Introduction
Although the incidence of osteoradionecrosis (ORN)
of the jaw seems to be progressively declining in recent years
(1), it remains one of the most
serious complications of radiation therapy (RT) for head and neck
malignancy. Patients with advanced ORN have nutrient insufficiency,
pain, and chronic drainage, resulting in severely decreased quality
of life (2).
Jacobson et al (3) classify ORN into stages I–III. Stage I
(early stage) exhibits minimal soft tissue ulceration and limited
exposure of cortical bone. It should be treated conservatively.
Stage I ORN rarely progresses to stage II [3]. Stage II
(intermediate stage) exhibits pathologic changes localized in the
mandibular cortex and underlying medullary bone. Most stage II ORN
resolves with conservative treatment or minimal surgical
intervention (3). Stage III
(advanced stage) shows full-thickness involvement of the bone,
including the inferior border (e.g., pathologic fracture may be
present). Surgical intervention (i.e., bone and/or soft tissue
replacement) is the definitive treatment for stage III (3).
Early detection and intervention are essential to
prevent progression to advanced ORN. A previous study showed that
panoramic radiography was useful for monitoring ORN, despite
underestimating ORN on these images (4). In fact, patients whose pathologic
changes are shown on panoramic radiographs sometimes develop
intermediate or advanced ORN.
A recent study demonstrated that fluorodeoxyglucose
positron emission tomography with computed tomography (FDG-PET CT)
detects local and diffuse metabolic changes that may not be
revealed on plain radiography in patients with medication-related
osteonecrosis of the jaw (MRONJ) (5). Another previous study showed that
FDG-PET reflects the disease course and indicates the point of
clinical remission in patients with mandibular chronic
osteomyelitis (6). The role of
FDG-PET in infectious diseases has been attracting attention, and
its usefulness in the diagnosis of active osteomyelitis in various
regions of the body (e.g., legs, lumbar spine) has recently been
reported (7,8).
In the present study, we focus on post-treatment
follow-up PET CT imaging (i.e., PET CT for monitoring and ruling
out recurrence and metastasis of head and neck cancer) to detect
and understand the pathologic state of ORN. The main objective of
our retrospective case series study was to evaluate the FDG
accumulation on post-treatment follow-up PET CT imaging in patients
who developed mandibular ORN. The authors hypothesized that the FDG
uptake would be detected on PET images before the clinicians found
and diagnosed mandibular ORN.
Patients and methods
Study population
All patients with head and neck malignancies
included in this study were mainly treated by otolaryngologists,
radiation oncologists, and medical oncologists in our hospital.
Oral and maxillofacial surgeons performed pre-RT dental
examinations and prophylactic extraction of unrestorable teeth
before initiating RT. After completion of the treatment for head
and neck malignancies (RT with chemotherapy or surgery), attending
clinicians in each department performed routine follow-up. During
this post-treatment observation period, imaging examinations were
applied as necessary to rule out local recurrence and metastasis.
The timing, frequency, and type of imaging examinations were
decided by the attending otolaryngologist, radiation oncologist,
and medical oncologist. Patients suspected of having ORN by
attending clinicians were re-introduced to our department. In this
study, these second introductions to us from other departments for
the diagnosis and treatment of ORN were designated ‘second visit’
cases.
To elucidate the usefulness of FDG-PET CT for
diagnosing mandibular ORN, we excluded patients who had not
undergone FDG-PET CT several times during the post-treatment
observation period. Patients with maxillary ORN were also excluded.
Only cancer patients who achieved a complete response to treatment
were included. Patients with recurrent cancer after treatment were
excluded. In all, 14 patients who re-visited our department for the
treatment of mandibular ORN from October 2011 to April 2016 were
included in the study. Because of the retrospective nature of this
study, the institutional review board in our hospital granted an
exemption (in writing) from requiring written informed consent from
the patients in the study.
ORN was defined as exposure of the bone for >6
months (9). The following
epidemiologic data were retrospectively gathered from the medical
charts: Age, sex, histologic diagnosis and site of the primary
tumor, radiation dose, chemotherapy, surgery for head and neck
cancer, interval between completion of RT and the second visit to
our department for the treatment of ORN, frequency of FDG-PET CT
during observation follow-up periods, and type of treatment of
mandibular ORN. The latter was divided into conservative and
surgical interventions. The former included repeated local wound
irrigation, antibiotic administration, and hyperbaric oxygen
therapy (HBO). The latter included surgical debridement with or
without free tissue transfer.
