Introduction
Hepatocellular carcinoma (HCC) is one of the most
common malignancies globally (1–3). Among
the various types of liver cancer, HCC is a major histological
subtype and accounts for about four-fifths of all primary liver
cancer cases (4). Recent advanced
imaging procedures have led to increased detection of early stage
HCC and improved survival, because curative therapies, such as
hepatic resection, liver transplantation, and radiofrequency
ablation, are possible in early stage patients (5). However, long-term survival remains
unsatisfactory, because of high recurrence rates, even after
curative therapy (6).
The development of advanced HCC with macroscopic
vascular invasion (MVI) especially hinders the use of additional
curative therapies, and therefore, this condition contributes to
poor survival. MVI, including the presence of a tumor thrombus in
the major portal vein, is known to be the most important negative
risk factor for survival after resection or liver transplantation
in patients with HCC (7,8). The median survival time of HCC patients
with MVI has been reported to be 2–3 months (9,10).
The landscape of systemic therapy for advanced HCC
has changed with the advent of molecular-targeted therapy.
Sorafenib, a relatively new molecular-targeted therapy for advanced
HCC, was approved in Japan in May 2009 (11–13).
Sorafenib is a multi-kinase inhibitor targeting the vascular
endothelial growth factor receptor, platelet-derived growth factor
receptor, and proto-oncoprotein c-Raf, among others (14,15). The
efficacy and safety of sorafenib in advanced HCC patients were
demonstrated in the Sorafenib HCC Assessment Randomized Protocol
(SHARP) (16), and Asia-Pacific
studies (17). However, sorafenib
monotherapy confers less than 3 months of actual survival benefit
in both Western and Asian populations (16,17).
Hepatic arterial infusion chemotherapy (HAIC) via an
implanted port system has been reported to be a useful therapeutic
option for advanced HCC, especially in patients with a major portal
vein tumor thrombus (PVTT), and response to HAIC is considered an
important prognostic factor (18–25).
Various chemotherapeutic regimens are used for HAIC, and the
combination of cisplatin and 5-fluorouracil (5-FU) is one of the
most common regimens. Repeated HAIC using low-dose 5-FU and
cisplatin (low-dose FP) has been shown to be useful in patients
with advanced HCC and tumor thrombus in the portal vein (18,19).
Additionally, Nagamatsu et al investigated the efficacy and
safety of the new combination therapy of cisplatin-lipiodol
suspension and 5-FU for HCC with portal vein tumor thrombus, which
was referred to as the new 5-FU and cisplatin therapy (NFP)
(25). The authors demonstrated that
the response rate was high at 86.3% and the median survival time
(MST) was 33 months using NFP for unresectable HCC with portal vein
tumor thrombus. While sorafenib and HAIC have been proven to
improve prognosis in HCC patients with MVI (26), which is the better option remains to
be determined.
The aim of the present multicenter, non-randomized,
prospective cohort study was to investigate the efficacy and safety
of NFP and compare the findings to those of sorafenib in patients
with advanced HCC and MVI, without extra-hepatic spread (EHS) and
Child-Pugh class A disease.
Patients and methods
Patients
The present study was performed between April 2008
and March 2014. A total of 64 HCC patients with MVI, without EHS
and Child-Pugh class A disease were registered. Of the 64 patients,
20 were treated with sorafenib and 44 were treated with NFP. Prior
to several treatments, all the patients in the sorafenib group were
treated without NFP and all the patients in the NFP group were
treated without sorafenib. The eligibility criteria for this study
were as follows: i) Eastern Cooperative Oncology Group (ECOG)
performance status of 0–2 (there were no patients with ECOG 2), ii)
measurable disease using the Response Evaluation Criteria in Solid
Tumors (RECIST) (27), iii)
Child-Pugh class A liver function, iv) leukocyte count of
≥2,000/mm3, v) platelet count of ≥50×109/l,
vi) hemoglobin level of ≥8.5 g/dl, vii) serum creatinine level of
<1.5 mg/dl, and viii) no ascites or encephalopathy. The enrolled
patients were treated with sorafenib at one of the following 14
experienced member institutions of the Kurume Liver Cancer Study
Group of Japan: Asakura Medical Association Hospital, Chikugo City
Hospital, Kurume General Hospital, Kurume University Medical
Center, Kurume University School of Medicine, Kyushu Medical
Center, Nagata Hospital, Ōmuta City Hospital, Saga Social Insurance
Hospital, Social Insurance Tagawa Hospital, St. Mary's Hospital,
Tobata Kyoritsu Hospital, Yame General Hospital, and Yokokura
Hospital. The primary outcome of this study was radiologic
progression-free survival, which was defined as the time from the
initiation of treatment to the date of disease progression. The
secondary outcome of this study was overall survival (OS), which
was defined as the time from the initiation of treatment to the
date of death or the patient's last follow-up. Relevant data from
all patient clinical records, including medical history, laboratory
results, radiological findings, histological results, and survival
data, were prospectively collected.
The study protocol was approved by the Ethics
Committee of Kurume University (no. 09227) and the University
Hospital Medical Information Network (UMIN) Center (no.
UMIN000004022), and conformed to the guidelines of the 1975
Declaration of Helsinki. Patients were provided comprehensive
information on the details of the clinical study, and each patient
provided written informed consent prior to participation.
