Introduction
Cholestatic jaundice associated with malignancy
typically occurs as a result of obstruction of the bile ducts or
widespread liver metastases. Reversible cholestasis without
evidence of biliary obstruction has been reported to occur in
association with a variety of malignancies, most notably Stauffer's
Syndrome in renal cell carcinoma. Intrahepatic cholestasis
occurring in the setting of advanced prostate adenocarcinoma has
less commonly been described with the first case reported in 1977
(1). Furthermore, the pathogenesis
of this syndrome remains poorly understood. We present a case of
patient with newly diagnosed metastatic prostate adenocarcinoma
associated with severe liver failure secondary to intrahepatic
cholestasis.
Case report
A 67 year old man with no significant past medical
history presented to his primary care physician with several weeks
of progressive jaundice, pruritus, dark urine, and unintentional
weight loss. Laboratory workup revealed AST of 216 U/l (normal,
15–37), ALT 234 U/l (normal, 16–63), Alkaline phosphatase 988 U/l
(normal 38–126), and total bilirubin of 26.3 mg/dl (0.1–1.2) with
direct bilirubin of 22.5 (0.0–0.3).
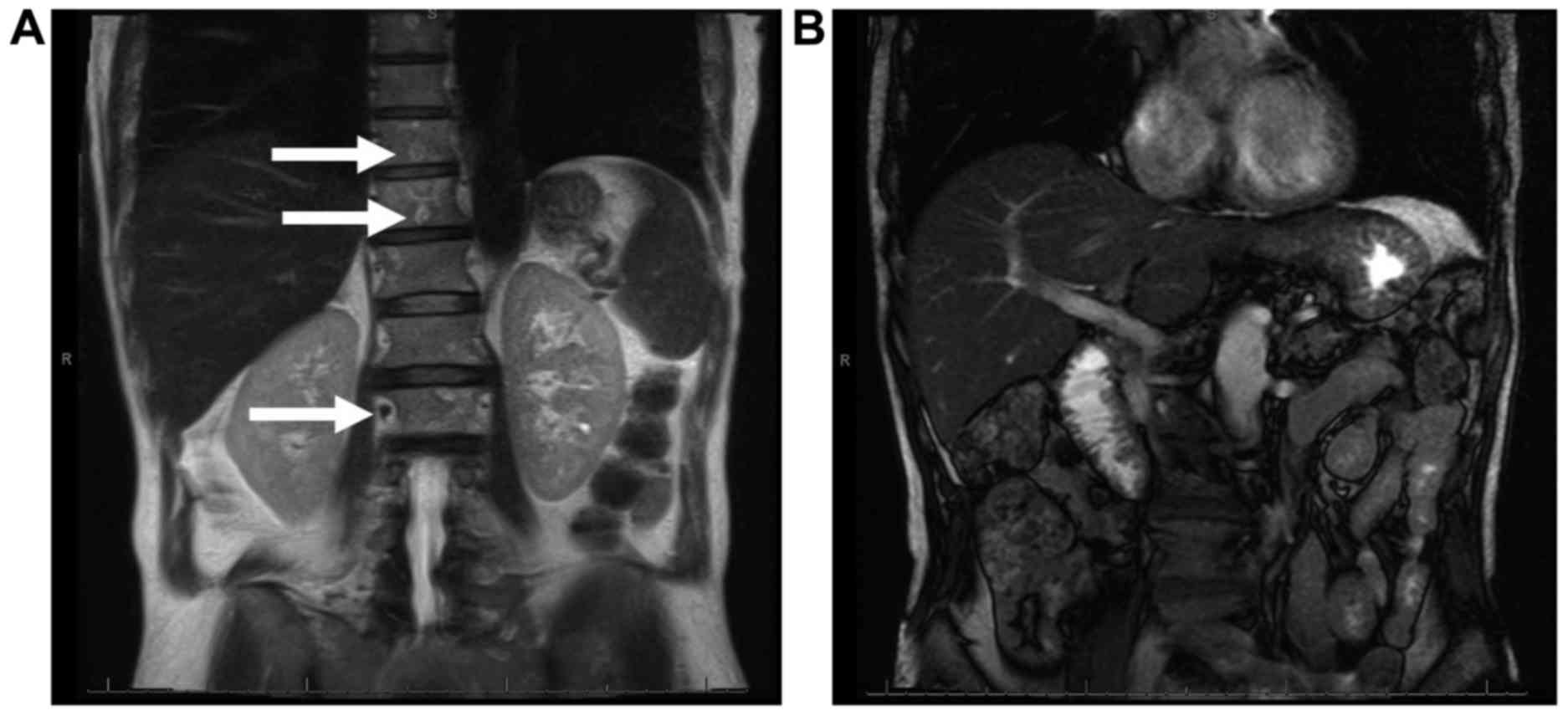
Given these abnormalities a magnetic resonance
imaging (MRI)-cholangiopancreatography (MRCP) of the abdomen