FDG-PET CT evaluation
Evaluation of FDG uptake by PET CT during the
observation follow-up periods was performed by three observers
(J.K., S.W., M.K.). Observer 1 (J.K.) is a specialist in oral and
maxillofacial surgery with more than 10 years of experience, and
observers 2 and 3 (S.W. and M.K.) are graduate fellows in the
Department of Oral and Maxillofacial Surgery. A
Microsoft® Office PowerPoint presentation (PPT) had been
prepared by the first author (M.A.). The areas exhibiting FDG
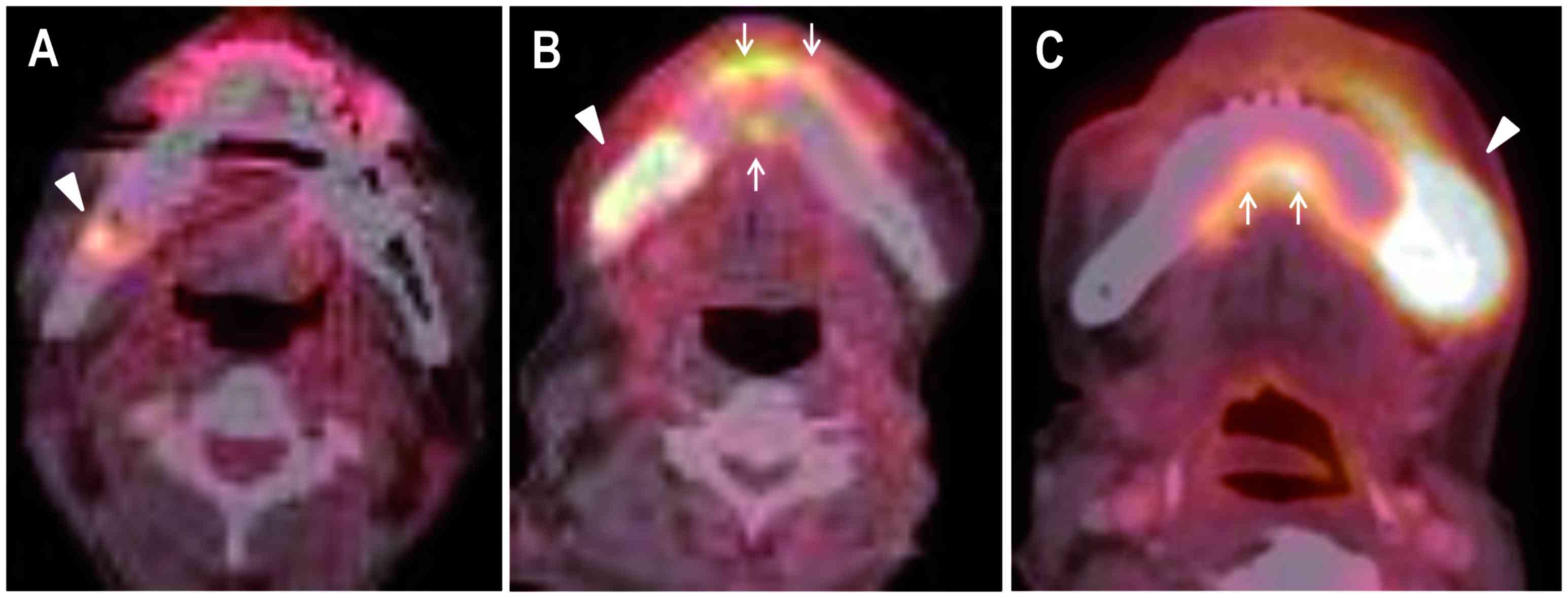
uptake were classified into three types: (1) spot type, with only spot accumulation of
FDG that did not extend to the labial or lingual sides of
mandibular cortices (Fig. 1A);
(2) localized type, with
accumulation of FDG restricted to within the bone resorption area
in the mandible (Fig. 1B); (3) extensive type, in which the FDG
accumulation extended from the mandible into the surrounding soft
tissue (Fig. 1C). Slight uptake of
FDG along the mandible outward was regarded as ‘non-specific’
(Fig. 1). To differentiate between
‘specific’ and ‘non-specific’ accumulation of FDG, the features of
‘specific’ accumulation were defined as follows: The shape of the
FDG accumulation was circular or elliptical, with its center
located in the mandible (Fig. 1). In
patients with bilateral ORN, the lesions accompanied by clinical
symptoms were evaluated. Three observers reviewed the PPT
individually. After one week, order of the PPT slides was randomly
changed, and assessed again by the same observers to allow to
evaluate intra-observer reliability. The results of the second
reviews were edited according to the first reviews to enable
comparison between the first and second observation. Discrepant
results were solved with reassessment by a first author and three
observers.