Diagnosis
HCC was either confirmed histologically or diagnosed
using non-invasive criteria according to the European Association
for the Study of Liver (28).
Intrahepatic lesions and vascular invasion were diagnosed using a
combination of contrast-enhanced computed tomography (CT), magnetic
resonance imaging (MRI), ultrasonography (US), and digital
subtraction angiography. Additionally, α-fetoprotein (AFP), lens
culinaris agglutinin-reactive fraction of AFP (AFP-L3), and
des-γ-carboxy prothrombin (DCP) serum levels were measured up to 1
month before treatment. Hepatic functional reserve was evaluated
before treatment using the Child-Pugh scoring system. Tumor stage
was determined according to the Barcelona Clinic Liver Cancer
(BCLC) staging classification (29).
Sorafenib treatment
Performance status was used to determine the initial
sorafenib dose, at the discretion of the chief physician.
Discontinuation and dose reduction were allowed based on tolerance.
Side effects of sorafenib treatment were documented according to
the National Cancer Institute's Common Terminology Criteria for
Adverse Events (CTCAE), version 4.0. Treatments were discontinued
upon development of CTCAE grade 3 or higher adverse events with the
exception of a platelet count of <25×109/l and a
leukocyte count of <1,500/mm3.
Implantation of arterial catheter
An indwelling catheter (5-Fr W-spiral Catheter;
Piolax, Tokyo, Japan) was inserted through the femoral or brachial
artery, with the distal end of the catheter extended into the
hepatic artery or gastroduodenal artery, and the proximal end
connected to the port system (SOPH-A-PORT; Sophisa, Besançon,
France), which was implanted subcutaneously. The right gastric,
gastroduodenal, and posterior superior pancreaticoduodenal arteries
were occluded with VortX coils (Boston Scientific, Marlborough, MA,
USA) to prevent gastroduodenal ulcers caused by anticancer
agents.
Therapeutic NFP regimen
The NFP regimen comprised a combination of 50 mg
cisplatin in 5–10 ml lipiodol and a continuous infusion of 5-FU
(1,500 mg/5 days). On day 1 of treatment, cisplatin with lipiodol
was injected through the reservoir catheter followed by 5-FU (250
mg). Then, 5-FU (1,250 mg) was continuously infused using a balloon
pump (SUREFUSER PUMP, Nipro Pharma Corporation, Osaka, Japan) for 5
days. This regimen was administered once a week during the first 2
weeks of admission, and then, the combination of 20–35 mg cisplatin
with 2–5 ml lipiodol and 500–1,000 mg 5-FU was infused every 2
weeks at the out-patient department as long as possible. Treatment
was discontinued in case of the occurrence of grade 3 or higher
adverse effects according to the ECOG classification (30), with the exception of total bilirubin
>3.0 mg/dl, platelet count <25×109/l, and
leukocyte count <1,500/mm3.
Assessment of tumor response
To determine the therapeutic effect, baseline tumor
measurements were obtained within 1 month before treatment by
combining the largest diameters of selected target lesions in each
patient as measured using CT or MRI. CT or MRI was performed 4–6
weeks after the initial treatment cycle and every 2–3 months
thereafter. The therapeutic effect was determined according to the
best overall response, which was defined by the RECIST as follows:
Complete response (CR), disappearance of all measurable lesions for
>4 weeks; partial response (PR), >30% decrease in the sum of
the largest target-lesion diameters and no development of a new
lesion for >4 weeks; progressive disease (PD), >25% increase
in the sum of the largest target-lesion diameters or appearance of
a new lesion; and stable disease (SD), neither PR nor PD seen for
>8 weeks (31). Patients who died
before their first radiographic assessment were classified as
having PD. Data from patients who died without tumor progression
were censored. The response rate was defined, on the basis of
independent radiologic review, as the percentage of patients whose
best-response RECIST rating of CR or PR was maintained for at least
1 month after the first demonstration of such a rating. The
disease-control rate was defined, on the basis of independent
radiologic review, as the percentage of patients whose
best-response RECIST rating of CR, PR, or SD was maintained for at
least 1 month after the first demonstration of such a rating.
Statistical analysis
Baseline patient characteristics were analyzed using
descriptive statistical methods. Survival curves were calculated
using the Kaplan-Meier method. Univariate analysis of survival
curves was performed using the log-rank test. P<0.05 was
considered statistically significant. The Cox proportional-hazards
model was used to evaluate the interaction between baseline
characteristics and overall survival or therapeutic effect. The JMP
software (SAS Institute, Inc., Cary, NC, USA), version 12, was used
for all analyses.
Results
Patient characteristics
The sorafenib therapy group (n=20) included 17 (85%)
men and 3 (15%) women, with a mean age of 65.4 years (Table I). Chronic hepatitis C virus
infection was the predominant cause of HCC (n=8; 40%), followed by
chronic hepatitis B virus infection (n=5; 25%). Of the 20 patients,
10 (50%) had a Child-Pugh score of 5 and 10 (50%) had a Child-Pugh
score of 6. Prior to sorafenib therapy, 12 (60%) patients received
previous treatment. HCC showed portal vein invasion, with 5 (25%)
patients having main trunk invasion and 15 (75%) having first or
second branch invasion, and the mean size was 74.3 mm.
 | Table I.Patient characteristics (n=64). |
Table I.
