Introduction
The clinical and descriptive term ‘leukoplakia’
denotes a white patch on a mucosal surface identified on
macroscopic examination. The underlying pathology includes various
lesions, such as squamous hyperplasia with or without keratosis,
epithelial dysplasia of various grades of severity, carcinoma in
situ (CIS) or invasive carcinoma. Therefore, biopsy and
histological examination are warranted to obtain a definitive
diagnosis (1,2). The most important etiological factors
for the development of laryngeal precancerous lesions, as well as
malignant transformation to invasive carcinoma, are tobacco and
alcohol abuse. In recent years, gastroesophageal reflux has also
been considered to play a causative role (3). Other possible etiological factors are
occupational hazards (e.g., asbestos), nutritional deficiencies,
vocal abuse, chronic infections and hormonal disorders (4,5).
The association of vocal cord leukoplakia with
laryngeal carcinoma has been the subject of numerous clinical
studies and meta-analyses over the past decades, which have been
mainly based on data from hospitals (3,6,7). The rates of carcinoma underlying
leukoplakia at first diagnosis and the secondary malignant
transformation rates in the later course of the disease vary widely
between studies, which is due to a marked sampling or case
selection bias of hospital-based studies when compared with the
general population, selecting more severe cases and higher
transformation rates in specialized centers (6). The only population-based study on vocal
cord leukoplakia and laryngeal cancer with supposedly less biased
data included a limited number of cases, only 108 over a period of
49 years (8). Current data from the
German healthcare system on vocal cord leukoplakia and its
association with laryngeal cancer have yet to be published.
The status of otorhinolaryngology practices in
particular, with their role as first diagnostic gatekeepers, has
yet to be examined. Thus, the aim of the present study was to
investigate the current epidemiological status of vocal cord
leukoplakia and its association with laryngeal cancer in
otorhinolaryngology practices in Germany, based on data from a
large and representative nationwide practice database.
Materials and methods
Database
The Disease Analyzer database (QuintilesIMS,
Frankfurt, Germany) compiles drug prescriptions, diagnoses, and
basic medical and demographic data obtained directly and in
anonymous format from computer systems used in physicians'
practices (9). Diagnoses (ICD-10),
prescriptions [Anatomical Therapeutic Chemical (ATC) Classification
System], and the quality of reported data are monitored by
QuintilesIMS based on a number of criteria, such as completeness of
documentation and association between diagnoses and prescriptions,
among others.
In Germany, the sampling methods used for the
selection of physicians' practices were considered appropriate for
obtaining a representative database of such practices (9). The sampling method for the Disease
Analyzer database is based on summary statistics from all
physicians in Germany published yearly by the German Medical
Association. IMS uses these statistics to determine the panel
design according to specialist group, German federal state,
community size category, and age of the physician. This panel
design forms the basis for the selection of practices included in
the Disease Analyzer. The sampling plan is subdivided into 8
geographical regions, which are groupings of the 16 German federal
states. This stratification results in 176 cells, derived from the
summary statistics for the specialist fields, and is proportional
to the summary statistics for the German federal states. Within
each region and specialist field, a minimum of 7 physicians must be
sampled to allow for estimates for each region at the specialist
field level. The database has already been used in several studies
focusing on cancer (10–12).
Study population
The study sample included patients aged 18–90 years,
from 113 otorhinolaryngology practices, who were diagnosed with
vocal cord leukoplakia (ICD-10: J38.3, plus an original note by the
physician containing the term ‘leukoplakia’) between January 2007
and December 2014 (index date). Patients were followed up for a
maximum of 5 years. In order to guarantee the accuracy of the
estimation of the progression of leukoplakia to laryngeal cancer,
patients with a documented diagnosis of cancer (C00-C99) prior to
the index date were excluded.
Study outcome and independent
variables
The primary outcome measure was the rate of patients
with a confirmed diagnosis of malignant neoplasm of the larynx,
including malignant neoplasm of the glottis (C32.0), malignant
neoplasm of overlapping sites of the larynx (C32.8) and unspecified
malignant neoplasm of the larynx (C32.9). Malignant neoplasms of
the supraglottis (C32.1), subglottis (C32.2) and laryngeal
cartilage (C32.3) were excluded. Independent variables included age
and sex.