Both the mean and maximum standard uptake value
(SUVmean and SUVmax) were analyzed
quantitatively in the axial planes by using DICOM workstation
(Yokogawa Medical Solutions Corporation, Tokyo, Japan).
Statistical analysis
Fisher's exact test was used to compare associations
between the type of FDG accumulation and the type of treatment
(conservative or surgical intervention). Kruskal-Wallis test with
Steel-Dwass multiple comparisons was used to compare the values of
SUV among three types of FDG accumulation (i.e., spot, localized,
and extensive type). Intra-observer reliability was evaluated by
calculating Cohen's Kappa, and inter-observer reliability was
assessed with Fleiss' Kappa. Statistical significance was accepted
at P<0.05, and statistical analyses were performed using R
software (R Development Core Team, 2011).
Results
Patient data are detailed in Table I. Overall, 93% of the patients
included in this study underwent concomitant chemoradiotherapy
(CCRT). Cisplatin was used in all of these patients.
 | Table I.Patient data. |
Table I.
Patient data.
| Characteristic | Valuesa (n=14) |
|---|
| Age (years), median
(range) | 64 (41–87) |
| Sex |
|
| Male | 12 (86) |
|
Female | 2 (14) |
| Histology |
|
| Squamous
cell carcinoma | 13 (93) |
| Adenoid
cystic carcinoma | 1 (7) |
| Primary tumor
site |
|
|
Oropharynx | 6 (44) |
| Oral
cavity | 2 (14) |
|
Nasopharynx | 2 (14) |
| Neck
(unknown primary) | 2 (14) |
| Paranasal
cavity | 1 (7) |
|
Submandibular gland | 1 (7) |
| Radiation dose
(Gy) |
|
| 70 | 9 (64) |
|
60–70 | 5 (36) |
| Chemotherapy | 13 (93) |
| Surgery for head and
neck cancer | 6 (43) |
| Period from
completion of RT and second visitb (months), median (range) | 45 (5–76) |
| No. of FDG PET-CT
sessions during follow-up period, median (range) | 3 (2–9) |
| Location of
mandibular osteoradionecrosis |
|
|
Unilateral posterior | 10 (72) |
| Bilateral
posterior | 2 (14) |
|
Anterior | 1 (7) |
| Bilateral
posterior and anterior | 1 (7) |
Fleiss' kappa value (inter-observer reliability) was
0.77. Cohen's kappa values (intra-observer reliability) of observer
1, 2, and 3 were 1, 0.81, and 0.76, respectively. At the second
visit (i.e., the time when patients were reintroduced to our
department for the treatment of mandibular ORN), the most common
ORN type, according to the PET classification, was the extensive
type (43%), followed by the localized type (36%) and the spot type
(21%). The significant difference of SUVmean (P=0.022)
but not SUVmax (P=0.075) among three types was found.
However, there was no significant difference in both
SUVmean and SUVmax between extensive and
localized types, extensive and spot types, and localized and spot
types. The increased area of FDG uptake around mandibular ORN was
found retrospectively on post-treatment follow-up FDG-PET CT in 50%
of patients. The types of changes of PET classification were the
spot type to localized type in 36% and the localized type to
extensive type in 14% (Table
II).
 | Table II.Fluorodeoxyglucose accumulation. |
Table II.
Fluorodeoxyglucose accumulation.
| Parameter | Valuesa (n=14) | SUVmean
median (range) | SUVmax
median (range) |
|---|
| PET
classificationb at
second visit |
|
|
|
|
Extensive | 6 (43) | 4.94 (3.36–6.94) | 9.1 (4.83–13.48) |
|
Localized | 5 (36) | 4.19 (3.54–4.64) | 6.16 (5.62–8.47) |
| Spot | 3 (21) | 2.96 (2.78–3.27) | 4.42 (3.84–6.29) |
|
P-valuec |
| 0.022 | 0.075 |
| Increased FDG
accumulation before the second visitd |
|
|
|
|
Total | 7 (50) |
|
|
| ‘Spot’ to
‘localized’ | 5 (36) |
|
|
|
‘Localized’ to
‘extensive’ | 2 (14) |
|
|
In Table III, data
are presented regarding the association between the range of FDG
accumulation and the type of treatment used for mandibular ORN. In
this study, 57% of the patients were treated conservatively. Among
them, only one patient underwent HBO. In all, 6 of the 14 patients
(43%) required surgical intervention. Four underwent segmental
mandibulectomy for extirpation of the disease with simultaneous
reconstruction using a free fibula osteocutaneous flap, and two
underwent segmental mandibulectomy to control severe infection.
