Introduction
The lateral retropharyngeal lymph node (LRPLN) is
located between the internal carotid artery and the prevertebral
muscles. The LRPLN is most often seen anterior to the arch of C1,
but is sometimes found at the level of the soft palate. The
uppermost part of the LRPLN anterior to the atlas is known as the
lymph node of Rouvière (1). Lateral
retropharyngeal lymph node (LRPLN) metastasis from oral squamous
cell carcinoma (OSCC) is rare and the prognosis is extremely poor
(2–5). We report an unusual patient with LRPLN
metastasis from squamous cell carcinoma of the upper gingiva and no
progression for more than 7 years. Docetaxel, cisplatin and
fluorouracil (TPF) therapy (6,7) was
performed as induction chemotherapy and it was planned to
subsequently conduct chemoradiotherapy or surgery. As the tumor
only exhibited a transient response to TPF, surgery was selected.
Postoperatively, only radiotherapy was performed and a favorable
outcome was achieved.
Case report
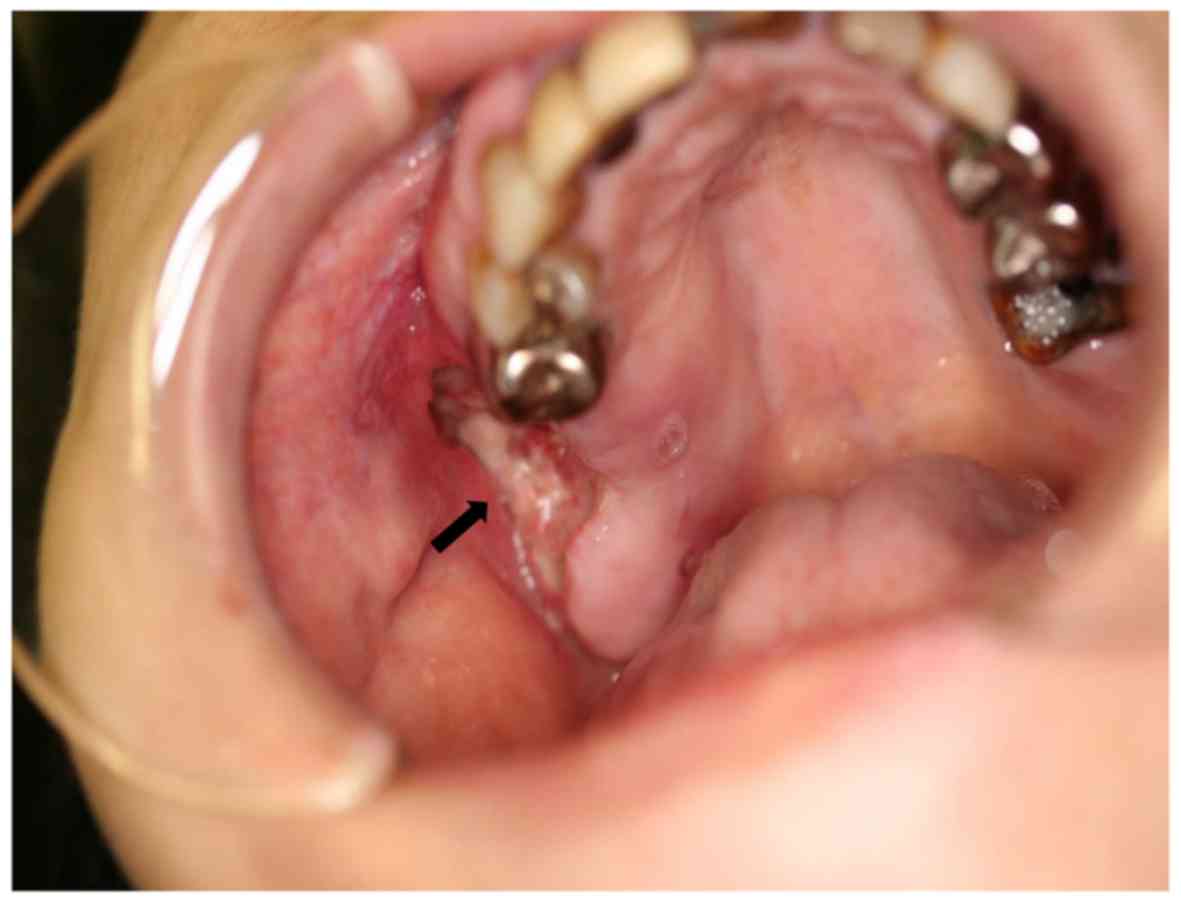
A 56-year-old Japanese woman visited the outpatient
clinic of the Department of Oral Surgery at Tokai University
Hospital in 2009. She had a gingival ulcer near the right maxillary
second molar. This molar had been extracted at another clinic 2
months previously, but healing of the socket was poor. A mobile