Statistical analysis
Descriptive analyses were obtained for all variables
and mean ± standard deviation (SD) was calculated for normally
distributed variables. Kaplan-Meier curves were used to analyze the
percentage of patients who developed laryngeal cancer over time in
the different sex and age groups. Finally, multivariate Cox
regression models (dependent variable, incidence of cancer
diagnosis) were used to determine laryngeal cancer risk when
adjusting for age and sex. P-values<0.05 were considered to
indicate statistically significant differences. Analyses were
performed using SAS software, version 9.4 (SAS Institute, Inc.,
Cary, NC, USA).
Results
Patient characteristics
Socio-demographic data pertaining to the individuals
included in the present study are shown in Table I. A total of 1,184 patients in 113
practices were available for analysis. The mean age was 58.2 years
(SD, 14.0 years), and 61.8% of patients were men.
 | Table I.Characteristics of patients with an
initial diagnosis of vocal cord leukoplakia (n=1,184) included in
the present study (QuintilesIMS Disease Analyzer database). |
Table I.
Characteristics of patients with an
initial diagnosis of vocal cord leukoplakia (n=1,184) included in
the present study (QuintilesIMS Disease Analyzer database).
| Demographic
characteristics | No. (%) |
|---|
| Age (years), mean ±
standard deviation | 58.2 (14.0) |
|
<50 | 346 (29.2) |
|
<50–65 | 462 (39.0) |
