Introduction
Muscle enlargement may be due to a variety of benign
conditions, such as exercise hypertrophy, infection, hemorrhage,
myxoma and autoimmune diseases, and malignant conditions, including
cancer metastasis and primary sarcoma or lymphoma (1).
Primary lymphomas of the bone or skeletal muscle are
rare entities. The most frequent among these diseases are primary
bone lymphomas, accounting for 3–5% of all bone tumors and 5% of
all primary extranodal non-Hodgkin lymphomas (NHLs) (2). Three mechanisms of lymphomatous
involvement of the muscle have been described: Direct invasion from
adjacent involved lymph nodes or bone, metastatic spread and, least
commonly, primary muscle lymphoma (1,3). The
treatment of primary skeletal muscle lymphoma relies predominantly
on the type of lymphoma and the prognosis of primary skeletal
muscle lymphoma is generally poor (4).
We herein present a rare case of primary mucle NHL
with a description of the associated clinicopathological findings
and a review of the relevant literature.
Case report
A 41-year-old female patient was referred to Erzurum
Regional Training and Research Hospital with a painful mass in the
right lower extremity that was impeding walking. The patient was
otherwise healthy, with no significant medical history. The
physical examination revealed a painful hard mass with a lobulated
contour, beginning in the proximal third of the right femur and
extending to the semitendinosus and sartorius muscles distally. The
left lower and bilateral upper extremities were normal on physical
examination. All the laboratory tests were normal, apart from an
elevated lactate dehydrogenase level of 1,055 U/l (normal range,
240–480 U/l).
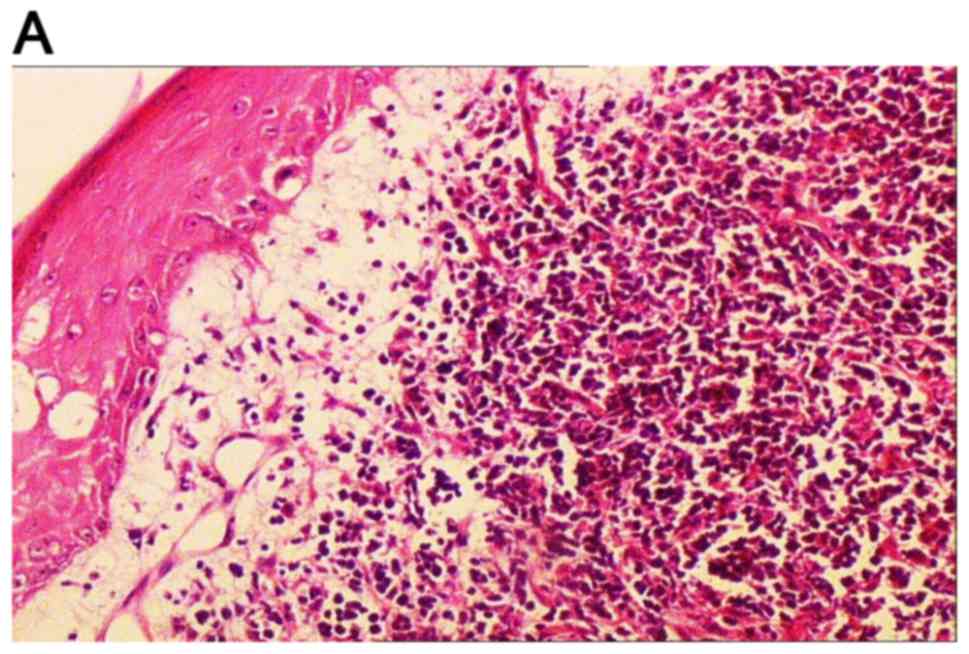
The patient received en bloc resection of the mass,
along with the cutaneous and subcutaneous tissue of the distal
lower right extremity. On histopathological examination, a diffuse
large B-cell lymphoma originating from the muscle with cutaneous
and subcutanenous infiltration was diagnosed. On
immunohistochemical staining, the tumor cells were positive for
CD20, CD79a, paired box protein Pax-5 and CD22, and negative for
CD3, CD5, CD30, CD15 and cyclin-D1; the Ki-67 proliferation index
was 50% (Fig. 1).