Patient characteristics (n=64).
| Variables | Sorafenib
(n=20) | NFP (n=44) | P-value |
|---|
| Age (years) | 65.4±8.1 | 63.4±10.0 | 0.426 |
| Sex, n (%) |
|
| 0.519 |
|
Male | 17 (85) | 33 (75) |
|
|
Female | 3 (15) | 11 (25) |
|
| HBs antigen, n
(%) |
|
| 0.238 |
|
Present | 5 (25) | 6 (14) |
|
|
Absent | 15 (75) | 38 (86) |
|
| HCV antibody, n
(%) |
|
| 0.054 |
|
Present | 8 (40) | 29 (66) |
|
|
Absent | 12 (60) | 15 (34) |
|
| Child-Pugh score, n
(%) |
|
| 0.787 |
| 5 | 10 (50) | 19 (43) |
|
| 6 | 10 (50) | 25 (57) |
|
| AFP (ng/ml), n
(%) |
|
| 0.787 |
|
<1,000 | 5 (25) | 22 (50) |
|
|
≥1,000 | 15 (75) | 22 (50) |
|
| DCP (AU/ml), n
(%) |
|
| 0.791 |
|
<1,000 | 12 (60) | 24 (55) |
|
|
≥1,000 | 8 (40) | 20 (45) |
|
| Previous treatment,
n (%) |
|
| 0.787 |
|
Present | 12 (60) | 28 (64) |
|
|
Absent | 8 (40) | 16 (36) |
|
| Maximum
tumor size, mm | 74.3±54.2 | 74.2±33.3 | 0.995 |
| Grade of portal
vein invasion, n (%) |
|
| 0.124 |
|
Trunk | 5 (25) | 4 (9) |
|
|
Branch | 15 (75) | 40 (91) |
|
| Hepatic vein
invasion, n (%) |
|
| 0.486 |
|
Present | 2 (10) | 8 (18) |
|
|
Absent | 18 (90) | 36 (82) |
|
On the other hand, the NFP group (n=44) included 33
(75%) men and 11 (25%) women, with a mean age of 63.4 years
(Table I). Chronic hepatitis C virus
infection was the predominant cause of HCC (n=29; 66%), followed by
chronic hepatitis B virus infection (n=5; 14%). Of the 44 patients,
19 (43%) had a Child-Pugh score of 5 and 25 (57%) had a Child-Pugh
score of 6. Prior to NFP, 28 (64%) patients received previous
treatment. HCC showed portal vein invasion, with 4 (9%) having main
trunk invasion and 40 (91%) having first or second branch invasion,
and the mean size was 74.2 mm.
There were no statistically significant differences
in the clinical factors between the groups.
Overall response and efficacy
Table II shows the
results at the first radiologic assessment according to the RECIST.
Of the 20 patients treated with sorafenib, 0 (0%), 2 (10%), and 8
(40%) patients had CR, PR, and SD, respectively. The response rate
was 10%, and the disease-control rate was 50%.
 | Table II.Therapeutic effects in all patients
(n=64). |
Table II.
Therapeutic effects in all patients
(n=64).
| Therapeutic
effect | Sorafenib
(n=20) | NFP (n=44) |
|---|
| CR | 0 (0) | 10 (23) |
| PR | 2 (10) | 21 (48) |
| SD | 8 (40) | 8 (18) |
| PD | 10 (50) | 5 (11) |
On the other hand, of the 44 patients treated with
NFP, 10 (23%), 21 (48%), and 8 (18%) patients had CR, PR, and SD,
respectively. The response rate was 71%, and the disease-control
rate was 89%.
Factors associated with survival
outcomes
Cox proportional-hazards regression analysis was
performed to identify the independent factors associated with
survival (Table III). Univariate
analysis of survival identified 4 baseline patient characteristics
as prognostic indicators for OS, including Child-Pugh score, grade
of portal vein invasion, regimen, and therapeutic effect.
Multivariate analysis confirmed that Child-Pugh score [5; P=0.022,
95% confidence interval (CI)=0.191–0.892], grade of portal vein
invasion (branch; P=0.002, 95% CI=0.118–0.614), and therapeutic
effect (CR/PR; P=0.009, 95% CI=0.220–0.752) were independent
factors for survival.
 | Table III.Univariate and multivariate analyses
of overall survival. |
Table III.
Univariate and multivariate analyses
of overall survival.
