Introduction
Transarterial chemoembolization (TACE) is a
well-established intervention for the treatment of hepatocellular
carcinoma (HCC). However, TACE has also been associated with a
variety of complications, such as right upper quadrant pain, fever,
elevated liver enzyme levels and hepatic duct ischemia (1). Bronchobiliary fistula (BBF) is commonly
associated with congenital conditions, trauma complications,
hepatic abscesses and biliary tract obstruction, and it is a
potentially serious condition, associated with a high mortality and
morbidity rate (12.2%) (2). We
herein present the case of a patient who developed BBF as a
complication following multiple TACEs for HCC. To the best of our
knowledge, this is the first such case reported in the literature
to date.
Case report
A 71-year-old man with hepatocellular carcinoma
(HCC) presented with a 2-day history of persistent cough and
sudden-onset expectoration of a large amount of greenish sputum. We
was admitted to Li Yang People's Hospital on the 19th of March
2016. The patient reported that the sputum tasted bitter, similar
to regurgitated stomach contents. The patient had undergone left
lobectomy for HCC 11 years prior, and 19 subsequent TACE
procedures. However, the tumor had progressed and compressed the
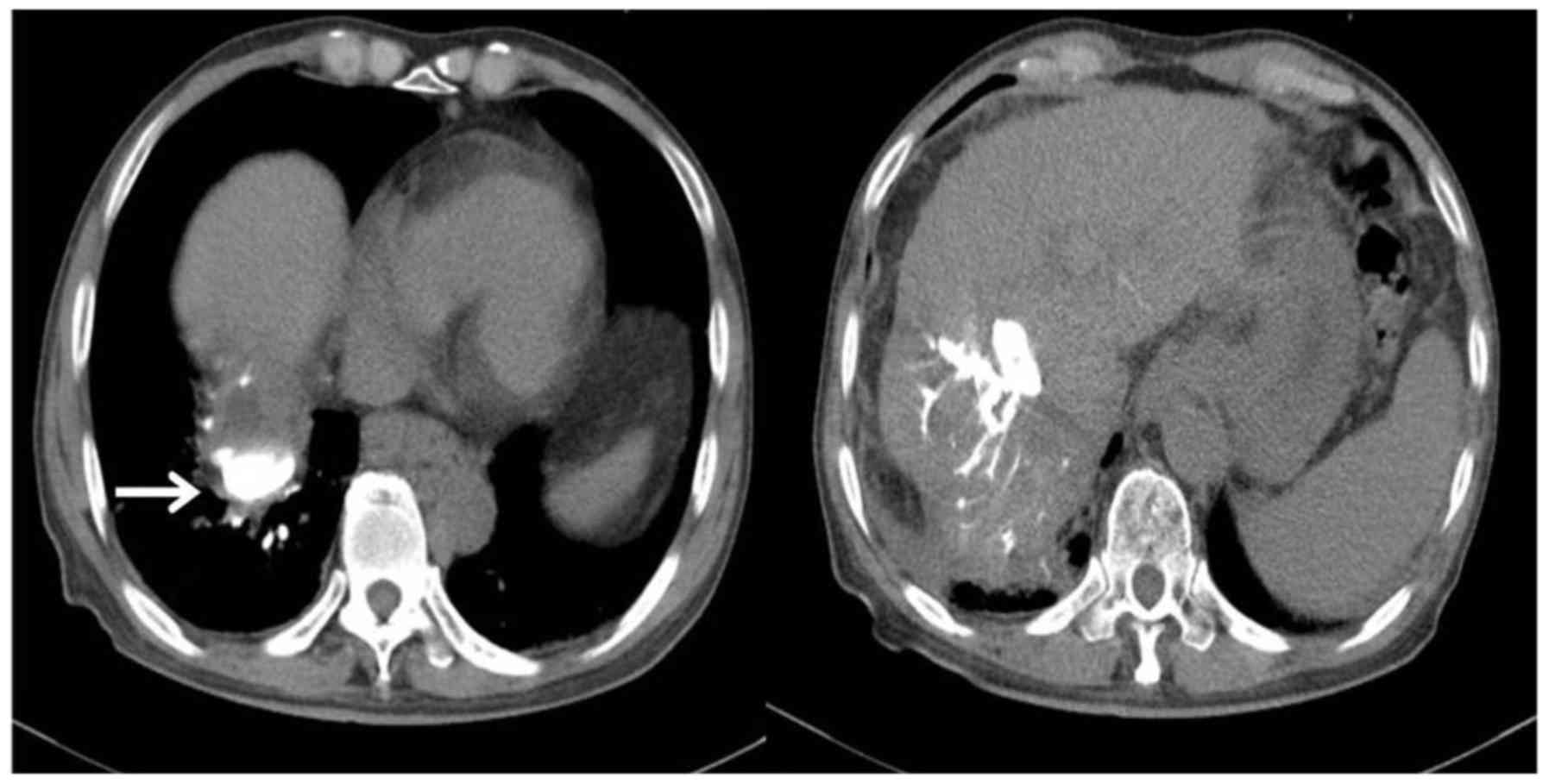
intrahepatic bile duct. A computed tomography (CT) scan of the
abdomen performed at a different institute revealed intrahepatic
bile duct dilatation; endobronchial presence of a high-density
contrast agent in agreement with the density of the intrahepatic
bile ducts further confirmed the presence of a bronchobiliary
shunt. Other findings were unremarkable. The patient was referred
to the Department of Interventional Radiology, First Affiliated
Hospital of Nanjing Medical University (Nanjing, China) for further
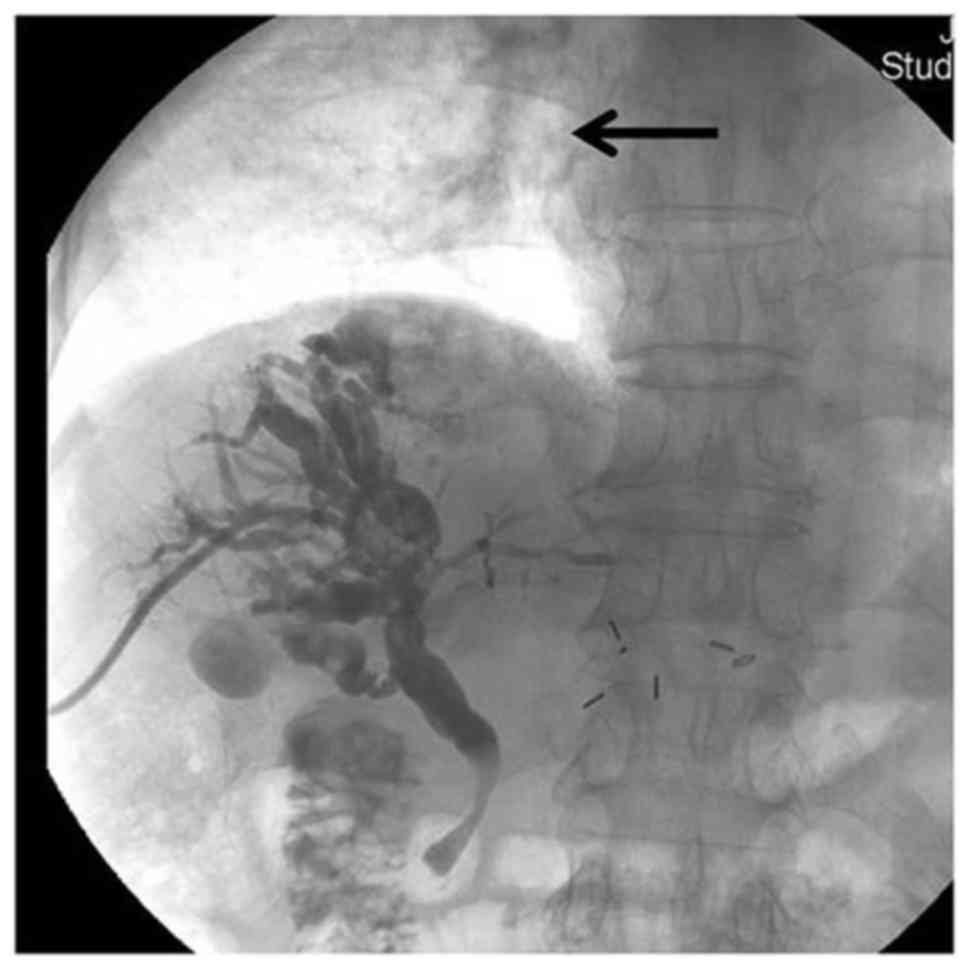
evaluation. Percutaneous transhepatic cholangiography (PTC) was
performed, based on the patient's clinical symptoms and
intrahepatic duct dilation on CT, and revealed focal high-grade
stenosis at the hepatic hilum associated with a severely dilated
biliary tree. An incidental finding of faint contrast material at
the lower lobe of the right lung was also observed during
cholangiography (Fig. 1); this
contrast material was suspected to represent contrast extravasation
from the biliary system to the lung. A follow-up chest CT revealed
contrast material within the bronchial tree of the right lower
lung, a finding consistent with the presence of a bronchobiliary
shunt (Fig. 2).
