Introduction
Nuclear medicine techniques have shown some
advantages over conventional imaging methods such as X-ray, CT,
MRI, because they illustrate functional changes in a patient which
occur before anatomic changes visualized by conventional imaging
methods. The introduction of PET/CT has brought a new quality in
the field of diagnostic tests. It had a significant impact on the
treatment of cancer patients and gives a better insight into the
nature of cancer (1). Whole body
PET/CT scan can immediately detect or is likely to exclude or
confirm distant metastases. Metastases are detected at ~11% of
patients with normal CT and in 41% the result of the PET/CT forces
to change their behavior and upstage cancer patients. In addition,
PET/CT can solve the problems that give inconclusive results of
conventional imaging. According to various authors, the sensitivity
and specificity of PET/CT in melanoma varies 85–100% and
83.3–95.5%, respectively (2).
Melanoma is one of the worst prognosis for
malignancy because of the unique aggressiveness. Every year in USA,
there has been ~87,110 new cases. The most common changes in the
spleen are congenital defects, infectious diseases and inflammatory
vascular disorders, benign and malignant tumors and systemic
diseases. The primary imaging method in the evaluation of the
spleen is ultrasound (USG). Focal lesions in the spleen visible on
ultrasound are generally gentle and non-specific, presents as a
hypoechogenic lesions. Another imaging technique which allows to
evaluate changes in the spleen is CT. Examination without a
contrast agent can visualize calcifications in the spleen, and
after the administration of contrast the normal spleen enhances. In
addition, the spleen can also visualize the MRI, but keep in mind
that the image depends on the sequence and age of the patient
(https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html)
(3,4).
Case report
The 50-year-old woman after thyroidectomy for benign
thyroid cancer was admitted to the Department of Nuclear Medicine
to determine the progression of melanoma and exclude any distant
metastases. The patient had previously been treated
surgically-underwent removal of the right thigh melanoma and the
sentinel lymph nodes biopsy was performed from inguinal. The
examination did not show any metastatic lesions in these lymph
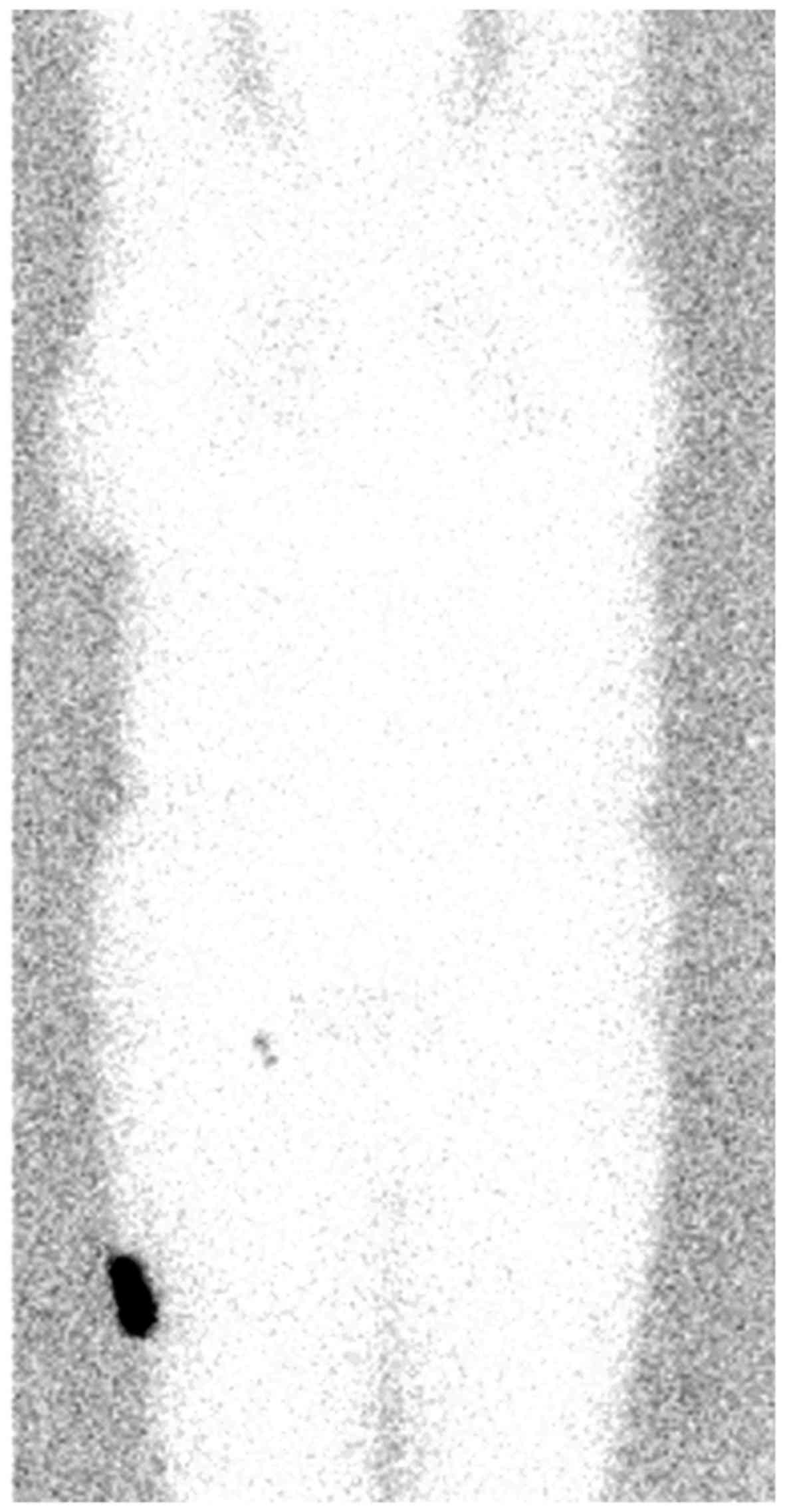
nodes. The sentinel lymph node imaging using Tc99m-nano albumin
colloid showed 2 lymph nodes with increased accumulation of
radioisotope in the right groin and these lymph nodes were removed