|
|
| Multivariate
analysis |
|---|
|
|
|
|
|---|
| Variable | Univariate analysis
P-value | 95% CI | P-value |
|---|
| Age (≥65
years) | 0.456 |
|
|
| Sex (male) | 0.242 |
|
|
| HBs Ag (+) | 0.631 |
|
|
| HCV Ab (+) | 0.661 |
|
|
| Child-Pugh score
(5) | 0.004 | 0.191–0.892 | 0.022 |
| AFP (≥1,000
ng/ml) | 0.169 |
|
|
| DCP (≥1,000
mAU/ml) | 0.452 |
|
|
| Previous treatment
(present) | 0.457 |
|
|
| Maximum tumor size
(≥100 mm) | 0.267 |
|
|
| Grade of portal
vein invasion (Branch) | <0.001 | 0.118–0.614 | 0.002 |
| Hepatic vein
invasion (present) | 0.176 |
|
|
| Regimen (NFP) | 0.015 |
|
|
| Therapeutic effect
(CR or PR) | <0.001 | 0.220–0·752 | 0.009 |
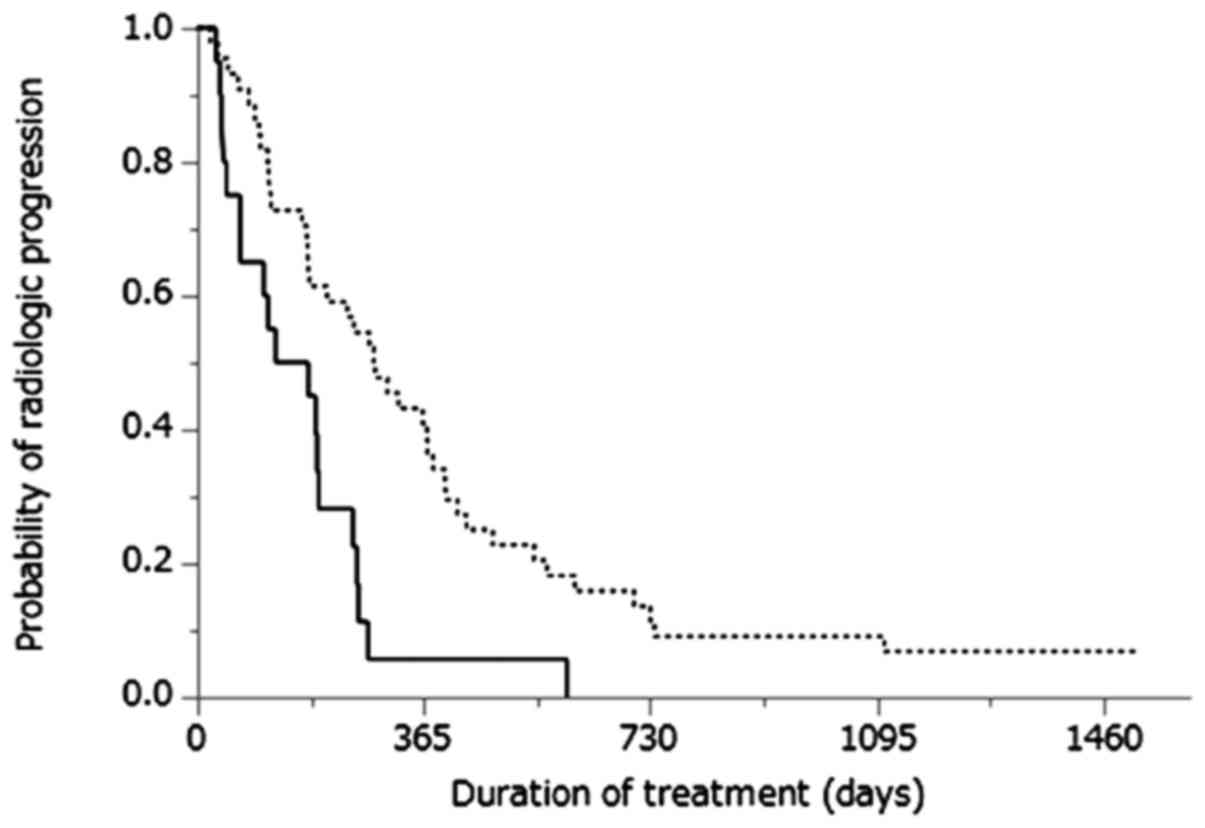
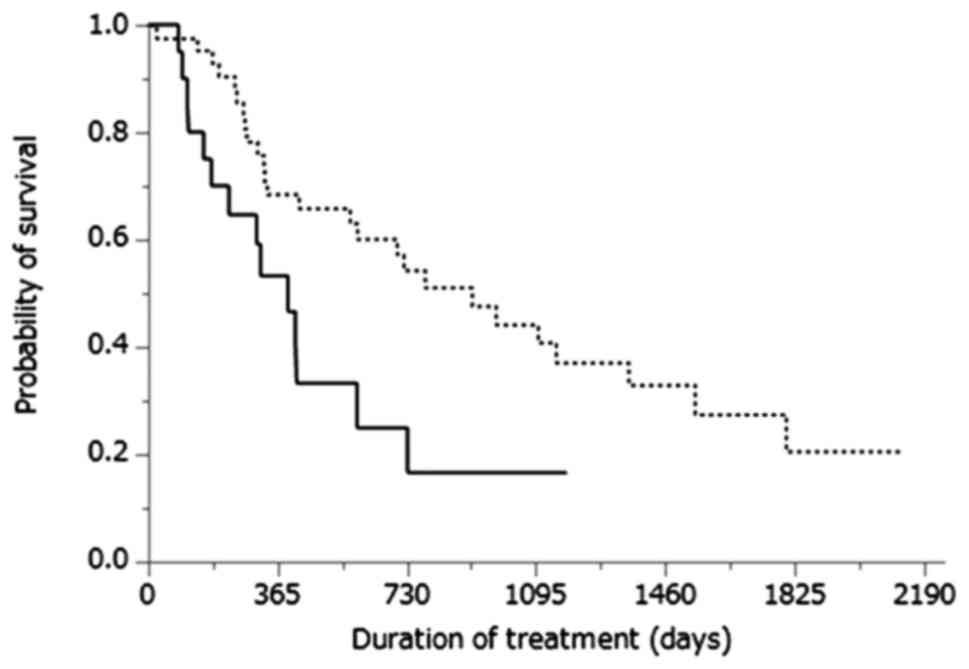
Cumulative progression-free survival curves of
patients treated with either sorafenib therapy or NFP are shown in
Fig. 1. The MST was 5.1 months for
patients treated with sorafenib therapy and 9.5 months for those
treated with NFP (P=0.002). Cumulative OS curves of patients
treated with sorafenib therapy or NFP are shown in Fig. 2. The MST was 13.2 months for patients
treated with sorafenib therapy and 30.4 months for those treated
with NFP (P=0.013).