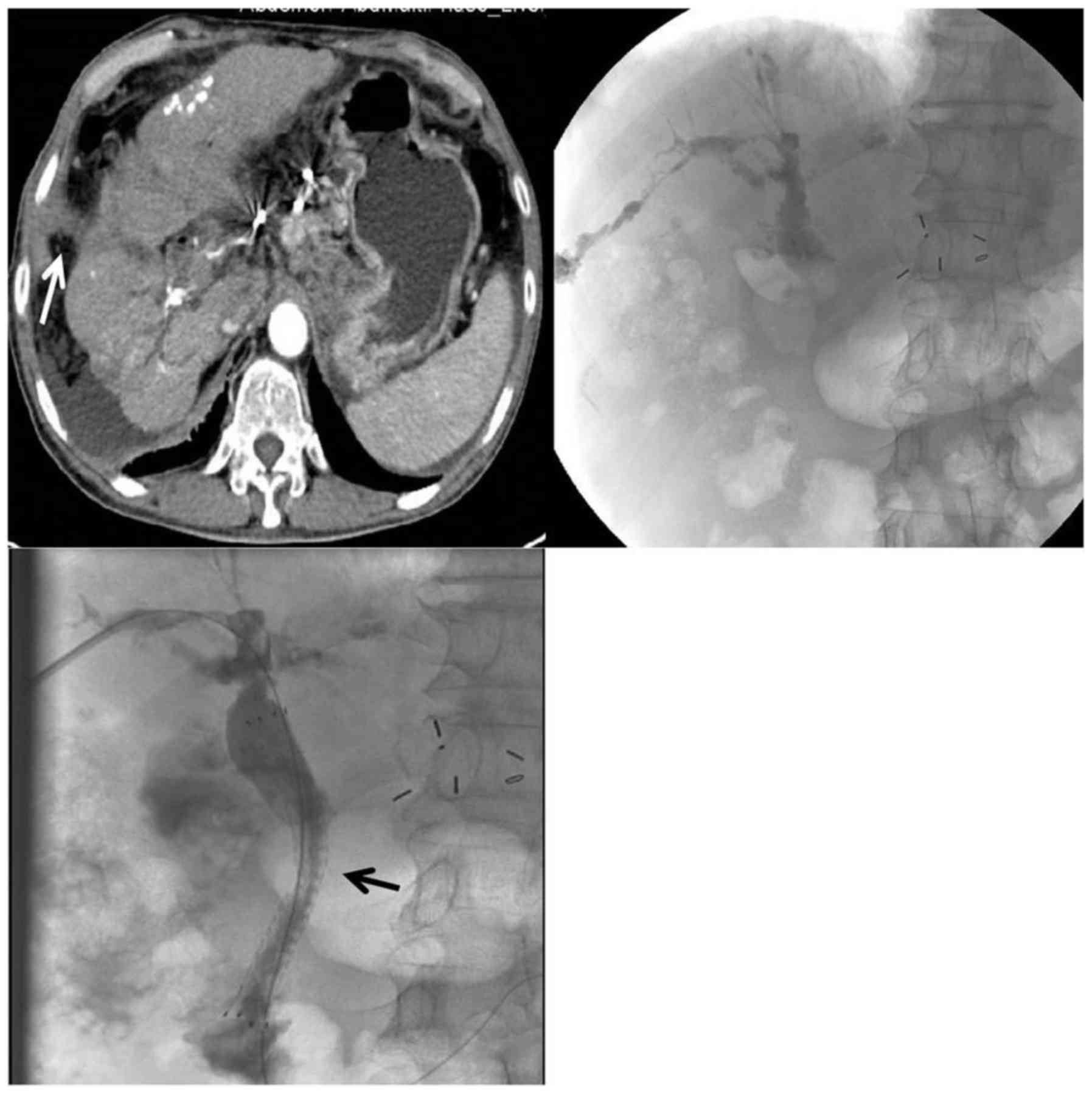
A decision was made to establish percutaneous
transhepatic biliary drainage to decompress the intrahepatic
biliary tree. An 8.5-Fr internal-external biliary drainage tube was
placed, and the patient's cough was relieved on the following day.