(Fig. 1) was ordered which revealed
a normal liver without any evidence biliary obstruction. Several
lytic lesions of the bone were incidentally discovered concerning
for metastatic disease. Given the unexplained osseous
abnormalities, a PSA was ordered which was significantly elevated
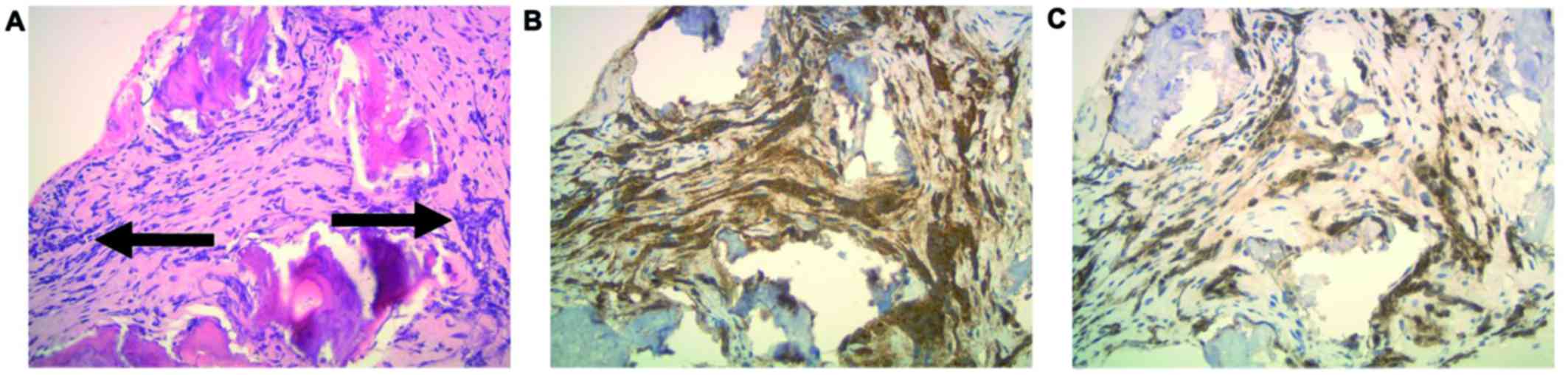
at 4,130 ng/ml (normal 0–4.5). CT-guided core needle biopsy of one
of the bony lesions confirmed metastatic adenocarcinoma strongly
positive for PSA and NKX3.1 (Fig.
2). The clinical presentation, laboratory abnormalities, and
pathology findings were consistent with metastatic prostate
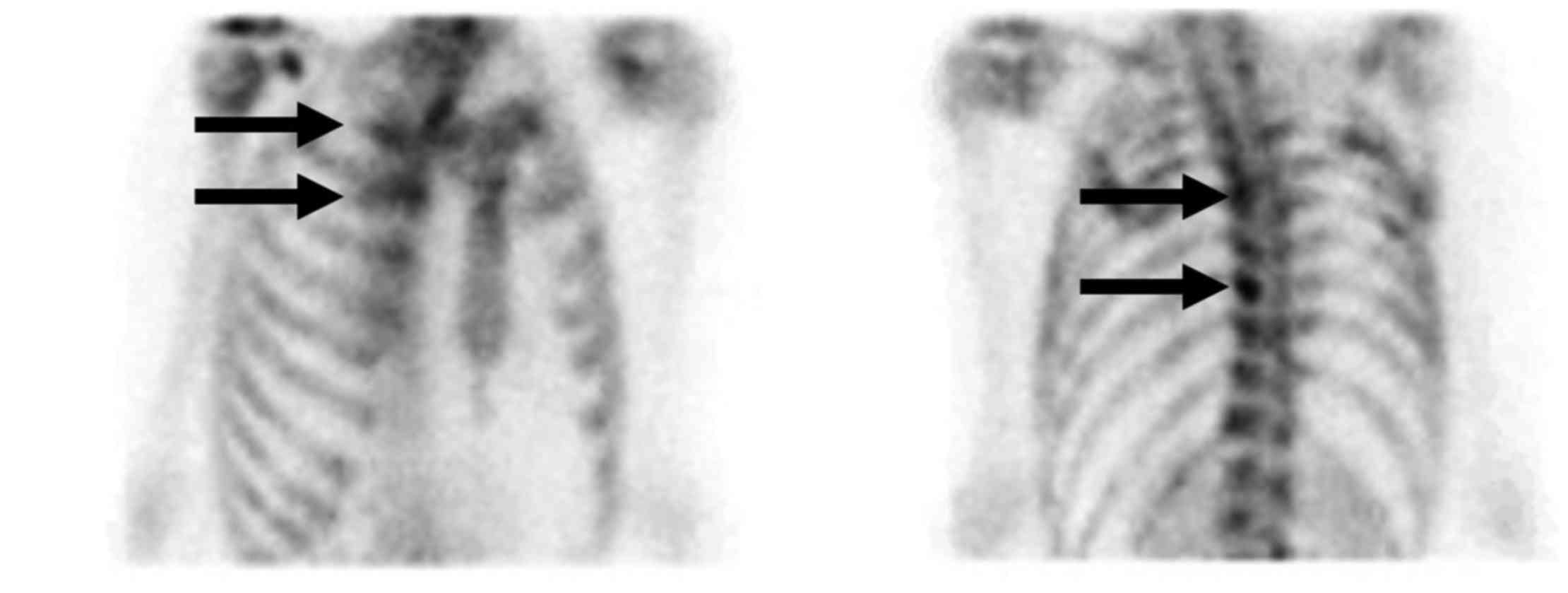
carcinoma. Bone scan (Fig. 3)
confirmed the presence of widespread osseous metastatic
disease.
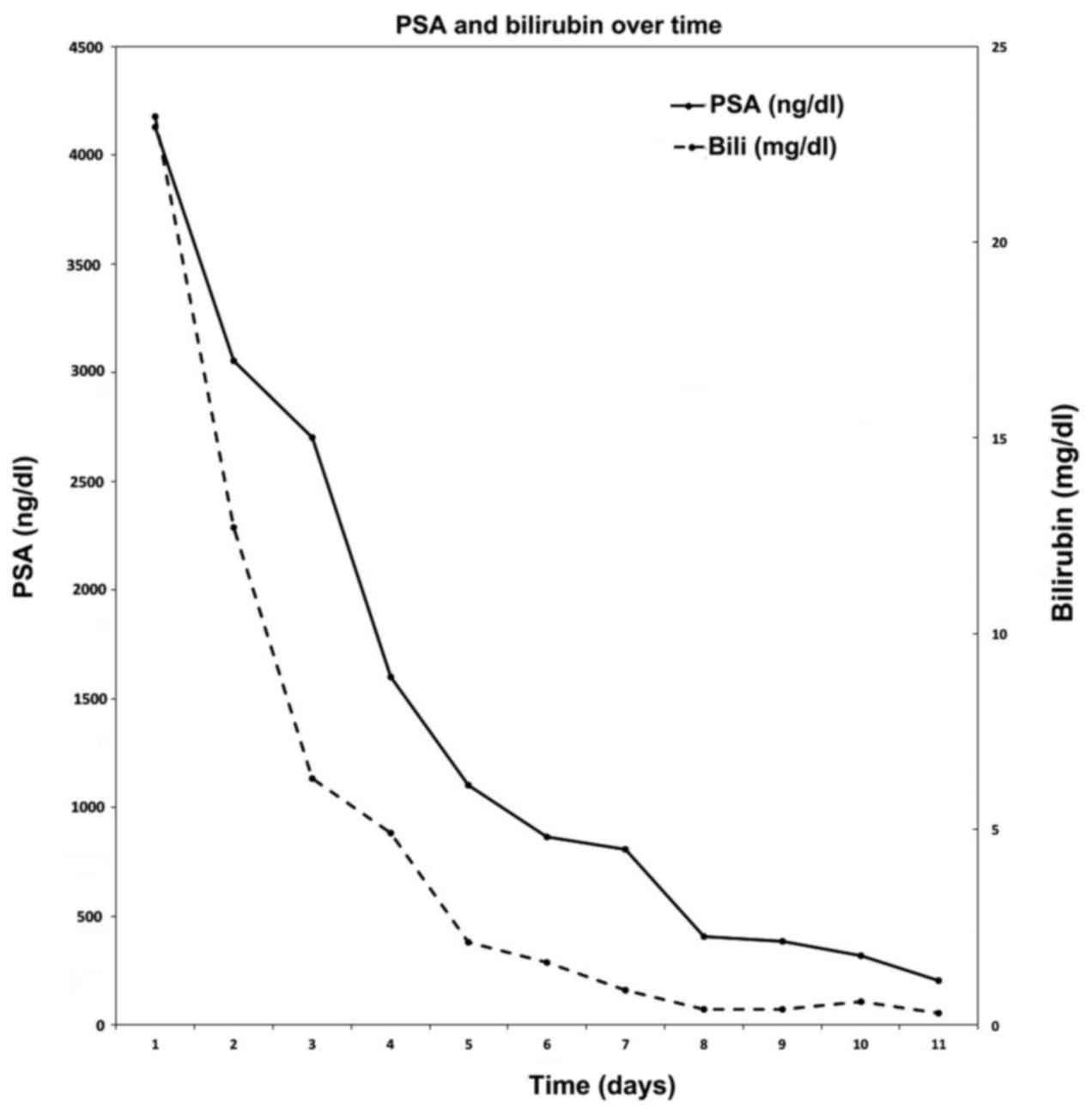
The patient was started on combined androgen
deprivation therapy with LupronDepot (Leuprolide acetate for depot
suspension, AbbVie Inc., North Chicago, IL, USA) 22.5 mg
subcutaneously once every three months and Casodex (Bicalutamide,
Wilmington, DE, USA) 50 mg orally once daily. The patient
clinically responded rapidly soon after initiation of therapy. His
PSA declined to 863 ng/ml four weeks after therapy initiation and
subsequently 408 ng/ml by eight weeks (Fig. 4). Conjugated bilirubin and liver