lymph node measuring 1.5 cm was palpable in the right cervical
region (Fig. 1). Her medical history
included fatty liver with hepatic impairment and her performance
status (ECOG) was Grade 0. A panoramic X-ray revealed bone
destruction with an uneven margin of the right maxillary molar
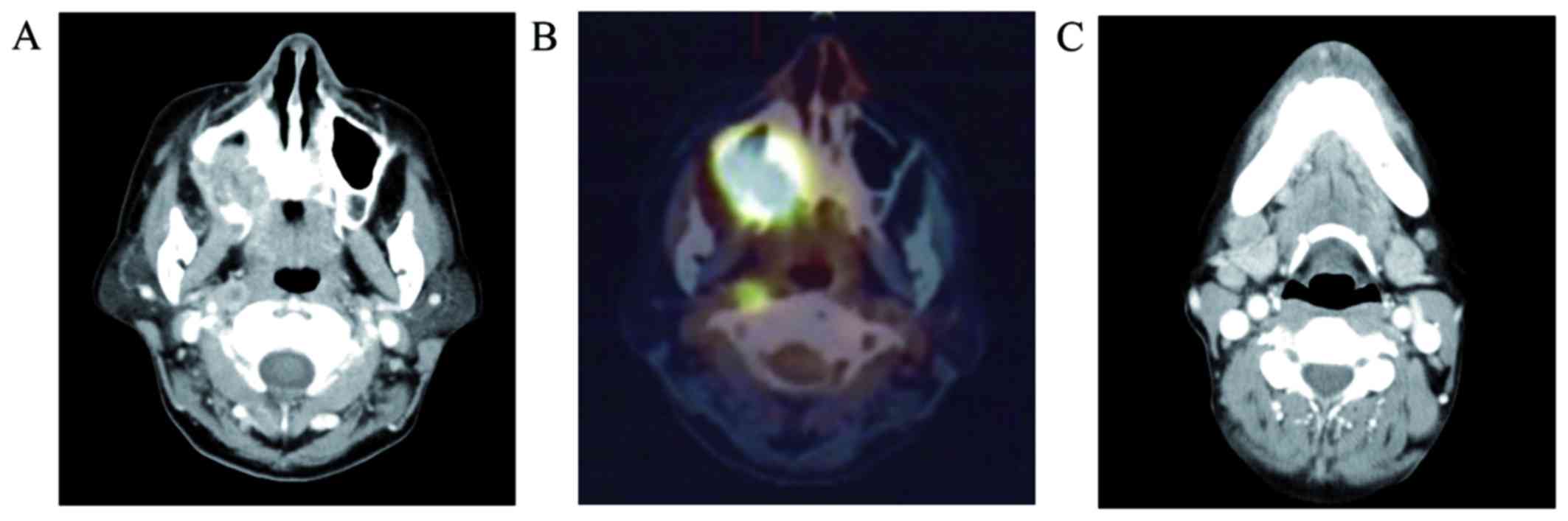
socket. Contrast CT scans showed a tumor with heterogeneous
enhancement that spread from the right maxillary region through the
maxillary sinus, and bone destruction with an uneven margin was
observed. Enlarged lymph nodes with rim enhancement were seen in
the right submandibular, superior internal jugular vein, and LRPLN
regions (Fig. 2). PET/CT also
demonstrated abnormal accumulation at the same sites. The SUVmax of
the primary tumor was 17.2. Biopsy revealed squamous cell carcinoma
and the diagnosis was upper gingival carcinoma T4aN2bM0: Stage IV A
(Fig. 3).
Laboratory tests gave the following results: WBC
8.6×103/µl (Seg+Stab 73.5%, lymphocytes 20.4%, monocytes
5.1%, eosinophils 0.8%, basophils 0.2%), RBC
3.93×106/µl, Hb 12.7 g/dl, Ht 37.3%, Plt
32.3×104/µl, AST 34 U/l, ALT 40 U/l, LDH 202 U/l, ALP
244 U/l, γ-GTP 62 U/l, BUN 13 mg/dl, Cre 0.6 mg/dl, TP 8.1 g/dl,
Glu 103 mg/dl, TG 84 mg/dl, T-CHO 193 mg/dl, Na 141 mEq/l, K 4.1
mEq/l, Cl 107 mEq/l, and T-bil 0.4 mg/dl. Mild hepatic impairment
was observed.