Comparison of patient characteristics
based on therapeutic effect
Cox proportional-hazards regression analysis was
performed to identify the independent factors associated with
therapeutic effect (Table IV).
Univariate analysis of the therapeutic effect identified three
baseline patient characteristics as prognostic indicators for
therapeutic response, including DCP level at baseline, maximum
tumor size, and regimen. Multivariate analysis confirmed that
maximum tumor size (≥100 mm, P=0.007, 95% CI=1.960–75.10) and
regimen (NFP, P<0.001, 95% CI=0.006–0.199) were independent
factors for therapeutic response.
 | Table IV.Univariate and multivariate analyses
of the comparison of patient characteristics based on therapeutic
effect. |
Table IV.
Univariate and multivariate analyses
of the comparison of patient characteristics based on therapeutic
effect.
|
|
|
|
| Multivariate
analysis |
|---|
|
|
|
|
|
|
|---|
| Variables | CR + PR (n=31) | SD + PD (n=33) | Univariate analysis
P-value | 95% CI | P-value |
|---|
| Age (≥65
years) | 68.3±9.5 | 68.6±8.6 | 0.892 |
|
|
| Sex (male) | 25/6 | 25/8 | 0.763 |
|
|
| Child-Pugh score
(5) | 13/18 | 22/11 | 0.078 |
|
|
| AFP (≥1,000
ng/ml) | 19/12 | 18/15 | 0.248 |
|
|
| DCP (≥1,000
mAU/ml) | 9/22 | 14/19 | 0.042 |
|
|
| Previous treatment
(present) | 21/10 | 23/10 | 0.140 |
|
|
| Maximum tumor size
(≥100 mm) | 19/12 | 31/2 | 0.045 | 1.961–75.12 | 0.007 |
| Grade of portal
vein invasion (Branch) | 5/26 | 4/29 | 0.729 |
|
|
| Hepatic vein
invasion (present) | 6/25 | 4/29 | 0.326 |
|
|
| Regimen (NFP) | 18/13 | 2/31 | <0.001 | 0.006–0.199 | <0.001 |
Adverse events
Severe adverse events were observed in 5 patients.
In the sorafenib group, 2 patients had hepatic failure, while in
the NFP group, 2 patients had hepatic failure and 1 had a
pseudo-aneurysm. In the two groups, treatment-related mortality was
not observed.
Discussion
Sorafenib, an oral multi-kinase inhibitor and a new
molecular-targeted therapy for advanced HCC has been shown to offer
a significant survival benefit with good tolerance in two
randomized phase III placebo-controlled trials (16,17).
Thus, it has become the standard treatment for advanced HCC. In the
SHARP trial, the median overall survival times of all patients and
patients with MVI treated with sorafenib were 10.7 and 8.1 months,
respectively (16). However,
contrary to our expectations, the survival and therapeutic
advantages of sorafenib are modest.
PVTT is a common complication in HCC, and it has
been reported in 65% of cases at autopsy (32). PVTT often leads to extensive
spreading of the tumor and can increase portal venous blood
pressure, resulting in the fatal rupture of esophageal varices
(33). PVTT can also decrease portal
flow that may lead to ascites, jaundice, hepatic encephalopathy, or
liver failure (33). Therefore, the
presence of PVTT is one of the most significant prognostic factors
of poor outcome (34,35), and it has been reported that these
patients survive only 2.7–4 months if left untreated (35,36). In
advanced HCC patients with PVTT, standard treatments have not been
established. The prognosis for advanced HCC with PVTT is dismal
owing to poor response to current treatment modalities (37). Although the BCLC staging system
recommends sorafenib in these patients, its efficacy is limited. In
another study, the MST of patients with PVTT was only 5 months
(38). Thus, HAIC is considered an
alternative treatment modality (38).
The difference between NFP and conventional TACE is
the administration of a drug repeatedly from the reservoir system
without using embolic material. As embolic material is not used, it
becomes possible to enhance the therapeutic effect by repeating the
treatment. The difference between NFP and conventional HAI is the
use of lipiodol. By using lipiodol, it is possible to temporarily
enhance the antitumor effect through the vascular embolic
effect.