Among the six patients classified as having extensive type ORN at
the second visit, four had a pathologic fracture and an
orocutaneous fistula. Significantly more patients with
extensive-type ORN at the second visit required surgical
intervention (P=0.026).
 | Table III.Association between fluorodeoxyglucose
accumulation and type of treatment for 14 patients. |
Table III.
Association between fluorodeoxyglucose
accumulation and type of treatment for 14 patients.
| PET classification at
second visit | No. of
patientsa (n=14) | P-valueb |
|---|
| Conservative
treatment |
| 0.026 |
| Extensive
accumulation | 1 (7) |
|
| Localized
accumulation | 4
(29) |
|
| Spot
accumulation | 3
(21) |
|
| Surgical
treatment |
|
|
|
Extensive accumulation | 5
(36) |
|
|
Localized accumulation | 1 (7) |
|
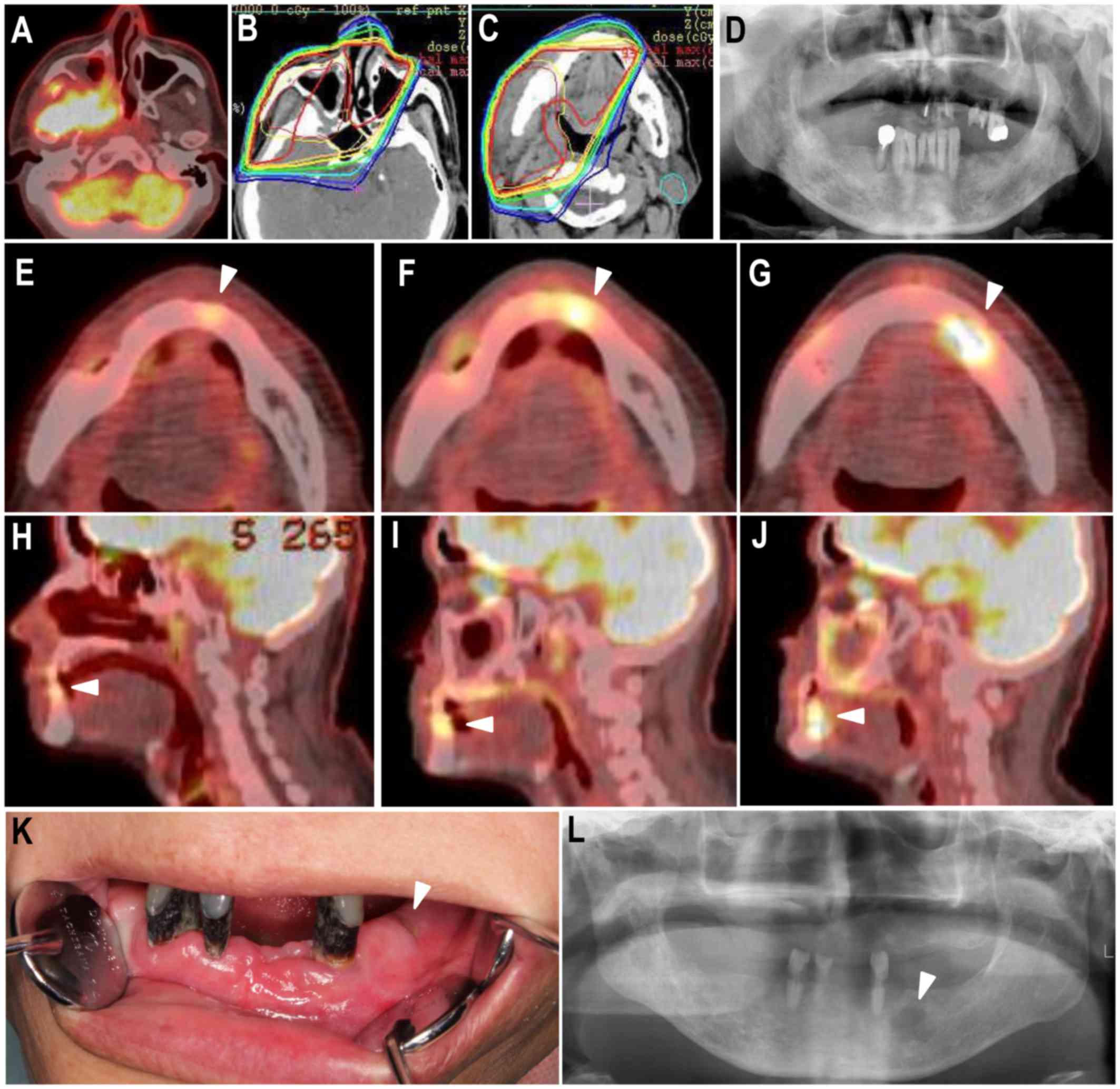
Representative cases are shown in Figs. 2 and 3. A 58-year-old man was re-referred to our
department for evaluation of left lower jaw pain. He previously
underwent CCRT for right maxillary carcinoma in our hospital
(Fig. 2). Prophylactic tooth
extraction was performed before initiating CCRT in our department
(Fig. 2). The patient had pain and
swelling in the left mental region at 4 years 5 months after CCRT
completion. Retrospective evaluation of the post-treatment
follow-up PET CT revealed sequential uptake of FDG (Fig. 2). The extent of FDG uptake was slight
(same signal as non-specific uptake) on PET CT at 2 years 2 months
after CCRT completion (Fig. 2). On
PET CT at 3 years 1 month after CCRT, we found localized
accumulation of FDG around the left mandibular canine (Fig. 2). On PET CT 4 years after CCRT, the
areas of FDG accumulation had increased around the osteolytic