Three courses of the induction chemotherapy were
conducted with docetaxel (Taxotere, Sanofi-Aventis), cisplatin
(CDDP), and fluorouracil (TPF) therapy (docetaxel at 60
mg/m2, CDDP at 60 mg/m2, and fluorouracil at
600 mg/m2) (6,7). At the end of the first course, CT
demonstrated reduction in the size of the primary lesion and lymph
nodes. However, repeat CT after 3 courses showed re-enlargement of
metastatic lymph nodes, although the primary tumor was unchanged.
There was only one adverse event of Grade 3 or higher during
chemotherapy, which was leukopenia.
Thus, the primary tumor and LRPLN responded to the
first course, but regrowth of the LRPLN was observed after 3
courses (Fig. 4). Similarly, the
right submandibular lymph node initially decreased in size, but
then showed regrowth. Therefore, she was judged to have progressive
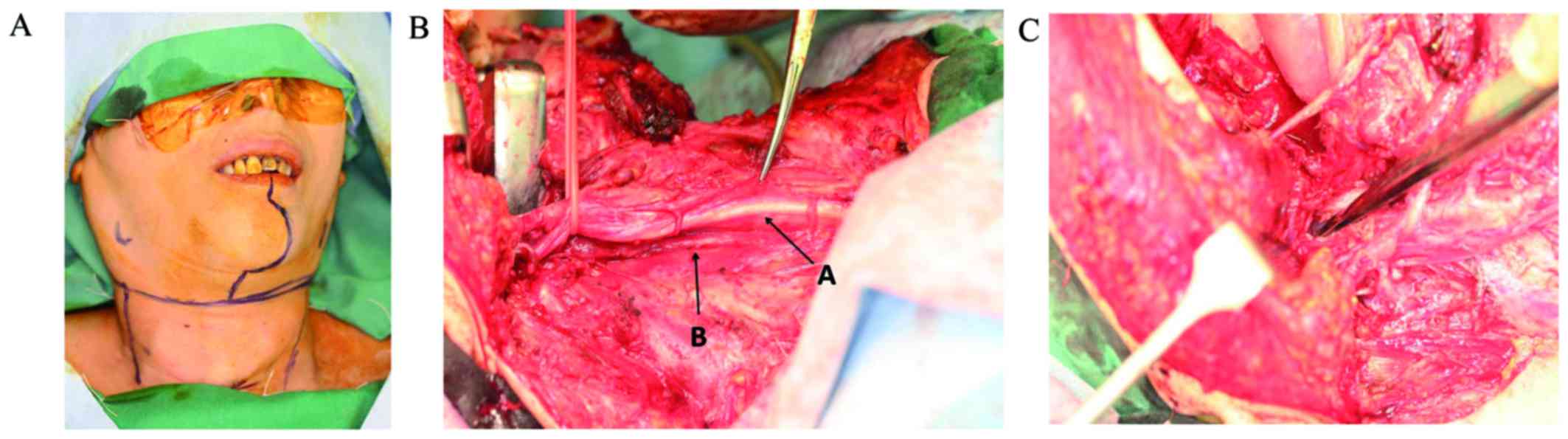
disease and it was decided to perform surgery. After induction of
general anesthesia, surgery was started with tracheotomy followed
by bilateral modified radical neck dissection. A midline lower lip
incision was made and the mandibular swing approach was employed.
The right maxilla was resected. From the dorsal region of the
submandibular gland, fatty tissue was removed from the
parapharyngeal space and it was explored in the cranial direction
until the base of the skull was observed. The fascia of the
superior constrictor muscle was detached. The internal carotid
artery and vagus nerve were exposed, and were pulled aside using
vascular tapes. Then the internal carotid artery, vagus nerve, and
sympathetic nerves were dissected up to the base of the skull and
fatty tissue was removed from the prevertebral fascia to complete
dissection of the retropharyngeal space (Figs. 5 and 6). Postoperatively, only radiotherapy was
administered (60 Gy). At 7 years after surgery, there has been no
sign of relapse or metastasis. The patient has no difficulty with
eating, swallowing, or speaking, and she returned to work
postoperatively.