function abnormalities normalized completely after four weeks of
androgen deprivation. The patient is maintained on depo-leuprolide
therapy six months after diagnosis and remains asymptomatic from
the standpoint of his cancer. Informed consent for this report was
obtained from the patient.
Discussion
Cholestasis in the setting of malignancy occurs from
a variety of mechanisms including external compression of the
biliary system, widespread hepatic infiltration, or metastatic
disease. Less commonly, reversible cholestasis in the absence of
biliary obstruction has been well-described as a paraneoplastic
syndrome. In this case, the possibility of extrinsic compression
causing cholestasis was excluded by multiple imaging techniques
(ultrasound, CT scan, as well as MRI/MRCP). Furthermore, systemic
conditions causing intrahepatic cholestasis such drug toxicity,
infections (viral hepatitis, HIV), primary biliary cirrhosis,
primary sclerosing cholangitis were entertained. These
possibilities were excluded by a careful clinical history and broad
laboratory workup. Given the incidental finding of diffuse osseous
metastasis that was confirmed to be prostate adenocarcinoma on
biopsy, patient was started on anti-androgen therapy and GnRH
agonist for treatment. Ultimately, the temporal association between
the treatment of prostate cancer and resolution of the patient's
liver dysfunction argues strongly for a diagnosis of a
paraneoplastic syndrome.
Paraneoplastic syndromes constitute a heterogeneous
group of disorders that occur as a result of malignancy independent
of mass effect or direct invasion (2). These disorders are felt to occur as a
result of humoral factors (e.g., cytokines or hormones) elaborated
by tumors. An additional mechanism involves activation of the
immune system against tumor antigens (3).
The first report of paraneoplastic liver dysfunction
associated with malignancy was described in association with renal
cell carcinoma (4). This syndrome is
characterized by elevated LFTs in a cholestatic pattern in the
absence of external compression or widespread liver metastases.
Liver pathology review may range from normal histologic findings to
varying degrees of reactive hepatitis (5).
Paraneoplastic intrahepatic cholestasis has been
described in several other malignancies including soft tissue
sarcoma, medullary thyroid cancer, renal sarcoma, T-cell lymphoma,
chronic lymphocytic leukemia, Hodgkin's disease (6–12).
Although uncommon, reversible hepatic dysfunction in prostate
cancer has been described in nine published cases (Table I) (1,13–20). All
reported cases occurred in patients with metastatic disease.