region and protruded into the lingual soft tissue. Hence, the type
of FDG accumulation was extensive (PET classification) (Fig. 2). At the second visit, only a small
fistula with pus discharge was found in the left mandibular molar
region (Fig. 2). However, the
panoramic radiographic image obtained at the second visit showed
bone resorption in the left mandibular molar region (Fig. 2). It was diagnosed as mandibular ORN.
The patient is currently undergoing conservative therapy that
includes repeated local irrigation, with antibiotic administration
only when absolutely necessary.
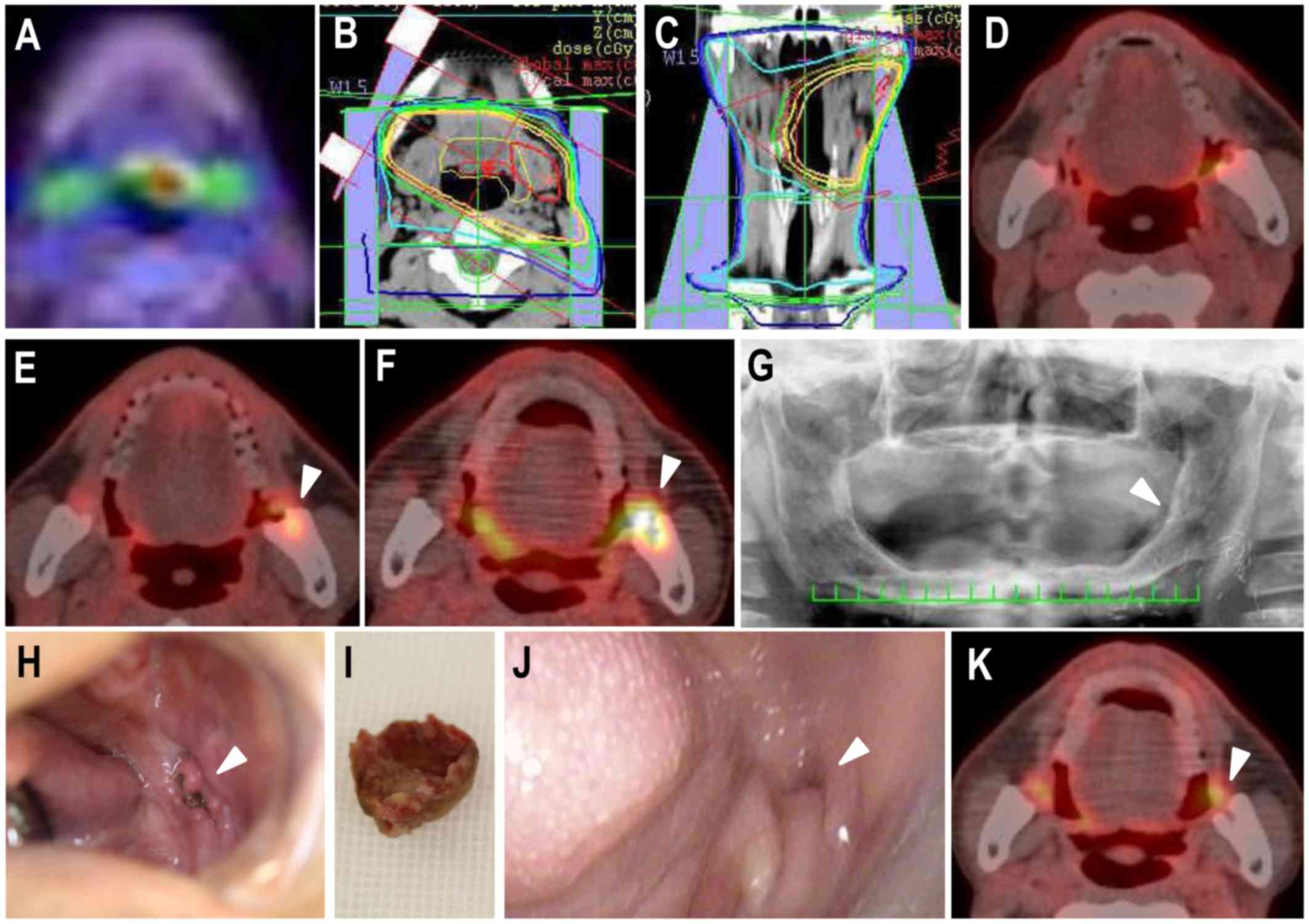
A 64-year-old man was re-referred for evaluation of
left lower jaw pain. He previously underwent CCRT for left
oropharyngeal carcinoma in our hospital (Fig. 3) and an oral examination before CCRT
initiation in our department. The patient had pain and swelling in
the left mandibular molar region at 5 years 10 months after
completion of CCRT. Retrospective evaluation of the post-treatment
follow-up PET CT revealed sequential FDG uptake (Fig. 3). The FDG accumulation was not found
on PET CT at 3 years 7 months after CCRT completion (Fig. 3). However, on PET CT at 4 years 8
months after CCRT, spot accumulation of FDG at the anterior edge of
the left mandibular ramus was found (Fig. 3). On PET CT at 5 years 8 months after
CCRT, an area of bone resorption was found along the left ramus,
changing the type of PET classification to localized accumulation
of FDG (Fig. 3). Although the
panoramic radiographic image at the second visit did not show
obvious bone resorption at the left mandibular ramus (Fig. 3), a fistula with exposure of necrotic
bone was found in the left retromolar region (Fig. 3). He was treated conservatively with
