Introduction
Carcinoma of the cervical stump rarely occurs in
patients who have previously received a subtotal hysterectomy, and
accounts for 2–5% of all cervical cancer cases worldwide from 1970
(1–3). Barillot et al (1) analyzed 213 cases of cervical stump
carcinoma and they observed that the locoregional control at equal
time points between radiotherapy alone and surgery were very
similar, however the lethal complications of radiotherapy were
lower. Hellström et al (2)
concluded that there was no difference in the longterm prognosis
for radiologically treated squamous cell carcinoma cervical stump
cancer and other cervical carcinomas, however the prognosis for
adenocarcinoma stump cancers was worse than those in an intact
uterus. For the treatment of early cervical stump cancer,
Diaz-Feijoo et al (3)
reported that total laparoscopic radical trachelectomy and
intraoperative sentinel node identification was effective and safe.
To date, there has been no standardized treatment of this type of
cervical neoplasm. The majority of gynecological tumor experts
conform to existing strategies of radiotherapy or laparotomic
abdominal (or laparoscopic) radical surgery. Presentation ≥2-years
following a subtotal hysterectomy is considered to indicate true
cervical stump cancer, whereas an interval of <2-years interval
following subtotal hysterectomy is considered to denote a
‘coincidental’ carcinoma that may have been present at the time of
the subtotal hysterectomy (4–7). In the
present study, 10 cases of patients with cervical stump cancer were
retrospectively analyzed with regard to the clinical
characteristics (including age, clinical stage and histopathology),
treatment and follow-up data. The results suggested that surgery
for cervical stump cancer at an early-stage is a viable and safe
procedure, particularly the laparoscopic approach as this type of
surgery has fewer associated complications, including reduced blood
loss and a shorter recovery time.
Patients and methods
Ethics statement
All the patients were recruited following the
receipt of written consent between January 2006 and October 2016 at
the Anhui Provincial Hospital affiliated to Anhui Medical
University (Hefei, China). The study was reviewed and approved by
the ethics review board of Anhui Provincial Hospital. All
procedures performed in the study were in accordance with the
ethical standards of the institutional research committee and with
the 7th revised edition of the declaration of Helsinki.
Patient characteristics
A total of 10 patients were evaluated with respect
to their medical history, a physical examination (including a
pelvic examination), routine lab work and a chest X-ray; the
diagnosis was determined according to the system of the
International Federation of Gynecology and Obstetrics (FIGO) by two
or more gynecological tumor experts who were blinded to the patient
data. Each patient had a histological diagnosis determined via
biopsy prior to treatment.
The median patient age was 52.4±4.8 years (range
46–61 years). All patients had previously undergone a subtotal
hysterectomy for benign disease such as fibromyoma and
menometrorrhagia. The mean time interval between the subtotal
hysterectomy and diagnosis of cervical stump cancer was 11.4±5.6
years (range, 5–21 years; all patients had an interval of ≥5
years). The clinical data, including tumor stage and histology, are
presented in Table I.
 | Table I.The clinical characteristics of the
cervical stump cancer cases. |
Table I.
The clinical characteristics of the
cervical stump cancer cases.
| Variable | No. patients |
|---|
| Age (years) |
|
| ≤50 | 4 |
|
>50 | 6 |
| Clinical stage |
|
| Carcinoma
in situ | 1 |
|
IB1 | 7 |
| IIA | 2 |
| Histology |
|
| Squamous
carcinoma | 7 |
|
Keratin | 1 |
|
Non-Keratin | 6 |
|
Adenocarcinoma | 2 |
|
High | 1 |
|
Middle | 1 |
|
Low | 0 |
All the patients were followed up twice a year by
gynecologic oncologists for ten years. A complete physical exam,
including a pelvic examination, was performed on each visit.
Vaginal smears and a colposcopy were conducted annually, as were
routine chest X-rays and squamous cell carcinoma antigen studies.
The median time of observation for patients alive at the last
follow-up visit was 33.20±37.78 months (range, 6–120 months).
