate controls to
avoid selection bias. However, it is relatively difficult to
recruit patients to a placebo-controlled randomized clinical trial
within a reasonable time period.
In conclusion, the use of sorafenib in combination
with TACE significantly improved TTP and OS in patients with
intermediate HCC. Further studies are needed to confirm the safety
and efficacy of this combination therapy.
Acknowledgements
The English language service Zenis™ aided in the
preparation of the current study manuscript for publication.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kudo M, Matsui O, Izumi N, Iijima H,
Kadoya M, Imai Y, Okusaka T, Miyayama S, Tsuchiya K, Ueshima K, et
al: JSH consensus-based clinical practice guidelines for the
management of hepatocellular carcinoma: 2014 update by the liver
cancer study group of Japan. Liver Cancer. 3:458–468. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
European Association For The Study Of The
Liver1, . European Organisation For Research And Treatment Of
Cancer: EASL-EORTC clinical practice guidelines: Management of
hepatocellular carcinoma. J Hepatol. 56:908–943. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bruix J and Sherman M: American
Association for the Study of Liver Diseases: Management of
hepatocellular carcinoma: An update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ogasawara S, Chiba T, Ooka Y, Kanogawa N,
Motoyama T, Suzuki E, Tawada A, Kanai F, Yoshikawa M and Yokosuka
O: Efficacy of sorafenib in intermediate-stage hepatocellular
carcinoma patients refractory to transarterial chemoembolization.
Oncology. 87:330–341. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Arizumi T, Ueshima K, Minami T, Kono M,
Chishina H, Takita M, Kitai S, Inoue T, Yada N, Hagiwara S, et al:
Effectiveness of sorafenib in patients with transcatheter arterial
chemoembolization (TACE) refractory and intermediate-stage
hepatocellular carcinoma. Liver Cancer. 4:253–262. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lencioni R and Llovet JM: Modified RECIST
(mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis.
30:52–60. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
NCI common terminology criteria for
adverse events (CTCAE) v.4 data files. http://evs.nci.nih.gov/ftp1/CTCAE/About.htmlMay
14–2015
|
|
9
|
Ikeda M, Arai Y, Park SJ, Takeuchi Y, Anai
H, Kim JK, Inaba Y, Aramaki T, Kwon SH, Yamamoto S, et al:
Prospective study of transcatheter arterial chemoembolization for
unresectable hepatocellular carcinoma: An Asian cooperative study
between Japan and Korea. J Vasc Interv Radiol. 24:490–500. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kudo M, Matsui O, Izumi N, Kadoya M,
Okusaka T, Miyayama S, Yamakado K, Tsuchiya K, Ueshima K, Hiraoka
A, et al: Transarterial chemoembolization failure/refractoriness:
JSH-LCSGJ criteria 2014 update. Oncology. 87 Suppl 1:S22–S31. 2014.
View Article : Google Scholar
|
|
11
|
Ikeda M, Mitsunaga S, Shimizu S, Ohno I,
Takahashi H, Okuyama H, Kuwahara A, Kondo S, Morizane C, Ueno H, et
al: Efficacy of sorafenib in patients with hepatocellular carcinoma
refractory to transcatheter arterial chemoembolization. J
Gastroenterol. 49:932–940. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, et al: Efficacy and safety of
sorafenib in patients in the Asia-Pacific region with advanced
hepatocellular carcinoma: A phase III randomised, double-blind,
placebo-controlled trial. Lancet Oncol. 10:25–34. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mise M, Arii S, Higashituji H, Furutani M,
Niwano M, Harada T, Ishigami S, Toda Y, Nakayama H, Fukumoto M, et
al: Clinical significance of vascular endothelial growth factor and
basic fibroblast growth factor gene expression in liver tumor.
Hepatology. 23:455–464. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Suzuki H, Mori M, Kawaguchi C, Adachi M,
Miura S and Ishii H: Serum vascular endothelial growth factor in
the course of transcatheter arterial embolization of hepatocellular
carcinoma. Int J Oncol. 14:1087–1090. 1999.PubMed/NCBI
|
|
15
|
Li X, Feng GS, Zheng CS, Zhuo CK and Liu
X: Expression of plasma vascular endothelial growth factor in
patients with hepatocellular carcinoma and effect of transcatheter
arterial chemoembolization therapy on plasma vascular endothelial
growth factor level. World J Gastroenterol. 10:2878–2882. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Poon RT, Lau C, Pang R, Ng KK, Yuen J and
Fan ST: High serum vascular endothelial growth factor levels
predict poor prognosis after radiofrequency ablation of
hepatocellular carcinoma: Importance of tumor biomarker in ablative
therapies. Ann Surg Oncol. 14:1835–1845. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sergio A, Cristofori C, Cardin R, Pivetta
G, Ragazzi R, Baldan A, Girardi L, Cillo U, Burra P, Giacomin A and
Farinati F: Transcatheter arterial chemoembolization (TACE) in
hepatocellular carcinoma (HCC): The role of angiogenesis and
invasiveness. Am J Gastroenterol. 103:914–921. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shim JH, Park JW, Kim JH, An M, Kong SY,
Nam BH, Choi JI, Kim HB, Lee WJ and Kim CM: Association between
increment of serum VEGF level and prognosis after transcatheter
arterial chemoembolization in hepatocellular carcinoma patients.
Cancer Sci. 99:2037–2044. 2008.PubMed/NCBI
|
|
19
|
Wilhelm SM, Adnane L, Newell P, Villanueva
A, Llovet JM and Lynch M: Preclinical overview of sorafenib, a
multikinase inhibitor that targets both Raf and VEGF and PDGF
receptor tyrosine kinase signaling. Mol Cancer Ther. 7:3129–3140.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kudo M, Imanaka K, Chida N, Nakachi K, Tak
WY, Takayama T, Yoon JH, Hori T, Kumada H, Hayashi N, et al: Phase
III study of sorafenib after transarterial chemoembolisation in
Japanese and Korean patients with unresectable hepatocellular
carcinoma. Eur J Cancer. 47:2117–2127. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sieghart W, Pinter M, Reisegger M, Müller
C, Ba-Ssalamah A, Lammer J and Peck-Radosavljevic M: Conventional
transarterial chemoembolisation in combination with sorafenib for
patients with hepatocellular carcinoma: A pilot study. Eur Radiol.
22:1214–1223. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pawlik TM, Reyes DK, Cosgrove D, Kamel IR,
Bhagat N and Geschwind JF: Phase II trial of sorafenib combined
with concurrent transarterial chemoembolization with drug-eluting
beads for hepatocellular carcinoma. J Clin Oncol. 29:3960–3967.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cabrera R, Pannu DS, Caridi J, Firpi RJ,
Soldevila-Pico C, Morelli G, Clark V, Suman A, George TJ Jr and
Nelson DR: The combination of sorafenib with transarterial
chemoembolisation for hepatocellular carcinoma. Aliment Pharmacol
Ther. 34:205–213. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|