and put on a histopathological examination which did not show any
presence of metastatic malignant melanoma cells (Fig. 1).
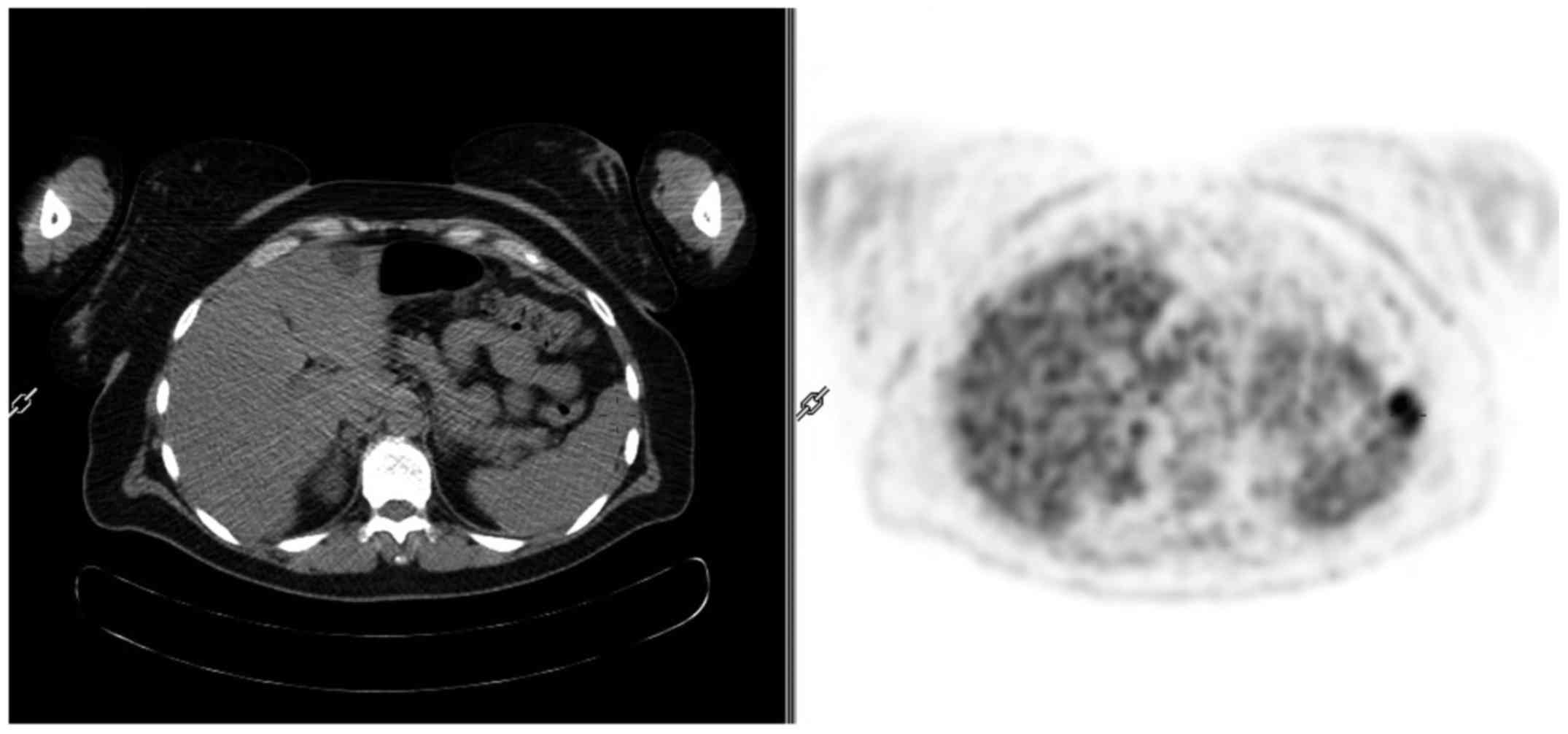
Current physical examination and laboratory test
results revealed no abnormality, LDH level was elevated. In
diagnostic studies performed prior the surgery no changes were
found, except diffuse hepatic steatosis and cysts in segment 4
(Fig. 2).
18F-FDG PET/CT examination was performed
from the top of the head down to the knee. The examination
confirmed the presence of cysts in the liver and also showed a
lesion in the anterior part of the spleen, which was considered as
a melanoma metastasis (SUVmax 6.2) (Fig. 3).
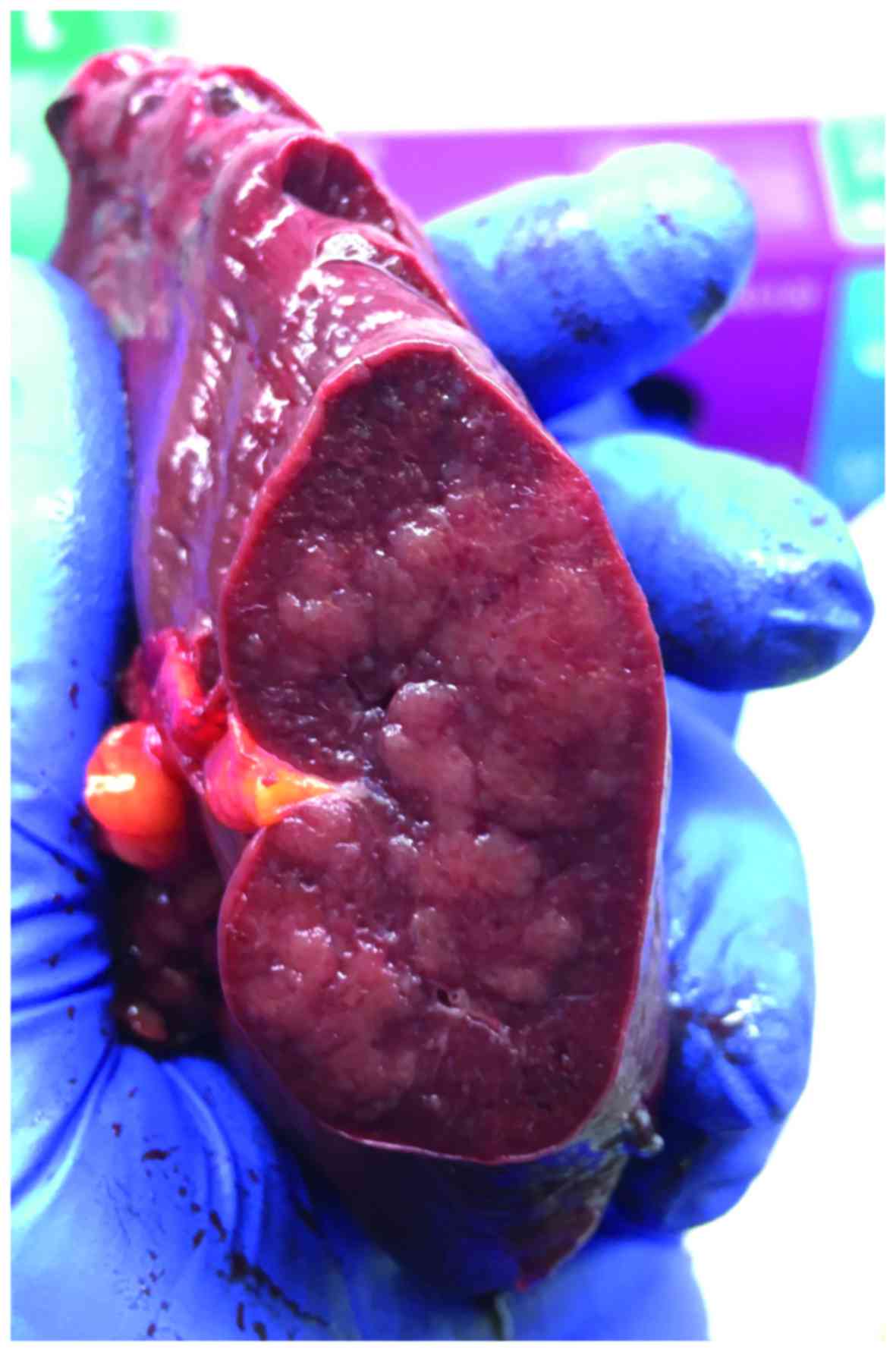
According to the results of PET/CT patient was
admitted to a surgical ward and qualified for surgical
treatment-splenectomy. During surgical procedure, there was no
pathology (except cyst in the liver). The whole spleen was removed
without complications and the spleen was submitted for
histopathological examination (Fig.
4).
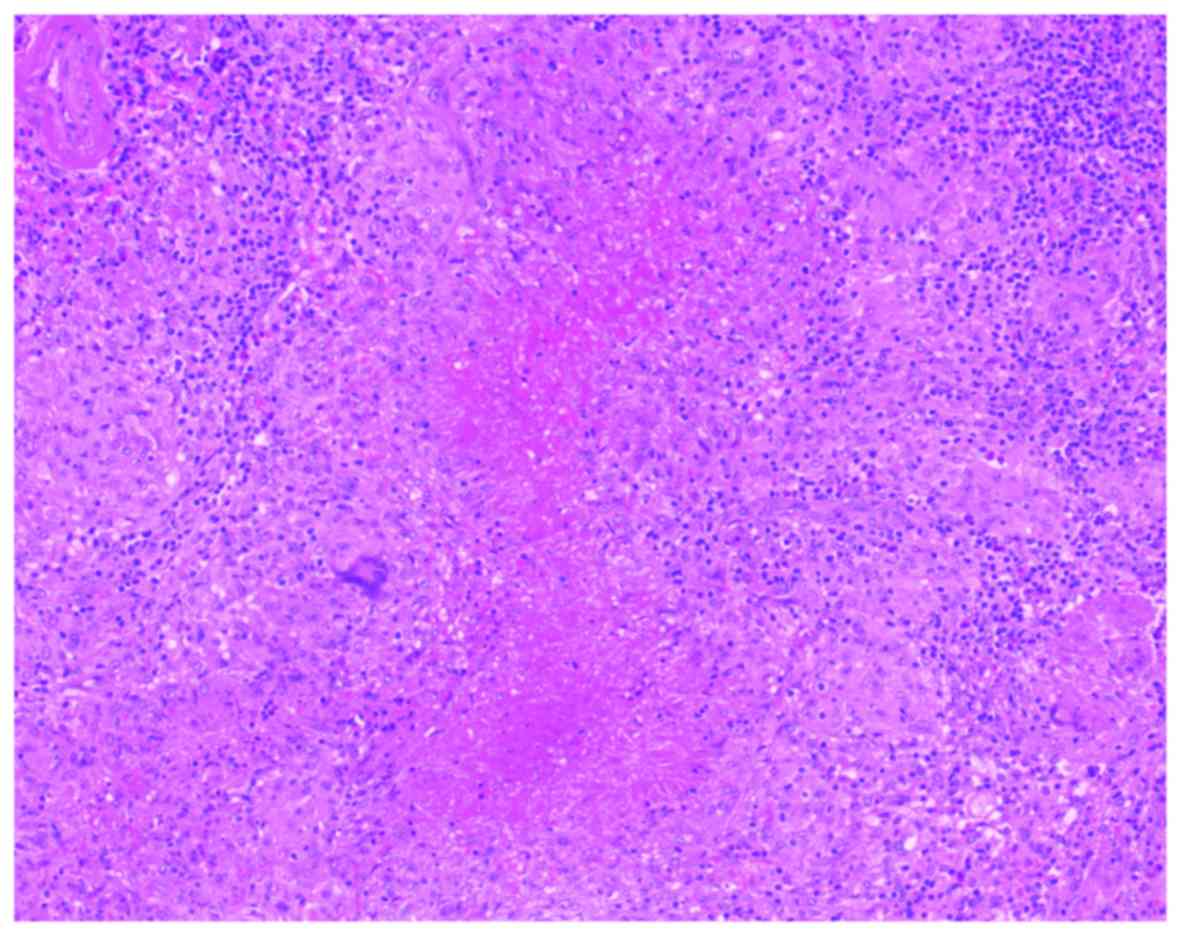
On microscopic examination we found spleen texture
with foci of epithelioid granuloma (consisted with tuberculous
granuloma). Ziehl-Neelsen staining was performed and no tuberculous