Treatment
Patients with a cervical cancerous stump diagnosed
as carcinoma in situ were administered a transvaginal
trachelectomy. Patients with a cervical cancer stump diagnosed at
stage IB1/IIA were treated with a radical trachelectomy
and pelvic lymphadenectomy (8). A
total of 5 cases were treated using a laparoscopic procedure: the
laparoscope was placed into position 3 cm above the umbilicus
through an 11-mm umbilical trocar with a direct-puncture, and three
other trocars were introduced in the Trendelenburg position. Two
accessory 12- and 5-mm trocars were then placed under direct
visualization in the iliac fossae, and one 5-mm accessory trocar at
the midline between the umbilicus and the left subcostal margin.
The number and position of trocars were then used to perform a
distal radical trachelectomy and a pelvic lymphadenectomy.
Following inspection of the abdominal cavity, the
retroperitoneal spaces were opened and a systematic bilateral
pelvic lymphadenectomy from the common iliac artery to the inferior
boundary of the circumflex iliac vein was performed. Then, the
paravesical, pararectal, rectovaginal, and vesicovaginal spaces
were fully expanded, thereby delineating the uterosacral ligaments
and the parametria. Uterine vessels were cut and coagulated at
their origin from the hypogastric vessels; the parametrial tissue
and the uterosacral ligaments were also transected by coagulation
and cutting.
Dissection of tissue adhesion, the ureteral tunnel,
urinary bladder and ureteral separation was performed with the aid
of an Ultracision® Harmonic Scalpel (Ethicon, Inc.,
Cincinnati, OH, USA). The uterus-lifting cup was placed into the
cervical cavity to facilitate tissue dissection and the development
of parametria and paracolpia. The proximal paracervical tissue and
the vagina were transected and removed vaginally. The vaginal cuff
was then closed laparoscopically by continuous suture. In total,
four cases were treated with laparotomic abdominal radical
trachelectomy and pelvic lymphadenectomy. A suprapubic catheter was
inserted. Two of the patients subsequently received postoperative
concurrent chemoradiotherapy due to deep stromal invasion. Four
patients were treated with adjuvant chemotherapy (Paclitaxol and
platinum).
Results
Histology
Squamous cell carcinoma was identified in 80% of
cases, with the remaining 20% determined to be adenocarcinoma. This
histological type distribution is similar that reported worldwide
in the NCCN Guidelines® 2015 in which squamous cell
carcinoma accounted for ~80% of all cervical cancer cases and
adenocarcinoma accounted for ~20% of all cases (8–12).
Age
The median age of patients with cervical stump
carcinoma was 52.4 years, similar to the median age of 58 years
reported by Miller et al (4),
compared with 49 years in patients with cervical carcinoma of the
intact uterus.
Clinical presentation
The clinical symptoms included vaginal bleeding
(90%) and abnormal cytology (10%). No other symptoms were observed.