The response rate and disease-control rate were 10
and 50% in the sorafenib therapy group, and 71 and 89% in the NFP
group, respectively (Table II). We
demonstrated that the therapeutic response rate of NFP was superior
to that of sorafenib. The rationale of the cisplatin + 5-FU regimen
is that cisplatin and 5-FU have antitumor effects (39), and cisplatin has a synergistic effect
as a modulator of 5-FU (40). In the
present study, 5-FU was continuously infused for 5 days. 5-FU does
not show a dose-dependent effect, but shows a time-dependent
antitumor effect (41). Continuous
infusion of 5-FU may enhance the antitumor effect in
cisplatin-lipiodol plus 5-FU therapy compared with other HAIC
regimens. The antitumor effect has been reported to be more potent
with anticancer agents in lipiodol suspension than with anticancer
agents alone, such as sorafenib (42).
Multivariate analysis identified three baseline
patient characteristics as prognostic indicators for overall
survival, including the Child-Pugh score, grade of portal vein
invasion, and therapeutic effect (Table III). We demonstrated that the
therapeutic response was a significant risk factor adversely
affecting survival in this study. Consistent with a previous study
showing that early radiological progression after treatment
predicts poor survival, our patients, who developed early PD, had
significantly worse OS (43).
Another multivariate analysis identified two baseline patient
characteristics as prognostic indicators for therapeutic effect,
including maximum tumor size and regimen (Table IV). In our study, patients treated
with NFP survived longer than patients treated with sorafenib
monotherapy. We demonstrated that the therapeutic response was more
effective in patients treated with NFP than in patients treated
with sorafenib. HAIC is a reasonable drug delivery system for
patients with advanced HCC because advanced HCC receives most of
its blood supply from the hepatic artery, and the non-cancerous
liver is supplied mainly by the portal vein (44). HAIC appears to deliver high
concentrations of chemotherapeutic agents to HCC tissues
selectively, with low toxicity for non-cancerous liver tissues and
the whole body. Several reports described the effects of HAIC with
cisplatin and 5-FU or systemic interferon-α therapy with HAIC using
5-FU for HCC patients with tumor thrombosis in the first branches
and the portal vein trunks (21,45).
Therefore, we showed that NFP is more effective than sorafenib
therapy in patients with advanced HCC and MVI.
The present study has limitations. First, there was
no protocol to guide treatment selection. Therefore, the treatments
were selected at the discretion of the chief physician and were not
randomized. This resulted in a selection bias for patients treated
with sorafenib therapy and NFP, although there were no significant
differences in the patient characteristics between the two groups.
Second, some patients received multiple treatments other than
sorafenib therapy or NFP. Third, the modified RECIST criteria
should have also been used for the evaluation of tumor response and
disease control rate. However, the therapeutic effect was
determined according to only the RECIST criteria at the different
centers in the sorafenib group. Therefore, we were unable to use
the modified RECIST for the evaluation of tumor response and the
disease control rate. Lastly, the size of the study cohort was
relatively small. To confirm the superiority of NFP over sorafenib
in patients with advanced HCC and MVI, prospective randomized
studies with a larger number of subjects are required.
In conclusion, our results showed that NFP was a
significantly positive prognostic treatment for patients with
advanced HCC and MVI. The survival potential was greater in
patients treated with NFP than in those treated with sorafenib.
Therefore, NFP should be the first choice for patients with
advanced HCC and MVI, without EHS and Child-Pugh A disease.
Acknowledgements
The authors thank the staff of the Kurume Liver
Cancer Study Group of Japan for their valuable support. The authors
also thank Editage (www.editage.jp) for English language editing.
References
|
1
|
El-Serag HB and Mason AC: Rising incidence
of hepatocellular carcinoma in the United States. N Engl J Med.
340:745–750. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sherman M: Hepatocellular carcinoma:
Epidemiology, risk factors, and screening. Semin Liver Dis.
25:143–154. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Perz JF, Armstrong GL, Farrington LA,
Hutin YJ and Bell BP: The contributions of hepatitis B virus and
hepatitis C virus infections to cirrhosis and primary liver cancer
worldwide. J Hepatol. 45:529–538. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Takayama T, Makuuchi M, Hirohashi S,
Sakamoto M, Yamamoto J, Shimada K, Kosuge T, Okada S, Takayasu K
and Yamasaki S: Early hepatocellular carcinoma as an entity with a
high rate of surgical cure. Hepatology. 28:1241–1246. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nagasue N, Uchida M, Makino Y, Takemoto Y,
Yamanoi A, Hayashi T, Chang YC, Kohno H, Nakamura T and Yukaya H:
Incidence and factors associated with intrahepatic recurrence
following resection of hepatocellular carcinoma. Gastroenterology.
105:488–494. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liver Cancer Study Group of Japan: Primary
liver cancer in Japan. Clinicopathologic features and results of
surgical treatment. Ann Surg. 211:277–287. 1990.PubMed/NCBI
|
|
8
|
Jonas S, Bechstein WO, Steinmüller T,
Herrmann M, Radke C, Berg T, Settmacher U and Neuhaus P: Vascular
invasion and histopathologic grading determine outcome after liver
transplantation for hepatocellular carcinoma in cirrhosis.