bacilli were found. In immunohistochemistry, melanoma markers as
HMB45 and CKA13, were negative. Further diagnostics have been
recommended for specific inflammations and in correlation with the
patient's history allowed to establish tuberculous-like lesions in
the spleen (the young woman was working as a nurse in a
tuberculosis clinic) (Fig. 5).
Discussion
Malignant melanoma accounts for ~2% of all cancers
and is one of the most common skin cancers. The highest number of
cases are recorded in New Zealand, Australia and the USA and in
rich European countries (Norway, Sweden, Switzerland). In men this
is ~1.7% of the cases, and the most common place is the skin of the
trunk, while in women it occurs in 1.9% of the cases and most often
occurs in the limbs. The diagnosis depends on the stage of the
cancer and regional ultrasound lymph nodes are performed to detect
enlarged cells that may contain melanoma metastatic cells. During
the diagnosis it's recommended to perform imaging based on the
identification and testing of the sentinel node and such a
diagnosis was performed in our patient before the procedure
extending the primary excision.
Metastatic melanoma to distant organs usually occurs
at high stage of tumor progression and usually are multiple. They
are also accompanied by metastases to regional lymph nodes.
Sentinel node biopsy is now an indispensable method for assessing
the presence of microsurgical lesions in lymph nodes. In 1999, the
World Health Organization (WHO) stated that sentinel lymph node
biopsy should be a standard practice in skin melanoma patients
without clinical features of metastatic regional lymph nodes.
Immunohistochemistry with monoclonal antibodies is an effective
tool for differentiating melanomas with other skin melanocytic
lesions. Melanoma cells exhibit a specific positive response to the
HMB 45 antibody (www.doctormed.pl).
Human tuberculosis has been present in the world for
10,000 years. Over 4 million cases are registered annually in the
world. Tuberculosis can affect any organ, but most often it locates
in the lungs. The most common site of extrapulmonary tuberculosis
is the pleura, lymph nodes, urinary tract, genitals, bones and
joints, the digestive tract (where it most occurs in the
intestines) and tuberculous meningitis. Tuberculosis-like changes
can occur in a number of diseases: mycobacteriosis, which are
caused by non-tuberculous mycobacteria, sarcoidosis, lymphomas,
brucellosis, fungal infections, foreign body reactions, sarcoid
reactions and the differentiation can be difficult (http://pulmonologia.mp.pl, www.czytelniamedyczna.pl).