The patient was admitted for routine catheter replacement 2 months
later, and cholangiography revealed interval resolution of the
contrast extravasation from the biliary system to the lung. As a
palliative measure, the biliary drain was removed and a metallic
biliary stent (E-Luminex; Bard, Murray Hill, NJ, USA) was placed to
relieve the hilar stenosis (Fig. 3).
The patient remained asymptomatic after the stent placement until
he eventually succumbed to liver failure, infection, and underlying
tumor progression 3 months later.
Discussion
BBF is the formation of an abnormal communication
between the biliary system and the bronchial tree. The mechanism of
BBF remains speculative due to the rarity of this condition. The
most commonly accepted hypothesis is an elevation of the biliary
system pressure, which produces an inflammatory reaction in the
subdiaphragmatic space and subsequent rupture into the bronchial
tree (3,4). Locally aggressive processes, such as
tumor infiltration or abscess rupture through the diaphragm, are
other possible causes of BBF (5).
Warren et al (6) suggested
that two conditions must be met before a BBF occurs in patients
with biliary tract disease: Partial or complete obstruction of the
bile duct, and formation of adhesions between the lung and the
diaphragm. In the present case, the patient had a hilar obstruction
and had undergone multiple TACE treatments, particularly in the
dome area, which may have caused tissue necrosis. Once the
intrabiliary pressure increases, bile may leak from the necrotic
area, rupture through the liver capsule and diaphragm, and
eventually erode into the lung and bronchial tree.
The diagnosis of BBF is straightforward, but a high
level of clinical suspicion is required. The symptoms include an
irritating cough, yellowish sputum and symptoms of acute bronchitis
(7). Sputum analysis should show a
bile component, rather than the typical inflammatory process
characterized by large numbers of bacteria and white cells. PTC and
endoscopic retrograde cholangiopancreatography (ERCP) remain the
procedures of choice to determine the exact anatomy of the fistula
(8). Radiological imaging (thoracic
and upper abdominal CT) may be required to confirm the presence of
contrast material within the bronchial tree after T-tube
cholangiography. Identification of the underlying fistula is useful
to optimize the treatment strategy, which involves either resection
of the fistula or embolization with minimally invasive techniques.
In the present case, the fistula was located in the dome of the
liver and the drainage tube was placed through the right
intrahepatic system, which appeared to adequately decompress the
bile from the hilar obstruction.
The management of BBF may be surgical or
non-surgical (PTC or ERCP), and a well-planned management strategy,
including proper antibiotics and supportive care, is required.