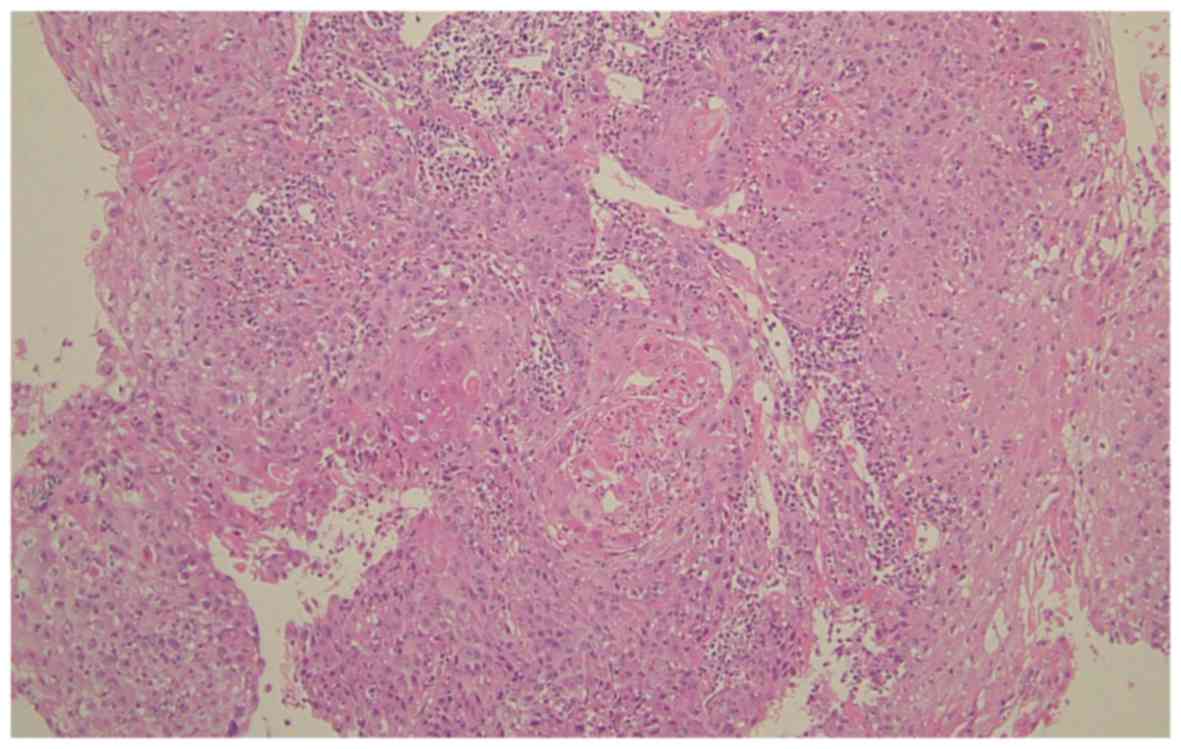
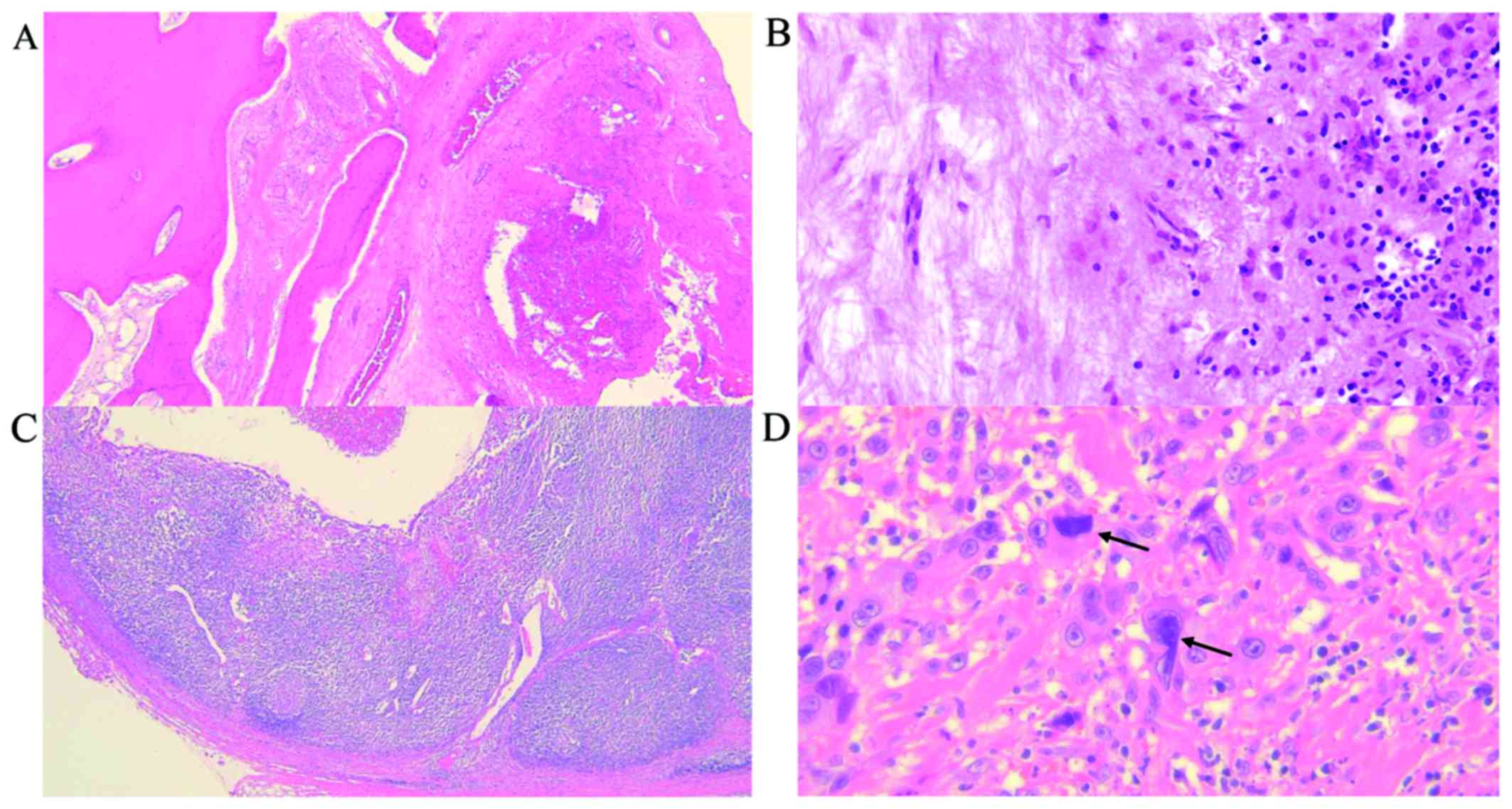
Histopathological examination of resected specimens
from the primary lesion indicated that the sites where tumor cells
presumably had been present were replaced by fibrous tissue showing
mild edema. Inflammatory cells (mainly lymphocytes) were observed
at these sites, but no tumor cells were seen. Some LRPLN sections
showed fibrosis and cyst formation within the structure of the
lymph node, but proliferation of cancer cells was also observed and
part of the capsule was involved. Tumor cells with enlarged,
densely stained nuclei were observed, suggesting changes induced by
chemotherapy (Fig. 7).
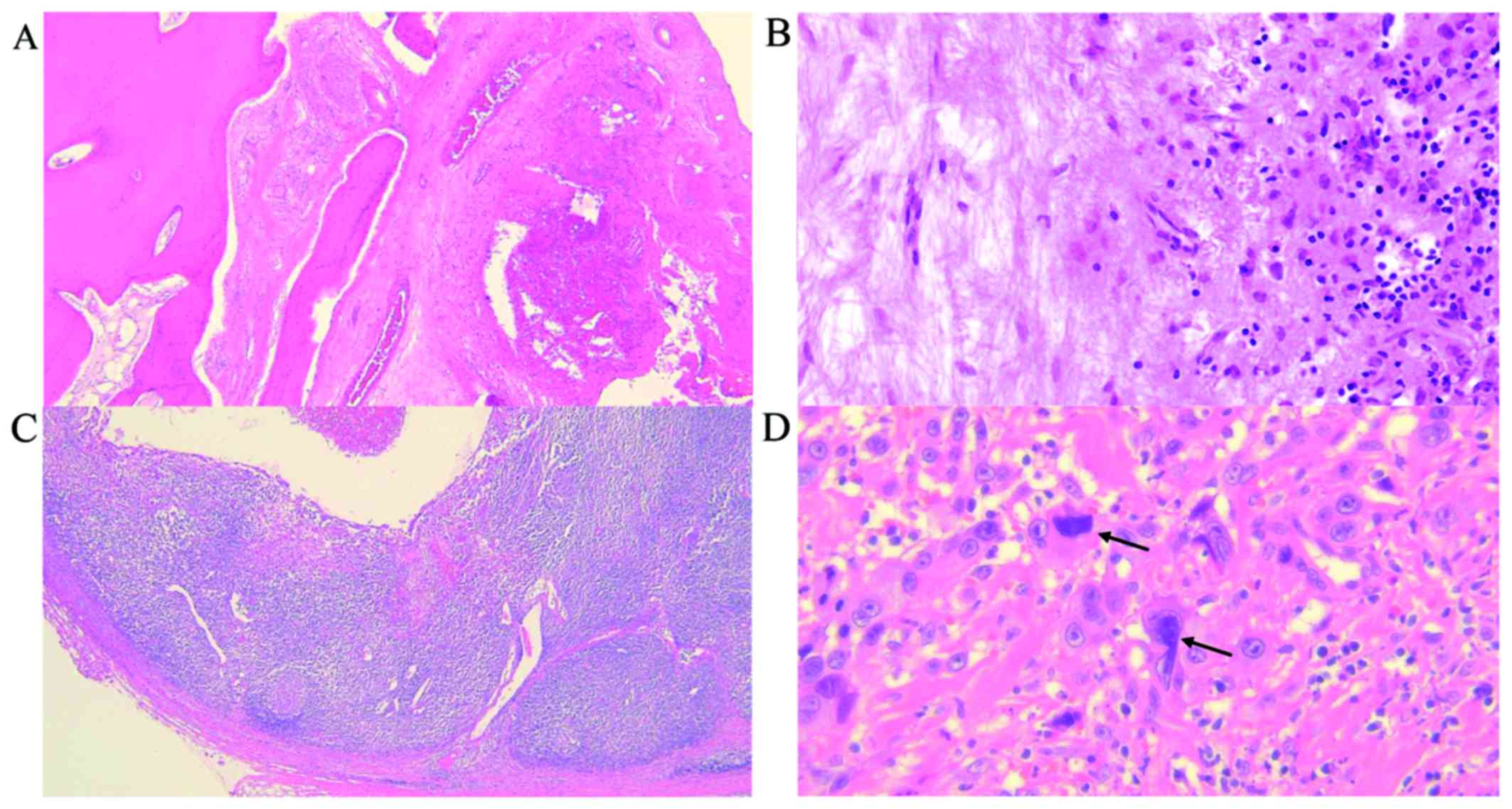 | Figure 7.Histopathological findings (H&E
staining). (A) A section of the primary tumor (magnification, ×40)
shows fibrosis between bone tissues where the tumor may have been
present. (B) Primary tumor (magnification, ×200). Inflammatory
cells (mainly lymphocytes) were observed at these sites, but no
tumor cells were seen. (C) LRPLN (magnification, ×40). Although
fibrosis and cysts are present within the lymph node, proliferation