Hepatology. 33:1080–1086. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pawarode A, Voravud N, Sriuranpong V,
Kullavanijaya P and Patt YZ: Natural history of untreated primary
hepatocellular carcinoma: A retrospective study of 157 patients. Am
J Clin Oncol. 21:386–391. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Llovet JM, Bustamante J, Castells A,
Vilana R, Ayuso Mdel C, Sala M, Brú C, Rodés J and Bruix J: Natural
history of untreated nonsurgical hepatocellular carcinoma:
Rationale for the design and evaluation of therapeutic trials.
Hepatology. 29:62–67. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Furuse J, Ishii H, Nakachi K, Suzuki E,
Shimizu S and Nakajima K: Phase I study of sorafenib in Japanese
patients with hepatocellular carcinoma. Cancer Sci. 99:159–165.
2008.PubMed/NCBI
|
|
12
|
Nakano M, Tanaka M, Kuromatsu R, Nagamatsu
H, Sakata K, Matsugaki S, Kajiwara M, Fukuizumi K, Tajiri N,
Matsukuma N, et al: Efficacy, safety, and survival factors for
sorafenib treatment in Japanese patients with advanced
hepatocellular carcinoma. Oncology. 84:108–114. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nakano M, Tanaka M, Kuromatsu R, Nagamatsu
H, Tajiri N, Satani M, Niizeki T, Aino H, Okamura S, Iwamoto H, et
al: Sorafenib for the treatment of advanced hepatocellular
carcinoma with extrahepatic metastasis: A prospective multicenter
cohort study. Cancer Med. 4:1836–1843. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wilhelm SM, Adnane L, Newell P, Villanueva
A, Llovet JM and Lynch M: Preclinical overview of sorafenib, a
multikinase inhibitor that targets both Raf and VEGF and PDGF
receptor tyrosine kinase signaling. Mol Cancer Ther. 7:3129–3140.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wilhelm SM, Carter C, Tang L, Wilkie D,
McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, et al:
BAY 43–9006 exhibits broad spectrum oral antitumor activity and
targets the RAF/MEK/ERK pathway and receptor tyrosine kinases
involved in tumor progression and angiogenesis. Cancer Res.
64:7099–7109. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, et al: Efficacy and safety of
sorafenib in patients in the Asia-Pacific region with advanced
hepatocellular carcinoma: A phase III randomised, double-blind,
placebo-controlled trial. Lancet Oncol. 10:25–34. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ando E, Yamashita F, Tanaka M and Tanikawa
K: A novel chemotherapy for advanced hepatocellular carcinoma with
tumor thrombosis of the main trunk of the portal vein. Cancer.
79:1890–1896. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ando E, Tanaka M, Yamashita F, Kuromatsu
R, Yutani S, Fukumori K, Sumie S, Yano Y, Okuda K and Sata M:
Hepatic arterial infusion chemotherapy for advanced hepatocellular
carcinoma with portal vein tumor thrombosis: Analysis of 48 cases.
Cancer. 95:588–595. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chung YH, Song IH, Song BC, Lee GC, Koh
MS, Yoon HK, Lee YS, Sung KB and Suh DJ: Combined therapy
consisting of intraarterial cisplatin infusion and systemic
interferon-alpha for hepatocellular carcinoma patients with major
portal vein thrombosis or distant metastasis. Cancer. 88:1986–1991.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Obi S, Yoshida H, Toune R, Unuma T, Kanda
M, Sato S, Tateishi R, Teratani T, Shiina S and Omata M:
Combination therapy of intraarterial 5-fluorouracil and systemic
interferon-alpha for advanced hepatocellular carcinoma with portal
venous invasion. Cancer. 106:1990–1997. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Park JY, Ahn SH, Yoon YJ, Kim JK, Lee HW,
Lee DY, Chon CY, Moon YM and Han KH: Repetitive short-course
hepatic arterial infusion chemotherapy with high-dose
5-fluorouracil and cisplatin in patients with advanced
hepatocellular carcinoma. Cancer. 110:129–137. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yamasaki T, Kimura T, Kurokawa F, Aoyama
K, Ishikawa T, Tajima K, Yokoyama Y, Takami T, Omori K, Kawaguchi
K, et al: Prognostic factors in patients with advanced
hepatocellular carcinoma receiving hepatic arterial infusion
chemotherapy. J Gastroenterol. 40:70–78. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Niizeki T, Sumie S, Torimura T, Kurogi J,
Kuromatsu R, Iwamoto H, Aino H, Nakano M, Kawaguchi A, Kakuma T and
Sata M: Serum vascular endothelial growth factor as a predictor of
response and survival in patients with advanced hepatocellular
carcinoma undergoing hepatic arterial infusion chemotherapy. J
Gastroenterol. 47:686–695. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nagamatsu H, Hiraki M, Mizukami N, Yoshida
H, Iwamoto H, Sumie S, Torimura T and Sata M: Intra-arterial
therapy with cisplatin suspension in lipiodol and 5-fluorouracil
for hepatocellular carcinoma with portal vein tumour thrombosis.