As in all cancers, in melanoma pre-staging is a key
factor in choosing the right treatment. According to AJCC
recommendations, staging of malignant melanoma is based on the TNM
system. In the case of melanoma, imaging is targeted to detect
regional and distant metastases so nuclear medicine techniques such
as lymphoscintigraphy of regional lymph nodes which was mentioned
earlier or PET/CT with 18F-FDG play an important role
here. Malignant melanomas are characterized by very high avidity of
FDG, hence the sensitivity of PET/CT with this marker is high so it
is used to evaluate distal metastases (M-staging) and also offers
several additional advantages over conventional CT imaging, for
example sensitivity to detection of small regions that are outside
of the brain and lungs. Over the last decade PET/CT has become a
gold standard in staging, restaging and managing patients with
solid tumors including advanced melanoma (5–7).
18F-FDG PET/CT is a better tool for morphological
imaging in the detection of distant metastases and has replaced MRI
and CT in determining the stage of melanoma (8,9). In
patients with stage I and II, the PET test appears to be useless
and only increases the cost of treatment due to the limitations of
the functional resolution of PET scans which range from 5–6 mm. PET
in melanoma will detect most lymph nodes greater than 10 mm, 83%
larger than 5 mm and only 23% smaller than 5 mm (10). In terms of distant metastasis, Xing
et al (11) performed a
meta-analysis of 2,150 patients with stage III and IV melanoma,
comparable to USG, CT, PET and PET/CT. It turned out that PET/CT
has the highest sensitivity (86%) and specificity (91%) of the
above mentioned imaging methods. PET imaging in advanced melanoma
alone showed 86% sensitivity and 87% specificity in detecting
metastases to lymph nodes, soft tissues and visceral metastases
(12). Schröer-Günther et al
(13), performed meta-analysis,
found that PET with or without CT had a sensitivity of 68–87% and a
specificity of 92–98% in diagnosing advanced melanoma (11–13).
Spleen tuberculosis is an extremely rare form of
tuberculosis. Usually spleen involvement is observed in advanced
stage of tuberculosis and then infects various organs and in
immunocompromised patients with HIV (14). Mostly in FDG PET/CT examination
spleen tuberculosis is seen as multiple lesions with increased FDG
uptake. In our case there was only one lesion in the spleen that's
why this case is so unusually form of tuberculosis. However several
authors describe in their work splenic tuberculosis. Dede et
al (15) described the case of a
29-year-old patient with widespread abdominal pain worsening for 6
mo. In performed exams showed enlarged, thick walled centrally
necrotic mass lesion at the upper pole of the spleen. Chest X-ray
without meaning. After splenectomy and histopathology exams splenic
tuberculosis was confirmed and patients underwent antituberculosis
therapy (15). Joshi et al
(16) also found splenic
tuberculosis in non diabetic, non hypertensive woman who presented
low grade fever, pain in left hypochondriac region and progressive
weight loss for about 2 mo. Abdominal ultrasound showed multiple
hypo echoic lesions and enlarged spleen (16). Gupta et al (17) had 49 year woman with symptoms of
fever of unknown origin lasting for 3 months, with enlarged spleen
on clinical examination and multiple small hypo echoic foci in the
spleen which occurred to be tuberculous etiology on
histopathological examination (17).
Singh et al (18) found
splenic tuberculosis in 35-year-old woman with evening rise of
temperature, decreased appetite, loss of weigh for last 3 months
and recurrent paint in left hypochondriac lasting for a month. An
abdominal ultrasound showed a normal sized spleen multiple hypo
echoic lesions. Other organs showed no significant abnormality and
further evaluation did not show other primary foci of tuberculosis
in lungs or any other organs (18).
In our case, patient did not show any imaging
abnormalities before PET/CT examination including splenomegaly or
enlarged lymph nodes. No tuberculosis history in the family was
noted. Also no fever, chills, weight loss or abdominal pain was
found in the patient and the results of laboratory tests did not
differ from normal. In 18F-FDG PET/CT examination only
one region with increased metabolic activity was found and it was
in the spleen. This example shows that oncological patients can be
a difficult diagnostic problem and the knowledge and experience of
physicians may be a necessary factor in solving the problem and
thus saving patients unnecessary treatment. After one year patient
came back to another 18F-FDG PET/CT examination and no
tuberculosis signs was seen in the patients in whole body.
It should be remembered that abnormal focal
accumulation of radiotracer with limited cancer specificity in
PET/CT examination in organs or tissues in cancer patients should
not be unambiguously taken as a metastatic lesion and sometimes
more diagnostic test if it possible need to be performed.