of cancer cells is also observed. Part of the capsule is involved
by the tumor. (D) LRPLN (magnification, ×400). Tumor cells with
enlarged, densely stained nuclei were observed, suggesting changes
induced by chemotherapy (arrow). H&E, haematoxylin and eosin;
LRPLN, lateral retropharyngeal lymph node. |
The present study was approved by the Institutional
Review Board for Clinical Research of Tokai University (Kanagawa,
Japan). Written informed consent was obtained from the patient for
publication of this case report and any accompanying images.
Discussion
The LRPLN is located between the internal carotid
artery and the prevertebral muscles. The LRPLN is most often seen
anterior to the arch of C1, but is sometimes found at the level of
the soft palate. The uppermost part of the LRPLN anterior to the
atlas is known as the lymph node of Rouvière (1). The incidence of LRPLN metastasis is
reported to be 29.1–88.6% in patients with nasopharyngeal cancer,
16–50% in those with oropharyngeal cancer, and 6–20% in those with
hypopharyngeal cancer (1). The
incidence is reported to be 0.6–1.4% in patients with OSCC
(3,5), while it is 6.9–16% in patients with
maxillary cancer and upper gingival cancer (4,8). Thus,
compared with oral cancer at other sites, the incidence of LRPLN
metastasis is high among patients with upper gingival cancer. At
our institution, LRPLN metastasis was detected in 3 out of 57
patients with upper gingival cancer (5.2%) between 2003 and 2013.
Umeda et al (4) discussed the
route of LRPLN metastasis in patients with upper gingival cancer
and they concluded that, similar to oral cancer at other sites, it
occurs via the submandibular nodes and superior internal jugular
nodes in upper gingival cancer (4).
Lymph channels inside the maxilla also enter both of these lymph
nodes. Furthermore, there may be a route unique to maxillary cancer
that reaches the LRPLN from tumors adjacent to the anterior and
posterior teeth, although it is more developed for the posterior
teeth, which means that tumors growing posteriorly tend to
metastasize to the LRPLN. Moreover, metastasis to the superior
internal jugular lymph nodes could subsequently result in
retrograde metastasis to the LRPLN. Therefore, it is considered
that LRPLN metastasis from upper gingival cancer may be different
to metastasis from other oral cancers.