Including the patient reported here, 90% of patients experienced
improvement in liver dysfunction and jaundice with treatment of the
prostate cancer. Patients presenting with intrahepatic cholestasis
appear to do as well as other patients diagnosed with metastatic
prostate cancer. In fact, 70% of reported cases presenting with
intrahepatic cholestasis were alive at one year compared with 71%
of patients diagnosed with metastatic prostate adenocarcinoma per
SEER analysis (21). This suggests
that hepatic dysfunction as a presenting sign may not necessarily
be a poor prognostic feature.
 | Table I.Cases reviewed from literature
detailing cholestasis reversal with prostate cancer treatment. Ten
cases were analyzed from the literature and compared in terms of
patient clinical characteristics, laboratory data, and outcome over
a 42 year period of time. |
Table I.
Cases reviewed from literature
detailing cholestasis reversal with prostate cancer treatment. Ten
cases were analyzed from the literature and compared in terms of
patient clinical characteristics, laboratory data, and outcome over
a 42 year period of time.
| First author | Age | Stage | PSA (ng/ml) | Total bilirubin
(mg/dl) | Management | Liver function test
outcome | Clinical followup
(Mos.) | (Refs.) |
|---|
| Bhangoo, 2017 | 67 | Metastatic | 4,130 | 26.3 | Leuprolide,
bicalutamide | Improved | Remission (6) | Present study |
| Reddy, 1977 | 57 | Metastatic |
| 6.2 | Radiation,
diethylstilbestrol | Transiently
improved | Deceased (32) | (1) |
| Karakolios 2003 | 72 | Metastatic | 150 | 18.1 | Flutamide,
leuprolide | Resolved | Remission (9) | (13) |
| Bloch, 1992 | 69 | Metastatic |
| 10.6 | ADT, bilateral
orchiectomy | Resolved | Deceased (48) | (14) |
| Cole, 2000 | 78 | Metastatic | 9,996 | 6.56 | Leuprolide,
bicalutamide | Resolved | Remission (3) | (15) |
| Nguyen, 2011 | 51 | Metastatic | 556 | 19 | Goserelin,
bicalutamide | Improved | Remission (6) | (16) |
| Kuramoto, 2013 | 75 | Metastatic | 9,862 | 17 | Leuprolide,
bicalutamide | Resolved | Remission (12) | (17) |
| Ben-Ishay, 1975 | 58 | Metastatic |
| 13 | Stilbestrol,
bilateral orchiectomy | Resolved | Remission (24) | (18) |
| Koruk, 2004 | 77 | Metastatic | 100 | 10 | Goserelin,
bicalutamide | Resolved | Remission (6) | (19) |
| Shah, 2006 | 64 | Metastatic | 956 | 132 | Goserelin,
cyproterone | No response | Deceased (6) | (20) |
The precise mechanism of disease is not well
understood. One putative explanation involves interleukin 6 (IL-6)
which appears to be involved in paraneoplastic cholestasis
associated with renal cell carcinoma. In a study of 119 patient
with metastatic renal cell carcinoma, patients with intrahepatic
cholestasis were found to have significantly elevated IL-6 levels
compared with patients without this syndrome (22). The association of IL-6 and
cholestasis may be mediated by a systemic inflammation as
laboratory markers including C-reactive protein (CRP) and
haptoglobin which are commonly elevated (22). Pro-inflammatory cytokines inhibit
expression of the hepatobiliary transporter gene expression
possibly accounting for impaired biliary outflow (23). The association of this condition with
IL-6 remains speculative and other humoral mediators have also been
proposed (18). Increased levels of
IL-6 have similarly been reported among prostate cancer patients
with liver dysfunction suggesting a potential association in this
paraneoplastic syndrome (16,17).
Future directions to elucidate the molecular mechanisms driving
this paraneoplastic syndrome includes cytokine profiling of serum
from affected patients. Whether or not increased levels of IL-6
correlate with liver dysfunction in prostate cancer is unknown and
warrants further investigation.
The case described above is one of few documented
cases where cholestasis occurred as a result of paraneoplastic
syndrome from prostate cancer without evidence of hepatic
infiltration, metastatic disease, or tumor compression. Our
patient's cholestasis resolved with the treatment of his prostate
cancer, which is consistent clinical feature of this disease.
References
|
1
|
Reddy A, Grosberg SJ and Wpanick S:
Intermittent cholestatic jaundice and nonmetastatic prostatic
carcinoma. Arch Intern Med. 137:1616–1618. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Darnell RB and Posner JB: Paraneoplastic
syndromes. Oxford Uni Press; pp. 4822011
|
|
3
|
Pelosof LC and Gerber DE: Paraneoplastic
syndromes: An approach to diagnosis and treatment. Mayo Clin Proc.