All patients presented with hemoglobin levels of >11 g/dl. The
median interval between the onset of symptoms and a diagnosis was
5.45 months (Table II). In 10% of
cases, the symptoms were present for ~2 years prior to the
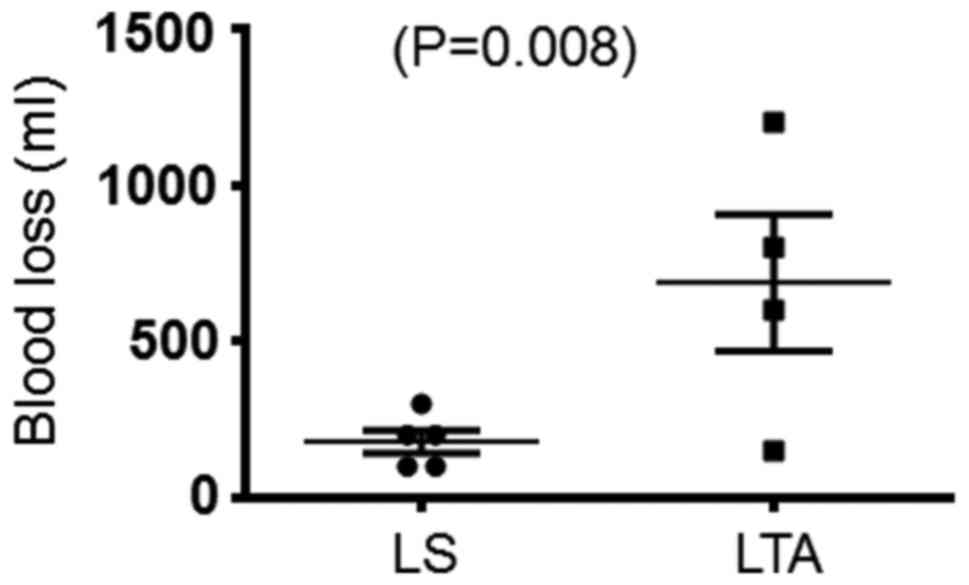
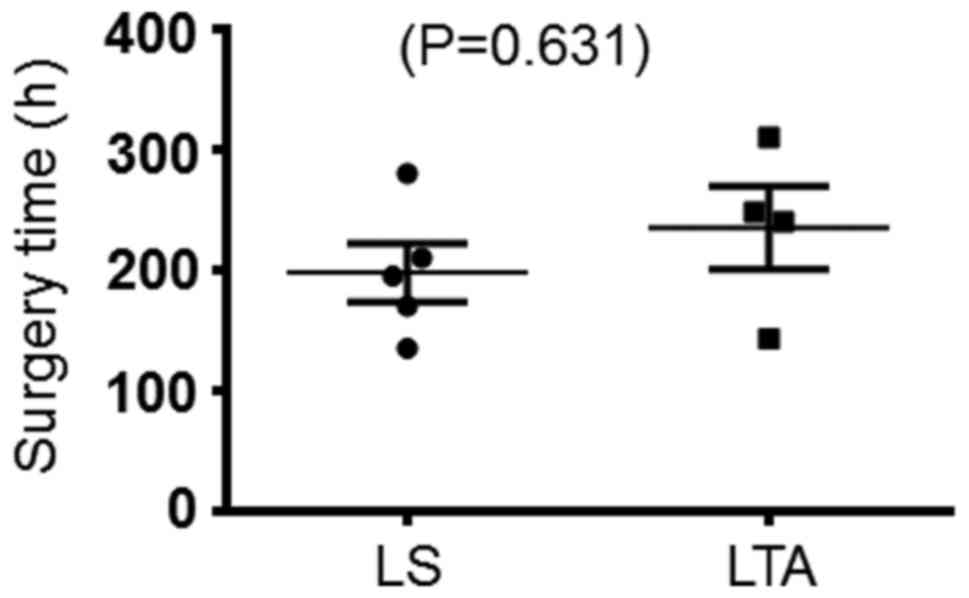
establishment of a diagnosis. The mean operative time was 214.6
min; the mean estimated blood loss was 180.0 ml for laparoscopic
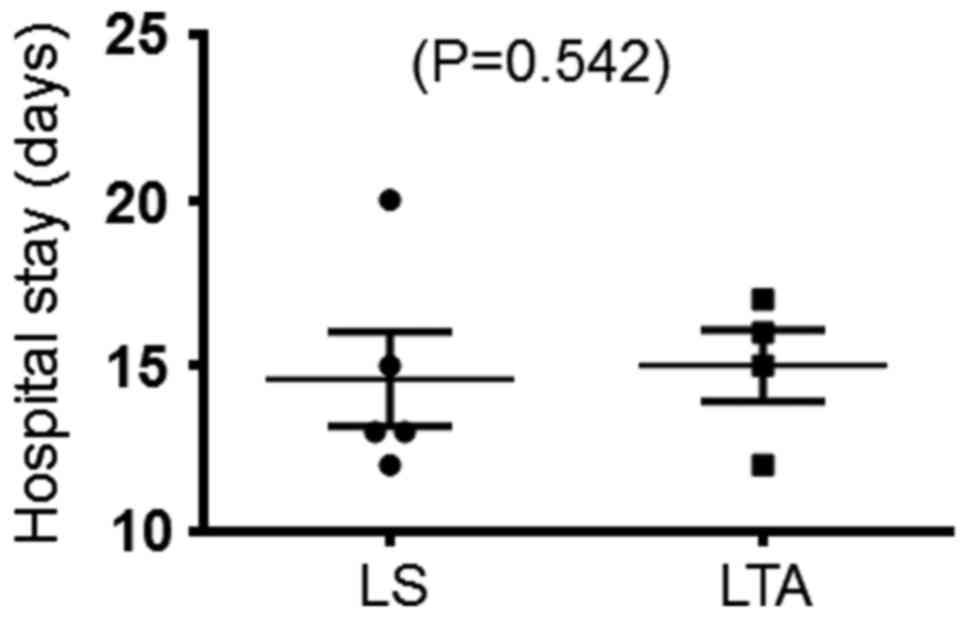
surgery, and 687.5 ml for laparotomic abdominal surgery (Fig. 1); the mean length of the hospital
stay was 14.8 days. The catheters of all patients were removed on
the 21st postoperative day after residual urine volumes of 80 ml.
There was no significant difference in the surgery time and the
duration of hospital stay between the laparoscopic surgery and the
laparotomic abdominal surgery (Figs.
2 and 3). The pathological
characteristics of the patients are presented in Table II. Overall, six patients were
received adjuvant chemotherapy, two of whom also received combined
radiotherapy (Table II).
 | Table II.The pathology patterns and the
adjuvant treatment of patients with cervical stump cancer. |
Table II.
The pathology patterns and the
adjuvant treatment of patients with cervical stump cancer.
| Case | Diagnosis interval
(months) | Differentiation
(Squamous or adenocarcinoma) | Deep stromal
invasion | Parametrium and the
resection margin of the vaginal involvement | LN Metastasis | LVSI | CT | RT | Follow-up
(months) |
|---|
| 1 | 1 | Keratin | <1/2 | Neg. | Neg. | Neg. | No | No | 12 |