In many reports about LRPLN metastasis from upper
gingival cancer (2–5), it is stated that metastasis to this
node occurred following resection of the primary tumor or secondary
lymph node metastases and it is common for there to be multiple
metastases to other lymph nodes (9).
Accordingly, it seems that retrograde metastasis may often occur in
patients with secondary lymph node metastasis.
For treatment of LRPLN metastasis, surgery is often
considered in patients with hypopharyngeal cancer (10,11).
Elective neck dissection and adjuvant radiotherapy are recommended.
LRPLN metastasis tends to progress rapidly to involve the carotid
sheath. Accordingly, the prognosis is usually quite poor when LRPLN
metastasis is detected (2–4). Because there are not so many patients
with oral cancer, including upper gingival cancer, evaluation of
treatment outcomes has rarely been conducted.
When a patient first presents with a tumor and LRPLN
metastasis, curative treatment is attempted with chemoradiotherapy
(CRT), radiotherapy alone, neo-adjuvant chemotherapy + surgery, or
CRT + surgery + adjuvant CRT (5).
Alternatively, chemotherapy is given alone as palliative therapy.
Patients with secondary metastasis are often treated by
radiotherapy alone or chemotherapy alone (5). LRPLN metastasis can only be detected by
CT or MRI and many tumors are already non-resectable when detected,
which means that radiotherapy or chemotherapy must be chosen.
On the other hand, there is a small group of
patients in whom surgery is effective (3,4). Upper
gingival cancer that grows posteriorly with metastasis in the deep
cervical area is considered a high-risk tumor for LRPLN metastasis.
Dissection of the parapharyngeal space and retropharyngeal space
should be conducted and resection of the entire lesion together
with the primary tumor should be considered (4,12). There
have been no reports of a favorable outcome with current standard
therapy or CRT according to the National Comprehensive Cancer
Network (NCCN) strategy, in which surgery is followed by high-dose
CDDP (100 mg/m2 on days 1, 22, and 43) (13). When LRPLN metastasis occurs, it may
be debatable whether resection with a sufficient margin is
feasible.
In the present case, induction chemotherapy was
provided and it was planned to subsequently conduct CRT or surgery
(cetuximab was not available in Japan in 2009). However, surgery
was selected as the tumor only transiently responded to TPF
therapy. Since TPF therapy had been conducted prior to surgery,
postoperative radiotherapy was performed alone to improve
tolerability and a favorable outcome was achieved. It is debatable
whether our patient should be judged as resectable or
non-resectable. Induction chemotherapy was reported to be
ineffective for resectable OSCC (14,15).
Standard therapy for non-resectable OSCC is CRT with high-dose CDDP
(13), while induction chemotherapy
with TPF therapy is also regarded as standard therapy in Europe
(16). Among the regimens for
induction chemotherapy, TPF therapy is considered to be the
standard (17). On the other hand, a
prospective Phase III study and a meta-analysis both failed to show
an additive effect of induction chemotherapy (18–20), so
re-appraisal of TPF therapy may be needed.
In conclusion, further discussion about whether
treatment of LRPLN metastasis was appropriate in the present case
seems to be warranted. Since LRPLN metastasis is rare among
patients with oral cancer, a multicenter study will be needed to
accumulate more cases.
References
|
1
|
Coskun HH, Ferlito A, Medina JE, Robbins
KT, Rodrigo JP, Strojan P, Suárez C, Takes RP, Woolgar JA, Shaha
AR, et al: Retropharyngeal lymph node metastases in head and neck
malignancies. Head Neck. 33:1520–1529. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kimura Y, Hanazawa T, Sano T and Okano T:
Lateral retropharyngeal node metastasis from carcinoma of the upper
gingiva and maxillary sinus. AJNR Am J Neuroradiol. 19:1221–1224.
1998.PubMed/NCBI
|
|
3
|
Nishida M, Yasuda S, Murakami K, Yamamura
I, Nagata Y and Iizuka T: Retropharyngeal lymph node metastases
from oral cancer: A report of 2 patients. J Oral Maxillofac Surg.