| >65 | 376 (31.8) |
| Sex |
|
|
Female | 452 (38.2) |
| Male | 732 (61.8) |
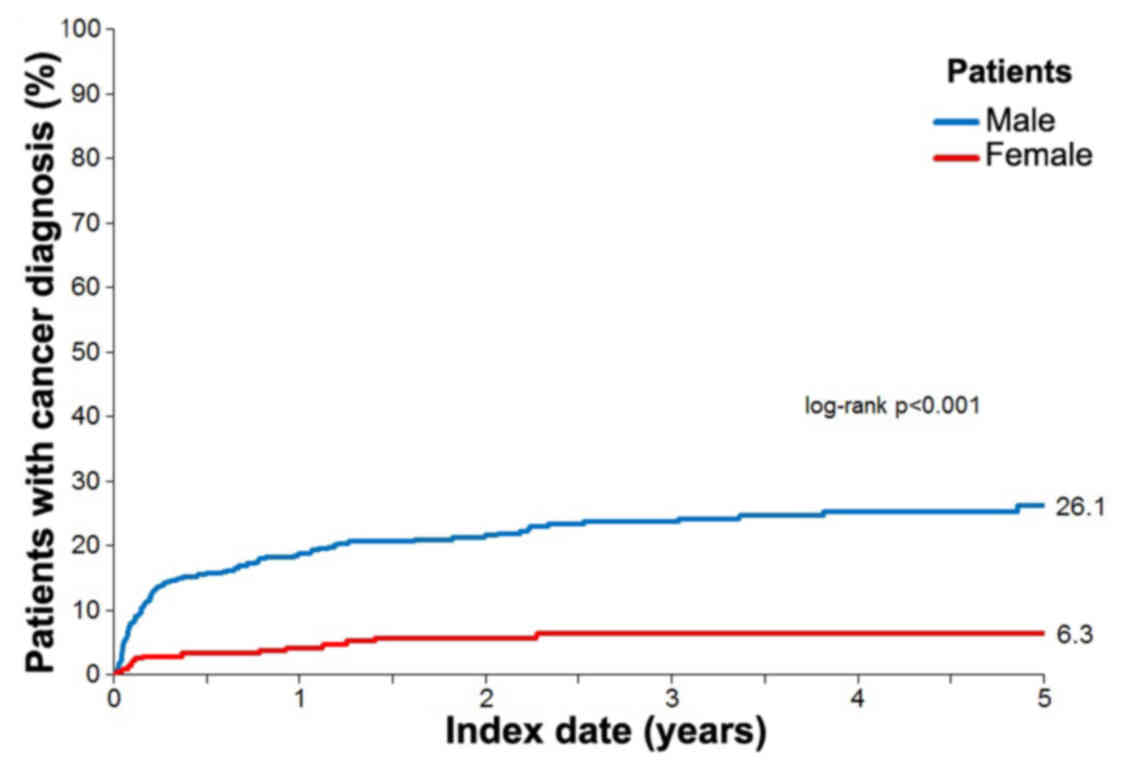
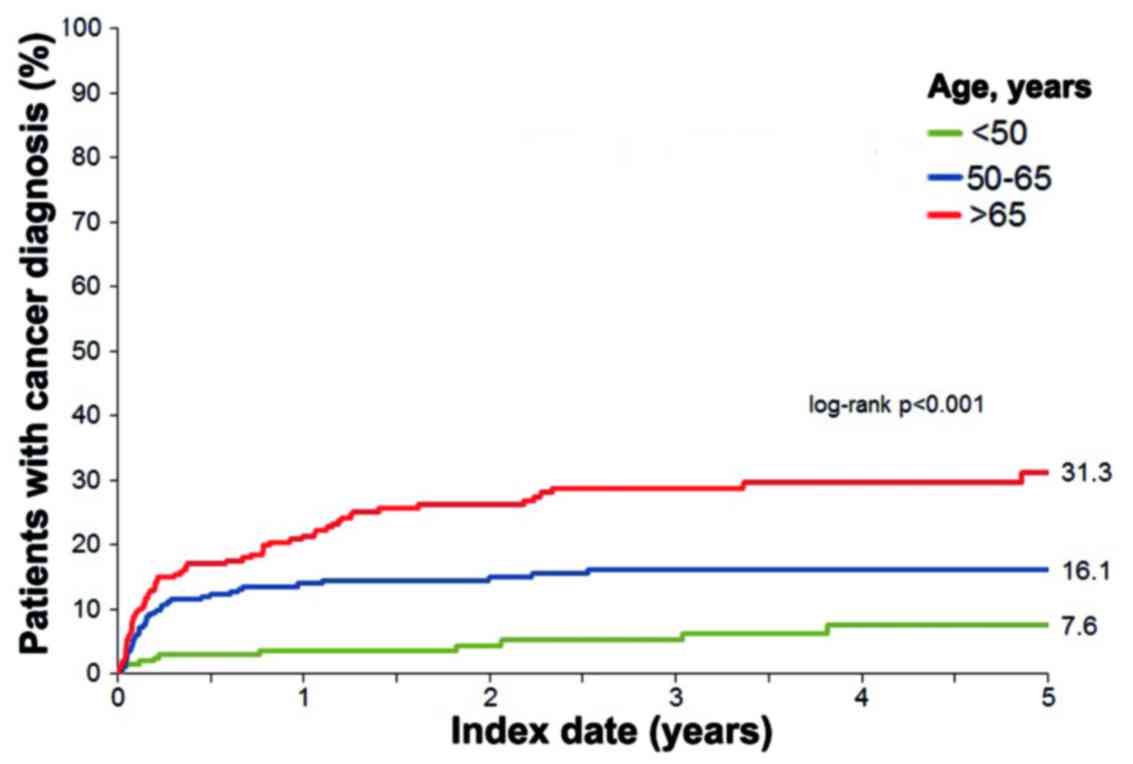
Laryngeal cancer diagnosis by age and
sex
Kaplan-Meier curves for the diagnosis of laryngeal
cancer are shown in Figs. 1 and
2. Within 6 months of initial
diagnosis of vocal cord leukoplakia, 11% of the patients were
diagnosed with laryngeal cancer. Between 7 months and 5 years after
leukoplakia diagnosis, laryngeal cancer was diagnosed in 7.6% of
the patients. Overall, within 5 years of leukoplakia diagnosis,
18.6% of the patients were diagnosed with laryngeal cancer (26.1%
of men and 6.3% of women; log-rank P-value<0.001, Fig. 1). Moreover, 31.3% of individuals aged
>65 years, 16.1% of individuals aged 50–65 years, and 7.6% of
individuals aged<50 years were diagnosed with laryngeal cancer
(log-rank P-value<0.001, Fig. 2).
Similar trends were observed for the three different age groups
among men (38.4, 21.7 and 14.7%, respectively; log-rank
P-value<0.001) and women (14.5, 4.4 and 0.9%, respectively;
log-rank P-value<0.003).
Among patients who developed laryngeal cancer, 46.6%
were diagnosed with malignant neoplasm of the glottis (ICD-10:
C32.0), 1.5% with malignant neoplasm of overlapping sites of the
larynx (ICD-10: C32.8), and 51.9% with unspecified malignant
neoplasm of the larynx (C32.9). The results of the Cox regression
model are presented in Table II.