| 2 | 2 | Non-Keratin | >2/3 | Neg. | Neg. | Neg. | Yes | No | 60 |
| 3 | 4 | Non-Keratin | >1/2 | Neg. | Neg. | Neg. | Yes | Yes | 12 |
| 4 | 24 | Non-Keratin | >1/2 | Neg. | Neg. | Neg. | Yes | No | 8 |
| 5 | 6 | High | >1/2 | Neg. | Neg. | Neg. | Yes | Yes | 6 |
| 6 | 3 | Non-Keratin | <1/2 | Neg. | Neg. | Neg. | Yes | No | 13 |
| 7 | 0.5 | Middle | >2/3 | Neg. | Neg. | Neg. | Yes | No | 28 |
| 8 | 2 | Non-Keratin | <1/2 | Neg. | Neg. | Neg. | No | No | 6 |
| 9 | 6 | L | L | L | L | L | L | L | 67 |
| 10 | 6 | Non-Keratin | >2/3 | Neg. | Neg. | Neg. | No | No | 120 |
Follow-up and complications
All the patients were followed-up and no cases of
recurrence were observed; the mean follow-up time was 33.20±37.78
months (range, 6–120 months). No intraoperative or postoperative
complications occurred, with the exception of one patient who
experience bladder fistula that occurred the day following the
removal of the catheter due to bladder over-dilation; the patient
recovered quickly after reinserting the catheter.
Discussion
Carcinoma of cervical stump accounts for 3–9% of all
cases of cervical cancer (2,13). Miller et al (4) reported that the symptomatology, stage
distribution and histology of cervical stump cancer were not
significantly different to those of cervical carcinoma of the
intact uterus. The individualization of therapy depends on the
tumor stage, volume and depth of invasion. Although the 5-year
survival rates of patients with cervical stump cancer compare
favorably with patients with intact uteri, the complication rate
appears to be enhanced by previous surgery and palliative care.