repeated local irrigation and sequestrectomy under local anesthesia
(Fig. 3), which resulted in
epithelialization of the area with necrotic bone exposure (Fig. 3). Recent PET CT showed no FDG
accumulation in the mandible (Fig.
3).
Discussion
We had hypothesized that post-treatment follow-up
with FDG-PET CT to monitor head and neck carcinoma would be useful
for detecting ORN. This retrospective case series study shows the
sequential increase in FDG uptake in patients with mandibular ORN,
indicating that post-treatment follow-up with FDG-PET CT has the
potential not only to evaluate cancer recurrence and metastasis but
also to detect and help us understand the disease conditions of
ORN.
We introduced a novel classification of ORN based on
the range of FDG accumulation in relevant tissues. In the PET
classification of ORN, the spot type probably reflects inflammation
due to marginal or apical periodontitis. ORN can develop in
odontogenic foci (e.g., periodontal and apical disease) or in cases
of failure to heal after dental extraction (10). As shown in Fig. 2, ORN sequentially progressed from
local odontogenic foci that exhibited spot accumulation of FDG. The
spot accumulation of FDG in the mandible on post-treatment
follow-up FDG-PET CT indicates a latent lesion that could cause
ORN. Early detection of such latent lesions based on spot
accumulation of FDG allows prompt initiation of conservative
treatment, such as local irrigation and dental treatment.
Importantly, ORN can also occur spontaneously (10). As shown in Fig. 3, ORN can occur in edentulous
patients, so the lesion cannot be detected on plain radiography
alone. Localized FDG accumulation reveals lesions that are at risk
of being overlooked (or not appearing at all) on plain
radiography.