Patients aged >65 and those aged 50–65 years were at a higher
risk of being diagnosed with laryngeal cancer (OR=4.90 and 2.55,
respectively). Furthermore, the risk of developing laryngeal cancer
was higher in men compared with that in women (OR=4.09).
 | Table II.Multivariate Cox regression model for
the risk of laryngeal cancer diagnosis in patients with an initial
diagnosis of vocal cord leukoplakia. |
Table II.
Multivariate Cox regression model for
the risk of laryngeal cancer diagnosis in patients with an initial
diagnosis of vocal cord leukoplakia.
|
Variablesa | OR (95%
CI)a | P-valuea |
|---|
| 50–65 vs. <50
years | 2.55 (1.36–4.82) | 0.001 |
| >65 vs. <50
years | 4.90 (2.66–9.03) | <0.001 |
| Male vs. female | 4.09 (2.42–6.90) | <0.001 |
Discussion
Using data from a large nationwide practice
database, the present study analyzed the association of laryngeal
cancer with vocal cord leukoplakia in 1,184 patients from 113
otorhinolaryngology practices in Germany. Within 6 months of
initial diagnosis of vocal cord leukoplakia, 11.0% of the patients
were diagnosed with laryngeal cancer, while between 7 months and 5
years after initial leukoplakia diagnosis, 7.6% of the patients
were diagnosed with laryngeal cancer. Male sex and older age were
found to be risk factors for the diagnosis of laryngeal cancer in
these patients.
The association between laryngeal leukoplakia and
cancer has been the subject of numerous clinical studies and
meta-analyses in recent decades. The terminology and classification
of this spectrum of lesions has changed markedly over time. While
in early studies the term ‘keratosis’ was used as a clinical term
interchangeably with leukoplakia (6), in current terminology ‘keratosis’ is
strictly reserved for a histological finding of a keratin layer on
squamous epithelium (3). Moreover,
the histological spectrum of laryngeal precancerous lesions
underlying the clinical finding of vocal cord leukoplakia has been
classified using a variety of grading systems over the years. Early
classifications subdivided histology into keratosis without atypia
(KWOA) vs. keratosis with atypia (KWA), or into grades I, II and
III according to Kleinsasser (hyperplasia without atypia,
hyperplasia with atypia and CIS, respectively) (13–17).
Other histological grading systems, such as those for squamous
intraepithelial neoplasia (SIN) or laryngeal intraepithelial
neoplasia (LIN), were subsequently developed (18,19). The
most frequently used classifications today are the SIN system, the
Ljubljana classification of squamous intraepithelial lesions (SIL)
and, particularly, the WHO dysplasia system with a subdivision into
hyperplasia, mild, moderate and severe dysplasia, and CIS (20–23).
In 1991, Bouquot and Gnepp published a review of
studies on malignant transformation rates of various laryngeal
precancerous lesions: Laryngeal keratosis (leukoplakia according to
the authors' terminology), KWOA vs. KWA and laryngeal CIS (6). The studies revealed malignant
transformation rates of 0.6–39.7% for laryngeal keratosis, 0.0–16%
for KWOA, 5.6–40.0% for KWA and 3.5–90.0% for laryngeal CIS.
In 2008, Isenberg et al reviewed 15 clinical
studies on vocal cord leukoplakia between 1960 and 2005 and
included their own data from 136 patients (7). A total of 3,107 cases were included.
Histological examination revealed no dysplasia in 53.6%, mild to
moderate dysplasia in 33.5% and CIS in 15.2% of the biopsies. The
malignant transformation rates in lesions with no dysplasia, mild
to moderate dysplasia and CIS were 3.7, 10.1 and 18.1%,
respectively. The overall malignant transformation rate (all
lesions from all studies) was 8.2%.