63:410–412. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Umeda M, Shigeta T, Takahashi H, Kataoka
T, Oguni A, Minamikawa T, Shibuya Y, Yokoo S and Komori T:
Metastasis to the lateral retropharyngeal lymph node from squamous
cell carcinoma of the oral cavity: Report of three cases. Int J
Oral Maxillofac Surg. 38:1004–1008. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tseng JR, Ho TY, Lin CY, Lee LY, Wang HM,
Liao CT and Yen TC: Clinical outcomes of patients with oral cavity
squamous cell carcinoma and retropharyngeal lymph node metastasis
identified by FDG PET/CT. PLoS One. 8:e797662013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vermorken JB, Remenar E, van Herpen C,
Gorlia T, Mesia R, Degardin M, Stewart JS, Jelic S, Betka J, Preiss
JH, et al: Cisplatin, fluorouracil and docetaxel in unresectable
head and neck cancer. N Engl J Med. 357:1695–1704. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Posner MR, Hershock DM, Blajman CR,
Mickiewicz E, Winquist E, Gorbounova V, Tjulandin S, Shin DM,
Cullen K, Ervin TJ, et al: Cisplatin and fluorouracil alone or with
docetaxel in head and neck cancer. N Engl J Med. 357:1705–1715.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Watarai J, Seino Y, Kobayashi M, Shindo M
and Kato T: CT of retropharyngeal lymph node metastasis from
maxillary carcinoma. Acta Radiol. 34:492–495. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tauzin M, Rabalais A, Hagan JL, Wood CG,
Ferris RL and Walvekar RR: PET-CT staging of the neck in cancers of
the oropharynx: Patterns of regional and retropharyngeal nodal
metastasis. World J Surg Oncol. 8:702010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Amatsu M, Mohri M and Kinishi M:
Significance of retropharyngeal node dissection at radical surgery
for carcinoma of the hypopharynx and cervical esophagus.
Laryngoscope. 111:1099–1103. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kamiyama R, Saikawa M and Kishimoto S:
Significance of retropharyngeal lymph node dissection in
hypopharyngeal cancer. Jpn J Clin Oncol. 39:632–637. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Umeda M, Minamikawa T, Komatsubara H,
Ojima Y, Shibuya Y, Yokoo S and Komori T: En bloc resection of the
primary tumour and cervical lymph nodes through the parapharyngeal
space in patients with squamous cell carcinoma of the maxilla: A
preliminary study. Br J Oral Maxillofac Surg. 43:17–22. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pfister DG, Spencer S, Brizel DM, Burtness
B, Busse PM, Caudell JJ, Cmelak AJ, Colevas AD, Dunphy F, Eisele
DW, et al: Head and neck cancers, Version 2.2014. Clinical practice
guidelines in oncology. J Natl Compr Canc Netw. 12:1454–1487. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Marta GN, Riera R, Bossi P, Zhong LP,
Licitra L, Macedo CR, de Castro Junior G, Carvalho AL, William WN
Jr and Kowalski LP: Induction chemotherapy prior to surgery with or
without postoperative radiotherapy for oral cavity cancer patients:
Systematic review and meta-analysis. Eur J Cancer. 51:2596–2603.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lau A, Li KY, Yang WF and Su YX: Induction
chemotherapy for squamous cell carcinomas of the oral cavity: A
cumulative meta-analysis. Oral Oncol. 61:104–114. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Grégoire V, Lefebvre JL, Licitra L and
Felip E: EHNS-ESMO-ESTRO Guidelines Working Group: Squamous cell
carcinoma of the head and neck: EHNS-ESMO-ESTRO Clinical Practice
Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 21
Suppl 5:v184–v186. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Teo M, Karakaya E, Young CA, Dyker KE,
Coyle C, Sen M and Prestwich RJ: The efficacy of induction
chemotherapy with docetaxel, cisplatin and 5-fluorouracil combined
with cisplatin concurrent chemoradiotherapy for locally advanced
head and neck squamous cell carcinoma: A matched pair analysis.
Clin Oncol (R Coll Radiol). 25:647–653. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhang L, Jiang N, Shi Y, Li S, Wang P and
Zhao Y: Induction chemotherapy with concurrent chemoradiotherapy
versus concurrent chemoradiotherapy for locally advanced squamous
cell carcinoma of head and neck: A meta-analysis. Sci Rep.
5:107982015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hitt R, Grau JJ, López-Pousa A, Berrocal
A, García-Girón C, Irigoyen A, Sastre J, Martínez-Trufero J,
Brandariz Castelo JA, Verger E, et al: A randomized phase III trial
comparing induction chemotherapy followed by chemoradiotherapy
versus chemoradiotherapy alone as treatment of unresectable head
and neck cancer. Ann Oncol. 25:216–225. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Budach W, Bölke E, Kammers K, Gerber PA,
Orth K, Gripp S and Matuschek C: Induction chemotherapy followed by
concurrent radio-chemotherapy versus concurrent radio-chemotherapy
alone as treatment of locally advanced squamous cell carcinoma of
the head and neck (HNSCC): A meta-analysis of randomized trials.
Radiother Oncol. 118:238–243. 2016. View Article : Google Scholar : PubMed/NCBI
|