Contrast-enhanced CT or magnetic resonance imaging
(MRI) examination is routinely performed for cancer follow-up, and
in general, are taken more frequently than PET CT. However, CT for
cancer follow-up is not thin-slice, therefore, it is often
difficult to detect early ORN. It is probably difficult for
attending doctors (i.e., otolaryngologists, radiation oncologists,
and medical oncologists) and radiologists who are not used to
diagnose jaw osteomyelitis to detect early ORN with MRI alone. In
contrast, FDG accumulation is easy to be detected. Taken together,
if attending doctors or radiologists detect spot or localized FDG
accumulation in the mandible on routine follow-up PET CT, it would
be better to consider the introduction to oral and maxillofacial
surgeons or dental oncologists.
In the present study, we found a significantly
higher rate of patients who required surgical interventions in the
extensive-type group (PET classification). Interestingly, a recent
study of MRONJ showed that the extent of FDG uptake predicted the
surgical outcome (11). The authors
showed that FDG uptake extending below the mandibular canal was
more likely to require segmental resection, and they concluded that
FDG-PET CT could provide additional treatment planning information
that did not necessarily correlate with the clinical or CT findings
(11). We think that the range of
FDG accumulation in extensive-type ORN (PET classification)
reflects the inflammation in surrounding soft tissues as the result
of infection of necrotic bone. In this study, patients with
extensive-type ORN mostly had pathologic fractures and orocutaneous
fistulas with chronic pus drainage that caused severe pain and
decreased quality of life. They therefore required surgical
intervention. Another important point in extensive-type ORN is the
differentiation from tumor recurrence. In extensive-type ORN, an
incisional biopsy of surrounding soft tissues should be performed
to exclude tumor recurrence before surgical intervention.
Thus, to avoid invasive procedures, early
intervention before ORN progresses to such an extent that FDG
accumulation spreads to the surrounding soft tissues is important.
In this study, there was a 43% incidence of extensive-type ORN at
the second visit. It is important that dental oncologists continue
routine follow-up in patients who have undergone RT for head and
neck malignancy. They must recognize, however, that oral
examination and plain radiography alone are not enough to detect
latent lesions in some patients. Therefore, we recommend that
dental oncologists assess post-treatment follow-up FDG-PET CT for
early detection of potential foci in the jaw that may portend ORN,
similar to the manner in which radiation oncologists, medical
oncologists, and head and neck surgeons evaluate the presence or
absence of cancer recurrence or metastasis.
This study showed that the incidence of increased
FDG accumulation areas on follow-up PET CT (i.e., ‘spot’ to
‘localized’ or ‘localized’ to ‘extensive’) was 50% in patients who
developed mandibular ORN (Table
II). The changes of the PET classification were from spot to
localized type in 36% of the areas, and from localized to extensive
type in 14%. If spot-type accumulation is detected on follow-up PET
CT, conservative treatment should be performed. Localized-type
accumulation (PET classification) may be equivalent to
intermediate-stage ORN. Jacobson et al (3) noted that it is difficult to recommend a
definitive treatment course for the intermediate stage of ORN.
Importantly, the localized type has the potential to develop into
the extensive type (i.e., advanced ORN), which mostly requires
surgical intervention. We have no recommended treatment criteria
for localized-type accumulation. Although a randomized controlled
trial concluded that HBO is no better than placebo (12), HBO or medication therapy which has
been attracting attention (pentoxifylline-tocopherol-clodronate
therapy) (13) may be necessary for
localized-type accumulation. In this study, one patient with
localized-type accumulation underwent surgery. Even though FDG
accumulation does not protrude into the surrounding soft tissue,
surgical intervention might be better to be selected for patients
who have severe pain probably due to inferior alveolar nerve
injury. In 50% of patients with ORN in this study, FDG accumulation
did not increase (i.e., non-progressive cases). The pathogenetic
difference between the progressive and the non-progressive cases
still remains elusive. As shown in Fig.
3, FDG accumulation disappeared after healing of mandibular
ORN. Follow-up PET CT may be useful not only for the detection of
progression of ORN but also the evaluation of existence of stable
disease or healing of disease.
There were limitations in this study. First, the
study had a small sample size, and it was retrospective. Second,
the cutoff value of the SUV could not be defined. A recent study
that reported the value of FDG-PET CT for diagnosing
implant-related infection of the tibia did not measure the SUV
(14). Another study on
differentiating between tumor recurrence and ORN concluded that the
significant overlap of SUV values in patients with tumor recurrence
and ORN renders SUV values relatively impractical in such cases
(15). Although determining the
cutoff value of SUV for the diagnosis of ORN may be difficult, a
further study should be conducted that focuses on the SUV value of
not only mandibular ORN and periodontal and apical diseases but
also non-specific accumulation after RT for head and neck
cancer.