Surgical approach is a definitive treatment, but requires
thoracotomy and/or laparotomy with resection of the fistula and
re-establishment of normal biliary drainage, and such procedures
are often associated with high morbidity (14.3%) and mortality
rates (12.7%) (9). Non-surgical
management includes percutaneous or endoscopic placement of a
biliary drain and/or stent to decompress the intrahepatic biliary
tree by diverting the bile. Such techniques are less invasive and
can provide good results with lower morbidity. Our patient was not
a surgical candidate due to his extensive disease and overall poor
medical condition; therefore, placement of a biliary drain was
considered the treatment of choice. The drain appeared to
effectively decompress the biliary tract pressure with immediate
cessation of the biliptysis. However, we did not further attempt to
close the fistula tract using embolic material or any devices, as
the patient's clinical symptoms had resolved following drain
placement. Thus, decompression of the biliary tract may be the key
to management of BBF in the emergency setting. In the present case,
the patient had undergone multiple (19 times) subsequent TACE
procedures. Such cases are at a high risk of BBF, as after several
TACEs the blood supply of the bile duct may become compromised,
with ensuing high pressure, ischemia and necrosis, leading to BBF
formation.
In conclusion, BBF is an uncommon condition that is
associated with severe mortality and morbidity. Imaging
confirmation of an abnormal communication between the biliary and
bronchial trees is required to establish the diagnosis, and PTC or
ERCP are the most common treatment choices. A CT scan may reveal
the presence of contrast material in the bronchial tree following
cholangiography. The management of BBF may be surgical or
non-surgical, aimed at either permanent resection of the fistula or
palliative decompression of the biliary tree, depending on each
individual case.
Acknowledgements
The authors wish to thank Angela Morben, DVM, ELS,
from Liwen Bianji, Edanz Group China, for editing the English text
of a draft of this manuscript.
Funding
The present study received funding from the Yong
Research Project of First People's Hospital of Changzhou.
Availability of data and materials
Not applicable.
Authors' contributions
CW, ZY made substantial contributions to conception
and design; WC and QW did acquisition of data, analysis and
interpretation of data; CW, JX, WW were involved in drafting the
manuscript and revising it critically for important intellectual
content; CW and ZY gave final approval of the version to be
published. Each author has participated sufficiently in the work to
take public responsibility for appropriate portions of the content;
and agreed to be accountable for all aspects of the work in
ensuring that questions related to the accuracy and integrity of
any part of the work are appropriately investigated and
resolved.
Ethics approval
This article does not contain any studies with human
participants or animals performed by any of the authors.
Consent for publication
The patient and/or his family consented to the
publication of the case details and associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Miyayama S and Matsui O: Superselective
conventional transarterial chemoembolization for hepatocellular
carcinoma: Rationale, technique and outcome. J Vasc Interv Radiol.
27:1269–1278. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Moumen M and El Fares F: Bilio-bronchial
fistula of hydatid origin. Apropos of 8 cases. J Chir (Paris).
128:188–192. 1991.(In French).
|
|
3
|
Singh B, Moodley J, Sheik-Gafoor MH,
Dhooma N and Reddi A: Conservative management of thoracobiliary
fistula. Ann Thorac Surg. 73:1088–1091. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ferguson TB and Burford TH: Pleurobiliary
and bronchobiliary fistulas. Surgical management. Arch Surg.
95:380–386. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim YS, Rhim H, Sung JH, Kim SK, Kim Y,
Koh BH, Cho OK and Kwon SJ: Bronchobiliary fistula after
radiofrequency thermal ablation of hepatic tumor. J Vasc Interv
Radiol. 16:407–410. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Warren KW, Christophi C, Armendariz R and
Basu S: Surgical treatment of bronchobiliary fistulas. Surg Gynecol
Obstet. 157:351–356. 1983.PubMed/NCBI
|
|
7
|
Gugenheim J, Ciardullo M, Traynor O and
Bismuth H: Bronchobiliary fistulas in adults. Ann Surg. 207:90–94.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rose DM, Rose AT, Chapman WC, Wright JK,
Lopez RR and Pinson CW: Management of bronchobiliary fistula as a
late complication of hepatic resection. Am Surg. 64:873–876.
1998.PubMed/NCBI
|
|
9
|
Kabiri H, Chafik A, Al Aziz S, El Maslout
A and Benosman A: Treatment of hydatid bilio-bronchial and
bilio-pleuro-bronchial fistulas by thoracotomy. Ann Chir.
125:654–659. 2000.(In French). View Article : Google Scholar : PubMed/NCBI
|