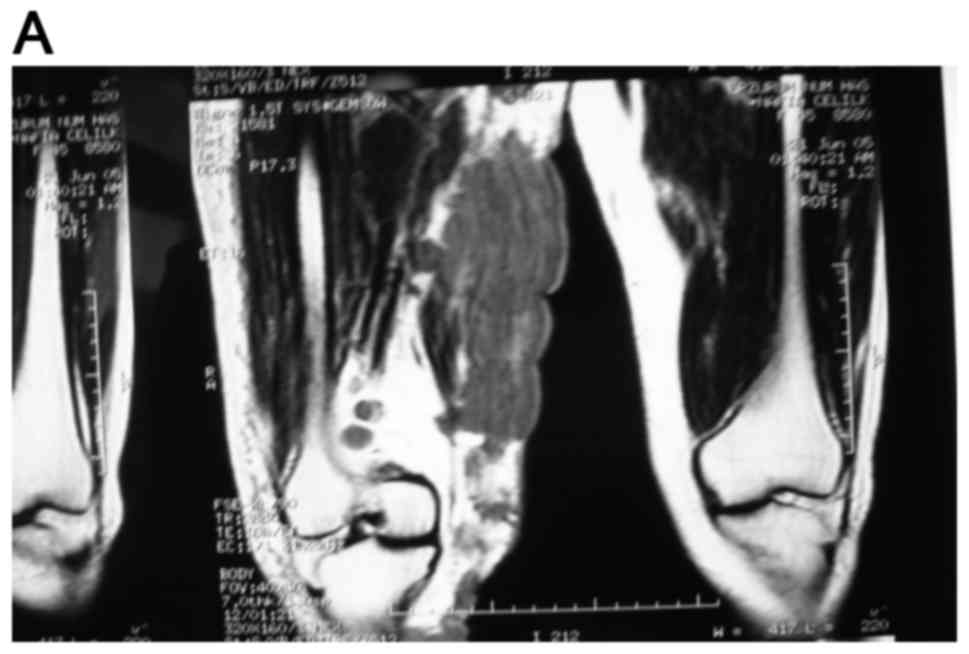
Magnetic resonance imaging (MRI) of the lower
extermities identified multiple solid masses with a lobulated
contour at the medial and posterior part of the femur. The masses
were infiltrating the gracilis and adductor magnus muscles and were
extending to the semitendinosus and sartorius muscles distally and
posteriorly, with cutaneous and subcutaneous fat invasion. The
lesions were isointense to muscle on T1-weighted images (WI) and
hyperintense on T2-WI. The size of all the lesions was 90×64×212 mm
(Fig. 2).
On lymphoma staging with contrast-enhanced computed
tomography (CT) imaging of the chest, abdomen and pelvis, there was
no evidence of lymphadenopathy. Bone marrow biopsy was performed
and revealed a normocellular marrow with trilineage hematopoesis
and no evidence of lymphoma.
The patient underwent chemotherapy with six cycles
of cyclophosphamide, hydroxydaunomycin, oncovin and prednisone
(CHOP). CHOP chemotherapy was initially planned to be administered
with rituximab (R-CHOP). However, after the first dose the patient
developed an allergic reaction (fever, chills, flushing and nausea)
to rituximab, which was thus excluded from the treatment. A
complete radiological response was achieved after six cycles of
treatment. A complete response was maintaned and the patient has
remained disease-free for 1 year.
Discussion
Primary malignant lymphomas of soft tissues are rare
(4). Primary skeletal muscle (PSM)
NHL has rarely been reported (5,6). Lanham
et al reviewed 75 cases of malignant lymphoma arising in
soft tissue and reported the most common histological subtype to be
large-cell type lymphoma (5). Travis
et al reported 8 cases of primary mucle lymphoma among 7,000
malignant lymphomas (0.11%) diagnosed over a 10-year period
(7). Elkouroshy et al
reported an adult male patient diagnosed with primary diffuse large
B-cell lymphoma of the gluteal and adductor muscles, with
aggressive bone involvement (8).
Kounami et al had also reported an anaplastic cell lymphoma
in a 14-year old female patient with a large left inguinal tumor
(9). An increased frequency of PSM
NHL (7%) was detected among AIDS-associated lymphomas (10). Approximately 25% of NHLs are
extranodal (11). Komatsuda et
al investigated a total of 2,147 patients between 1976–1978 and
only found 31 primary muscle lymphomas in that series. Lymphomatous
involvement of muscle has been reported to occur in 1.4% of all
lymphoma cases, with 0.3% occuring in Hodgkin's disease and 1.1% in
NHL (12). Primary NHLs originating
from skeletal muscle may be misdiagnosed as soft tissue tumors,
such as rhabdomyosarcoma, Ewing's sarcoma and metastasis to
skeletal muscle (2).