References
|
1
|
Brikenfeld B and Listewnik M: Nuclear
Medicine, molecular imaging. Wyd. PUM. 2011.(In Polish).
|
|
2
|
Kordek R, Jassem J, Jeziorski A, Kornafel
J, Krzakowski M and Pawlęga J: Oncology, textbook for students and
doctors. Via Medica, Gdańsk. 2007.(In Polish).
|
|
3
|
Windorbska W, Partyka A, Lewandowska A and
Małkowski B: Assessment of diagnostic value of FDG-PET / CT in
diagnosis of melanoma patients. Onkologia. 11:42007.(In
Polish).
|
|
4
|
Vancauwenberghe T, Snoeckx A,
Vanbeckevoort D, Dymarkowski S and Vanhoenacker FM: Imaging of the
spleen: What the clinician needs to know. Singapore Med J.
56:133–144. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Balch CM, Gershenwald JE, Soong SJ,
Thompson JF, Atkins MB, Byrd DR, Buzaid AC, Cochran AJ, Coit DG,
Ding S, et al: Final version of 2009 AJCC melanoma staging and
classification. J Clin Oncol. 27:6199–6206. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Anna N: Pashali; the role of nuclear
medicine in malignant melanoma. J Nucl Med. 6:42015.
|
|
7
|
Powell P, Charles M and Rathan M:
Subramaniam 18F-fdg pet/ct and melanoma: Staging, immune modulation
and mutation-targeted therapy assessment and prognosis. AJR Am J
Roentgenol. 205:259–270. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Steinert HC: PET and PET/CT of malignant
melanomaSkin cancer: A world-wide perspective. Dummer R, Pittelkow
MR, Iwatsuki K, Green A and Elwan MN: Springer; Berlin, Germany:
pp. 379–390. 2011
|
|
9
|
Nanni C, Fantini L, Nicolini S and Fanti
S: Non FDG PET. Clin Radiol. 65:536–548. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Crippa F, Leutner M, Belli F, Gallino F,
Greco M, Pilotti S, Cascinelli N and Bombardieri E: Which kinds of
lymph node metastases can FDG PET detect? A clinical study in
melanoma. J Nucl Med. 41:1491–1494. 2000.PubMed/NCBI
|
|
11
|
Xing Y, Bronstein Y, Ross MI, Askew RL,
Lee JE, Gershenwald JE, Royal R and Cormier JN: Contemporary
diagnostic imaging modalities for the staging and surveillance of
melanoma patients: A meta-analysis. J Natl Cancer Inst.
103:129–142. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Krug B, Crott R, Lonneux M, Baurain JF,
Pirson AS and Vander Borght T: Role of PET in the initial staging
of cutaneous malignant melanoma: Systematic review. Radiology.
249:836–844. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schröer-Günther MA, Wolff RF, Westwood ME,
Scheibler FJ, Schürmann C, Baumert BG, Sauerland S and Kleijnen J:
F-18-fluoro-2-deoxyglucose positron emission tomography (PET) and
PET/computed tomography imaging in primary staging of patients with
malignant melanoma: A systematic review. Syst Rev. 1:622012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cobelschi C, Maier A, Hogea MD, Gheorghiu
AR and Toader I: SplenicTuberculosis-case report. Chirurgia
(Bucur). 111:165–169. 2016.PubMed/NCBI
|
|
15
|
Dede F, Doğan E, Demir M, Sener D, Kös M,
Tad M and Eskioğlu E: Unusual presentation of tuberculosis as a
splenic mass. Tohoku J Exp Med. 210:79–82. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Joshi S, Bankar M, Kagal A, Rane S,
Bharadwaj R and Phadke M: Splenic tuberculosis-a rare case report.
Int J Med Update. 2:38–41. 2007.
|
|
17
|
Gupta PP, Fotedar S, Agarwal D and
Sansanwal P: Tuberculosis of spleen presenting with pyrexia of
unknown origin in a non-immunocompromised woman. Lung India.
25:22–24. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Singh TB, Niyas J, Subhalaxim L, Singh KR,
Singh SK and Singh THB: Splenic tuberculosis-a rare case report.
JMSCR. 3:8454–8457. 2015.
|