85:pp. 838–854. 2010; View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Stauffer M: Nephrogenic hepatomegaly.
Gastroenterol. 40:6941961.
|
|
5
|
Dancygier H: Clinical hepatology:
Principles and practice of hepatobiliary diseases. 2. Springer;
2010, View Article : Google Scholar
|
|
6
|
Perisic VN, Howard ER, Mihailovic T,
Vujanic G, Milovanovic D and Ivanovski P: Cholestasis caused by
biliary botryoid sarcoma. Eur J Pediatr Surg. 1:242–243. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tiede DJ, Tefferi A, Kochhar R, Thompson
GB and Hay ID: Paraneoplastic cholestasis and hypercoagulability
associated with medullary thyroid carcinoma. Resolution with tumor
debulking. Cancer. 73:702–705. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Patel KJ, Latif SU and de Calaca WM: An
unusual presentation of precursor T cell lymphoblastic
leukemia/lymphoma with cholestatic jaundice: Case report. J Hematol
Oncol. 2:122009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Alirhayim Z, Dyal H, Alarhayem A and
Donthireddy V: Non-Hodgkin's lymphoma: A cause of paraneoplastic
cholestasis. BMJ Case Rep. 2013(pii): bcr20130097142013.PubMed/NCBI
|
|
10
|
Fraisse TC, Damigny A, di Castri A, de
Wazières B and Fourcade J: Leiomyosarcoma and Stauffer syndrome.
Rev Med Interne. 22:1116–1118. 2001.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Barta SK, Yahalom J, Shia J and Hamlin PA:
Idiopathic cholestasis as a paraneoplastic phenomenon in Hodgkin's
lymphoma. Clin Lymphoma Myeloma. 7:77–82. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pandey J and Bhowmik KT: Chronic
lymphocytic leukemia presenting as jaundice. Indian J
Gastroenterol. 17:281998.PubMed/NCBI
|
|
13
|
Karakolios A, Kasapis C, Kallinikidis T,
Kalpidis P and Grigoriadis N: Cholestatic jaundice as a
paraneoplastic manifestation of prostate adenocarcinoma. Clin
Gastroenterol Hepatol. 1:480–483. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bloch WE and Block NL: Metastatic prostate
cancer presenting as obstructive jaundice. Urology. 40:456–457.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cole A, Mendelblatt D, Aguayo J, Mathew A,
Martin E and Vesely DL: Metastatic prostate cancer (with
prostate-specific antigen of 9996) presenting as obstructive
jaundice. Am J Med Sci. 319:118–122. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nguyen V, Gurney H and van der Poorten D:
Paraneoplastic hepatic dysfunction in metastatic prostate cancer:
The role of cytokine dysregulation. J Clin Oncol. 29:e21–e23. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kuramoto T, Senzaki H, Koike H, Yamagiwa
K, Tamura S, Fujimoto T and Inagaki T: Cholestatic jaundice as a
paraneoplastic manifestation of prostate cancer. Case Rep Urol.
2013:3037272013.PubMed/NCBI
|
|
18
|
Ben-Ishay D, Slavin S, Levij IS and
Eliakim M: Obstructive jaundice associated with carcinoma of the
prostate. Isr J Med Sci. 11:838–844. 1975.PubMed/NCBI
|
|
19
|
Koruk M, Büyükberber M, Savaş C and
Kadayifçi A: Paraneoplastic cholestasis associated with prostate
carcinoma. Turkish J Gastroenterol. 15:53–55. 2004.
|
|
20
|
Shah SH: Paraneoplastic liver dysfunction
in prostate cancer. J Pain Symptom Manage. 32:511–513. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
National Cancer Institute, . Cancer of the
prostate-SEER stat fact sheets. 2016.
|
|
22
|
Blay JY, Rossi JF, Wijdenes J,
Menetrier-Caux C, Schemann S, Négrier S, Philip T and Favrot M:
Role of interleukin-6 in the paraneoplastic inflammatory syndrome
associated with renal-cell carcinoma. Int J Cancer. 72:424–430.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Trauner M, Fickert P and Stauber RE:
Inflammation-induced cholestasis. J Gastroenterol Hepatol.
14:946–959. 1999. View Article : Google Scholar : PubMed/NCBI
|