References
|
1
|
Maesschalck T, Dulguerov N, Caparrotti F,
Scolozzi P, Picardi C, Mach N, Koutsouvelis N and Dulguerov P:
Comparison of the incidence of osteoradionecrosis with conventional
radiotherapy and intensity-modulated radiotherapy. Head Neck.
38:1695–1702. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wanifuchi S, Akashi M, Ejima Y, Shinomiya
H, Minamikawa T, Furudoi S, Otsuki N, Sasaki R, Nibu KI and Komori
T: Cause and occurrence timing of osteoradionecrosis of the jaw: A
retrospective study focusing on prophylactic tooth extraction. Oral
Maxillofac Surg. 20:337–342. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jacobson AS, Buchbinder D, Hu K and Urken
ML: Paradigm shifts in the management of osteoradionecrosis of the
mandible. Oral Oncol. 46:795–801. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Store G and Larheim TA: Mandibular
osteoradionecrosis: A comparison of computed tomography with
panoramic radiography. Dentomaxillofac Radiol. 28:295–300. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fleisher KE, Raad RA, Rakheja R, Gupta V,
Chan KC, Friedman KP, Mourtzikos KA, Janal M and Glickman RS:
Fluorodeoxyglucose positron emission tomography with computed
tomography detects greater metabolic changes that are not
represented by plain radiography for patients with osteonecrosis of
the jaw. J Oral Maxillofac Surg. 72:1957–1965. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hakim SG, Bruecker CW, H Ch Jacobsen,
Hermes D, Lauer I, Eckerle S, Froehlich A and Sieg P: The value of
FDG-PET and bone scintigraphy with SPECT in the primary diagnosis
and follow-up of patients with chronic osteomyelitis of the
mandible. Int J Oral Maxillofac Surg. 35:809–816. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
De Winter F, Vogelaers D, Gemmel F and
Dierckx RA: Promising role of 18-F-fluoro-D-deoxyglucose positron
emission tomography in clinical infectious diseases. Eur J Clin
Microbiol Infect Dis. 21:247–257. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Demirev A, Weijers R, Geurts J, Mottaghy
F, Walenkamp G and Brans B: Comparison of [18 F]FDG PET/CT and MRI
in the diagnosis of active osteomyelitis. Skeletal Radiol.
43:665–672. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wahl MJ: Osteoradionecrosis prevention
myths. Int J Radiat Oncol Biol Phys. 64:661–669. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nabil S and Samman N: Incidence and
prevention of osteoradionecrosis after dental extraction in
irradiated patients: A systematic review. Int J Oral Maxillofac
Surg. 40:229–243. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fleisher KE, Pham S, Raad RA, Friedman KP,
Ghesani M, Chan KC, Amintavakoli N, Janal M, Levine JP and Glickman
RS: Does fluorodeoxyglucose positron emission tomography with
computed tomography facilitate treatment of medication-related
osteonecrosis of the jaw? J Oral Maxillofac Surg. 74:945–958. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Annane D, Depondt J, Aubert P, Villart M,
Géhanno P, Gajdos P and Chevret S: Hyperbaric oxygen therapy for
radionecrosis of the jaw: A randomized, placebo-controlled,
double-blind trial from the ORN96 study group. J Clin Oncol.
22:4893–4900. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Robard L, Louis MY, Blanchard D, Babin E
and Delanian S: Medical treatment of osteoradionecrosis of the
mandible by PENTOCLO: preliminary results. Eur Ann Otorhinolaryngol
Head Neck Dis. 131:333–338. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shemesh S, Kosashvili Y, Groshar D,
Bernstine H, Sidon E, Cohen N, Luria T and Velkes S: The value of
18-FDG PET/CT in the diagnosis and management of implant-related
infections of the tibia: A case series. Injury. 46:1377–1382. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Alhilali L, Reynolds AR and Fakhran S:
Osteoradionecrosis after radiation therapy for head and neck
cancer: Differentiation from recurrent disease with CT and PET/CT
imaging. AJNR Am J Neuroradiol. 35:1405–1411. 2014. View Article : Google Scholar : PubMed/NCBI
|