Aliment Pharmacol Ther. 32:543–550. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bruix J, Raoul JL, Sherman M, Mazzaferro
V, Bolondi L, Craxi A, Galle PR, Santoro A, Beaugrand M,
Sangiovanni A, et al: Efficacy and safety of sorafenib in patients
with advanced hepatocellular carcinoma: Subanalyses of a phase III
trial. J Hepatol. 57:821–829. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bruix J, Sherman M, Llovet JM, Beaugrand
M, Lencioni R, Burroughs AK, Christensen E, Pagliaro L, Colombo M
and Rodés J: EASL Panel of Experts on HCC: Clinical management of
hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL
conference. European Association for the Study of the Liver. J
Hepatol. 35:421–430. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Forner A, Reig ME, de Lope CR and Bruix J:
Current strategy for staging and treatment: The BCLC update and
future prospects. Semin Liver Dis. 30:61–74. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Therasse P, Arbuck SG, Eisenhauer EA,
Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van
Oosterom AT, Christian MC and Gwyther SG: New guidelines to
evaluate the response to treatment in solid tumors. European
Organization for Research and Treatment of Cancer, National Cancer
Institute of the United States, National Cancer Institute of
Canada. J Natl Cancer Inst. 92:205–216. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nakashima T, Okuda K, Kojiro M, Jimi A,
Yamaguchi R, Sakamoto K and Ikari T: Pathology of hepatocellular
carcinoma in Japan. 232 Consecutive cases autopsied in ten years.
Cancer. 51:863–877. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Song DS, Bae SH, Song MJ, Lee SW, Kim HY,
Lee YJ, Oh JS, Chun HJ, Lee HG, Choi JY and Yoon SK: Hepatic
arterial infusion chemotherapy in hepatocellular carcinoma with
portal vein tumor thrombosis. World J Gastroenterol. 19:4679–4688.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Park KW, Park JW, Choi JI, Kim TH, Kim SH,
Park HS, Lee WJ, Park SJ, Hong EK and Kim CM: Survival analysis of
904 patients with hepatocellular carcinoma in a hepatitis B
virus-endemic area. J Gastroenterol Hepatol. 23:467–473. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Okuda K, Ohtsuki T, Obata H, Tomimatsu M,
Okazaki N, Hasegawa H, Nakajima Y and Ohnishi K: Natural history of
hepatocellular carcinoma and prognosis in relation to treatment.
Study of 850 patients. Cancer. 56:918–928. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Villa E, Moles A, Ferretti I, Buttafoco P,
Grottola A, Del Buono M, De Santis M and Manenti F: Natural history
of inoperable hepatocellular carcinoma: Estrogen receptors' status
in the tumor is the strongest prognostic factor for survival.
Hepatology. 32:233–238. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lin CC, Hung CF, Chen WT and Lin SM:
Hepatic arterial infusion chemotherapy for advanced hepatocellular
carcinoma with portal vein thrombosis: Impact of early response to
4 weeks of treatment. Liver Cancer. 4:228–240. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Nakano M, Tanaka M, Kuromatsu R, Nagamatsu
H, Satani M, Niizeki T, Okamura S, Iwamoto H, Shimose S, Shirono T,
et al: Alternative treatments in advanced hepatocellular carcinoma
patients with progressive disease after sorafenib treatment: A
prospective multicenter cohort study. Oncotarget. 7:64400–64409.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Paquet KJ, Kalk JF, Cuan-Orozco F, Siemens
F, Koussouris P and Mercado MA: Hepatic chemoinfusion of 5-FU in
metastasis of gastrointestinal cancer and advanced primary
hepatocellular carcinoma. Eur J Surg Oncol. 18:156–161.
1992.PubMed/NCBI
|
|
40
|
Hata F, Sasaki K, Hirata K, Yamamitsu S
and Shirasaka T: Efficacy of a continuous venous infusion of
fluorouracil and daily divided dose cisplatin as adjuvant therapy
in resectable colorectal cancer: A prospective randomized trial.
Surg Today. 38:623–632. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Okabe H, Toko T, Saito H, Nakano K,
Fujioka A, Yuasa C, Takeda S and Unemi N: Augmentation of the
chemotherapeutic effectiveness of UFT, a combination of tegafur
[1-(2-tetrahydrofuryl)-5-fluorouracil] with uracil, by oral
l-leucovorin. Anticancer Res. 17:157–164. 1997.PubMed/NCBI
|
|
42
|
Terayama N, Matsui O, Gabata T, Kobayashi
S, Sanada J, Ueda K, Kadoya M and Kawamori Y: Accumulation of
iodized oil within the nonneoplastic liver adjacent to
hepatocellular carcinoma via the drainage routes of the tumor after
transcatheter arterial embolization. Cardiovasc Intervent Radiol.
24:383–387. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Iavarone M, Cabibbo G, Piscaglia F,
Zavaglia C, Grieco A, Villa E, Cammà C and Colombo M: SOFIA
(SOraFenib Italian Assessment) study group: Field-practice study of
sorafenib therapy for hepatocellular carcinoma: A prospective
multicenter study in Italy. Hepatology. 54:2055–2063. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Breedis C and Young G: The blood supply of
neoplasms in the liver. Am J Pathol. 30:969–977. 1954.PubMed/NCBI
|
|
45
|
Itamoto T, Nakahara H, Tashiro H, Haruta
N, Asahara T, Naito A and Ito K: Hepatic arterial infusion of
5-fluorouracil and cisplatin for unresectable or recurrent
hepatocellular carcinoma with tumor thrombus of the portal vein. J
Surg Oncol. 80:143–148. 2002. View Article : Google Scholar : PubMed/NCBI
|