Surgery is recommended for patients with pre-invasive disease and
small volume (2 cm) invasive lesions limited to the cervix (stage
IA and IB). In the present study, patients with stage IIA cervical
stump cancer were surgically treated and no complications were
identified.
A review of PubMed revealed that the majority of
current reports are associated with the cornerstone management of
radiation therapy; comparatively few reports are associated with
radio-surgical combination methods. However, severe complications
such as cystitis and rectum fistula have been reported, this is due
to the absence of the uterus which acts as a shield. Of the present
9 cases treated with radical trachelectomy and pelvic
lymphadenectomy (5 with laparoscopic; 4 with laparotomic abdominal
surgery), only one patient experienced the complication of bladder
fistula, and the patient recovered soon after reinserting the
catheter.
Compared with patients with cervical cancer and
intact uteri, the patients with cervical stump cancer were
generally older and typically had concurrent complicating
conditions such as hypertension or diabetes (14–19). The
benefits of preserving the cervix may be associated with the
patient's desire to preserve sexual, bladder and bowel function as
previously reported, an approach that remains controversial among
gynecologists (20–22). It must be noted that regular cervical
screening following a subtotal hysterectomy is essential. Vaginal
bleeding is a severe symptom in non-menstruating female.
As amputation of the radical cervical stump is
considered to be challenging following a supravaginal hysterectomy,
the majority of patients were subjected to concurrent
chemoradiotherapy. Severe rectal, bladder and sigmoid complications
following radiation have been reported due to the loss of
protection offered by the intact uterus. Currently, surgery is the
recommended approach for this type of tumor. With the development
and proficiency of the laparoscopic surgical technique, ever more
complicated laparoscopic surgical techniques have been made
clinically available. This type of surgery has fewer associated
complications, particularly with regard to reduced blood loss and a
shorter recovery time.
In China, patients with malignant tumors often stay
longer in hospital for reasons, including patient requests, age and
physical weakness, compared with patients in developed countries.
Oncologists must be vigilant to the appearance of complications. As
the laparoscopic surgery approach has a number of inherent
advantages, including easier identification of the ureter using
laparoscopic enlargement and less injuries, laparoscopic surgery is
recommended for the treatment of patients with early-stage cervical
stump cancer.
Acknowledgements
The present study was supported by Anhui Provincial
Science and Technology Agency 2013 Year Key Research Projects
(grant no. 1301043053) and the National Natural Science Foundation
of China (grant nos. 81001168 and 81272881). The Anhui Provincial
Key Research and Development Project (grant no. 1704a0802151).
References
|
1
|
Barillot I, Horiot JC, Cuisenier J,
Pigneux J, Schraub S, Rozan R, Pourquier H, Daly N, Vrousos C,
Keiling R, et al: Carcinoma of the cervical stump: A review of 213
cases. Eur J Cancer. 29A:1–1236. 1993.
|
|
2
|
Hellström AC, Sigurjonson T and Pettersson
F: Carcinoma of the cervical stump. The radiumhemmet series
1959–1987. Treatment and prognosis. Acta Obstet Gynecol Scand.
80:152–157. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Diaz-Feijoo B, Gil-Moreno A, Puig O,
Martínez-Palones JM and Xercavins J: Total laparoscopic radical
trachelectomy with intraoperative sentinel node identification for
early cervical stump cancer. J Minim Invasive Gynecol. 12:522–524.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Miller BE, Copeland LJ, Hamberger AD,
Gershenson DM, Saul PB, Herson J and Rutledge FN: Carcinoma of the
cervical stump. Gynecol Oncol. 18:100–108. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nass JM, Brady LW, Glassburn JR and
Prasasvinichai S: The radiotherapeutic management of carcinoma of
the cervical stump. Int J Radiat Oncol Biol Phys. 4:279–281. 1978.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Prempree T, Patanaphan V and Scott RM:
Radiation management of carcinoma of the cervical stump. Cancer.