A mass lesion may be identified on CT or MRI, but a
definitive diagnosis can only be made by biopsy (4,6). Lee
et al recommended that, in patients with a soft tissue mass,
routine plain radiography and MRI should be performed prior to
biopsy (3). Lim et al
suggested that MRI is the most useful modality for assessment of
muscular lymphoma (13). This
condition most commonly affects skeletal muscles of the lower
extremities, pelvis and gluteal regions. On CT, the mass may be
iso- or hypodense (4). Suresh et
al presented a report of MRI findings in 23 skeletal muscle
lymphomas. In that report, all the tumors were of intermediate
T1-WI signal intensity (SI), while 85% of the lesions also
exhibited intermediate T2-WI SI (14). The majorty of these lymphomas have a
B-cell immunophenotype. Two more reports of primary muscle lymphoma
with a T-cell morphology were identified on Medline (15,16).
Primary NHLs originating in skeletal muscles are
quite rare. Primary NHLs derived from lower limb soft tissues may
be mistaken for metastatic tumors. The lesions may be identified on
CT or/and MRI, but the definitive diagnosis relies on biopsy. In
conclusion, masses of the extremities must be carefully assessed
and a biopsy is recommended.
References
|
1
|
Kandel RA, Bédard YC, Pritzker KP and Luk
SC: Lymphoma. Presenting as an intramuscular small cell malignant
tumor. Cancer. 53:1586–1589. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ludwig K: Musculoskeletal lymphomas.
Radiologe. 42:988–992. 2002.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee VS, Martinez S and Coleman RE: Primary
muscle lymphoma: Clinical and imaging findings. Radiology.
203:237–244. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Beggs I: Primary muscle lymphoma. Clin
Radiol. 52:203–212. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lanham GR, Weiss WS and Enzinger FM:
Malignant lymphoma. A study of 75 cases presenting in soft tissue.
Am J Surg Pathol. 13:1–10. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bozzola C, Boldorini R, Ramponi A and
Monga G: Fine needle aspiration cytology in the diagnosis of
non-Hodgkin's lymphomas of the muscle: A report of 2 cases. Acta
Cytol. 49:213–218. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Travis WD, Banks PM and Reiman HM: Primary
extranodal soft tissue lymphoma of the extremities. Am J Surg
Pathol. 11:359–366. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Elkourashy SA, Nashwan AJ, Alam SI, Ammar
AA, El Sayed AM, Omri HE and Yassin MA: Aggressive lymphoma
‘Sarcoma Mimicker’ originating in the gluteus and adductor muscles:
A case report and literature review. Clin Med Insights Case Rep.
9:47–53. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kounami S, Shibuta K, Yoshiyama M, Mitani
Y, Watanabe T, Takifuji K and Yoshikawa N: Primary anaplastic large
cell lymphoma of the psoas muscle: A case report and literature
review. Acta Haematol. 127:186–188. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Raphael M, Gentilhomme O, Tulliez M, Byron
PA and Diebold J: Histopathologic features of high-grade
non-Hodgkin's lymphomas in acquired immunodeficiency syndrome. The
French study group of pathology for human immunodeficiency
virus-associated tumors. Arch Pathol Lab Med. 115:15–20.
1991.PubMed/NCBI
|
|
11
|
Freeman C, Berg JW and Cutler SJ:
Occurrence and prognosis of extranodal lymphomas. Cancer.
29:252–260. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Komatsuda M, Nagao T and Arimori S: An
autopsy case of malignant lymphoma associated with remarkable
infiltration in skeletal muscles (author's transl). Rinsho
Ketsueki. 22:891–895. 1981.(In Japanese). PubMed/NCBI
|
|
13
|
Lim CY and Ong KO: Imaging of
musculoskeletal lymphoma. Cancer Imaging. 13:448–457. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Suresh S, Saifuddin A and O'Donnell P:
Lymphoma presenting as a musculoskeletal soft tissue mass: MRI
findings in 24 cases. Eur Radiol. 18:2628–2634. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Alekshun TJ, Rezania D, Ayala E, Cualing H
and Sokol L: Skeletal muscle peripheral T-cell lymphoma. J Clin
Oncol. 26:501–503. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Robaday S, Héron F, Girszyn N, Humbrecht
C, Levesque H and Marie I: Muscle lymphoma: A case report. Rev Med
Interne. 29:837–839. 2008.(In French). View Article : Google Scholar : PubMed/NCBI
|