43:1262–1273. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wolff JP, Lacour J, Chassagne D and Berend
M: Cancer of the cervical stump. Study of 173 patients. Obstet
Gynecol. 39:10–16. 1972.PubMed/NCBI
|
|
8
|
Koh WJ, Greer BE, Abu-Rustum NR, Apte SM,
Campos SM, Cho KR, Chu C, Cohn D, Crispens MA, Dorigo O, et al:
Cervical Cancer, Version 2.2015. J Natl Compr Canc Netw.
13:395–404. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Johnson CJ, Graff R, Moran P, Cariou C and
Bordeaux S: Breast cancer stage, surgery and survival statistics
for Idaho's National Breast and Cervical Cancer Early Detection
Program population, 2004–2012. Prev Chronic Dis. 12:E362015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rose J, Beaulac J, Howlett R and Kan L;
Cervical Cancer Prevention and Control Network, : Cervical cancer
in Canada: A response to the release of the CCS/NCIC Cancer
Statistics 2006. J Obstet Gynaecol Can. 28:678–679. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bray F, Carstensen B, Møller H, Zappa M,
Zakelj MP, Lawrence G, Hakama M and Weiderpass E: Incidence trends
of adenocarcinoma of the cervix in 13 European countries. Cancer
Epidemiol Biomarkers Prev. 14:2191–2199. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bray F, Loos AH, McCarron P, Weiderpass E,
Arbyn M, Møller H, Hakama M and Parkin DM: Trends in cervical
squamous cell carcinoma incidence in 13 European countries:
Changing risk and the effects of screening. Cancer Epidemiol
Biomarkers Prev. 14:677–686. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hannoun-Lévi JM, Peiffert D, Hoffstetter
S, Luporsi E, Bey P and Pernot M: Carcinoma of the cervical stump:
Retrospective analysis of 77 cases. Radiother Oncol. 43:147–153.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Maggi R, Bortolozzi G, Mangioni C, Uderzo
A, Pisani G and Candiani GB: Residual cervical stump cancer (true
cancer) and residual cancer of the cervical stump (coincident
cancer). Casuistics and therapeutic results in the period
1955–1979. Eur J Gynaecol Oncol. 6:92–94. 1985.PubMed/NCBI
|
|
15
|
Hellström AC, Hellman K, Pettersson BF and
Andersson S: Carcinoma of the cervical stump: Fifty years of
experience. Oncol Rep. 25:1651–1654. 2011.PubMed/NCBI
|
|
16
|
Lee CL, Huang KG, Wang CJ, Yen CF and
Soong YK: Radical laparoscopic surgery for carcinoma of the
cervical stump. J Am Assoc Gynecol Laparosc. 7:241–244. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liang Z, Xu H, Chen Y, Li Y, Chang Q and
Shi C: Laparoscopic radical trachelectomy or parametrectomy and
pelvic and para-aortic lymphadenectomy for cervical or vaginal
stump carcinoma: Report of six cases. Int J Gynecol Cancer.
16:1713–1716. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Parkar RB, Hassan MA, Otieno D and Baraza
R: Laparoscopic trachelectomy for cervical stump ‘carcinoma in
situ’. J Gynecol Endosc Surg. 2:58–60. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shah AN and Olah KS: Cervical stump
carcinoma following subtotal hysterectomy. J Obstet Gynaecol.
22:7012002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bey P, Dartois D, Schoumacher P and Pernot
M: Carcinoma of cervical stump. A retrospective study (author's
transl). Bull Cancer. 67:90–92. 1980.PubMed/NCBI
|
|
21
|
Calais G, Leloup R, Chauvet B, Body G,
Lansac J, Bougnoux P and Le Floch O: Carcinoma of the cervical
stump. Retrospective analysis of 43 cases. Bull Cancer.
76:1103–1110. 1989.(In French).
|
|
22
|
Kovalic JJ, Grigsby PW, Perez CA and
Lockett MA: Cervical stump carcinoma. Int J Radiat Oncol Biol Phys.
20:933–938. 1991. View Article : Google Scholar : PubMed/NCBI
|