In 2009, Gale et al reviewed 9 clinical
studies with a variety of different histological classifications
between 1982 and 2003 (n=2,841 patients) and added their own data
spanning 25 years (n=1,268 patients) (4). Corresponding grades of different
classification systems were pooled and the following malignant
transformation rates were observed: Group of squamous hyperplasia
and KWOA, 0–4.1%; group of mild dysplasia, SIN I, LIN I and
basal-parabasal hyperplasia, 0–11.5%; group of moderate dysplasia,
SIN II and LIN II, 4–24%; and group of severe dysplasia, SIN III,
LIN III, atypical hyperplasia and CIS, 9.3–57%. The total
transformation rates of all grades together ranged from 2.3% in the
authors' own data to 21.4% in a study by Blackwell et al
(24). The authors' own data
represents the largest study on the topic to date, and reported
transformation rates that were substantially lower compared with
previous studies: 1.1% in squamous hyperplasia and basal/parabasal
cell hyperplasia, 9.5% in atypical hyperplasia and 2.3% in all
grades combined.
While the aforementioned clinical studies analyzed
the malignant transformation rate of various precancerous lesions
with known histology, the perspective of primary healthcare
providers in daily otorhinolaryngology practice is based on a
population with leukoplakia of initially unknown histology. As
leukoplakia is merely a descriptive clinical term without any
histological or prognostic implications, it is important to bear in
mind that a certain percentage of these leukoplakias already
contain carcinoma at the time of first presentation. Reliable and
unbiased data on the rates of carcinoma underlying vocal cord
leukoplakia at first presentation in contrast to secondary
malignant transformation in the later course of the disease is
scarce in the literature. In 1991, Bouquot et al published
the first population-based study on laryngeal keratosis
(leukoplakia according to the authors' terminology) and laryngeal
cancer in the literature (8).
Histological examination revealed underlying invasive cancer in 12%
(carcinoma at diagnosis), while the secondary malignant
transformation rate (carcinoma after diagnosis) was merely 1%. In
comparison to 10 previous studies with hospital-based data from
1953–1983, which reported carcinoma at diagnosis in 3.5–66.7% and
carcinoma after diagnosis in 0.0–42.0% of the patients, the rates
of the present study were at the lower end of the spectrum, which
may be explained by the minimal sampling/case selection bias in a
population-based study when compared to hospital-based studies.
The results of the present German study of a
representative nationwide practice database are in line with the
findings of Bouquot's population-based study. The Kaplan-Meier
curves revealed a steep increase in laryngeal cancer diagnoses
within 6 months after the initial diagnosis of leukoplakia,
followed by a flat increase towards the end of the study period.
The initial steep increase most likely represents cases with
carcinoma underlying the initial leukoplakia (carcinoma at
diagnosis), while the later flat increase represents those with
malignant transformation in the later course of the disease
(carcinoma after diagnosis). The overall rate of laryngeal
carcinoma diagnosis increased steeply to 11.0% within 6 months of
leukoplakia diagnosis, while it increased by only 7.6% over the
following 4.5 years, which is comparable to the magnitude of the
population-based study of Bouquot et al (8). Our data indicated a similar tendency,
but with a higher estimated proportion of secondary malignant
transformation, which may be explained by the increased mean age of
our study participants when compared to the study of Bouquot et
al (58 vs. 50 years, respectively). When compared to Isenberg's
pooled malignant transformation rate of 8.2%, our estimated rate of
7.6% was within the same range (7).
The proportion of male patients with vocal cord
leukoplakia in the present study was 61.8%, which is at the lower
end of the spectrum compared with the results of previous studies
(6,25,26). In
addition, the present study identified advanced age as a risk
factor for the diagnosis of laryngeal carcinoma in patients with
vocal cord leukoplakia. This may be easily explained by the latency
of progression from precancerous lesions to invasive cancer, and is
consistent with the findings of previous studies (8,27).
Our study was subject to several limitations. First,
an exact differentiation between carcinoma at diagnosis and
carcinoma after diagnosis was not possible, as the data were based
solely on ICD codes, whereas clinical information and histological
results were not included in the database. In addition, no
information on TNM status or stage was available. Moreover,
although neoplasms of the supraglottis, subglottis and laryngeal
cartilage were excluded, it cannot be ascertained whether the
diagnosed cancers have evolved from the previously diagnosed
leukoplakia or possibly from another laryngeal site. For the same
reason, the diagnostic procedures were not standardized and the
accuracy of the diagnoses could not be validated. Finally,
information on pre-existing medical conditions and risk factors,
including smoking behavior, alcohol use and gastroesophageal
reflux, was lacking. Moreover, other relevant parameters, such as
voice quality or quality of life, could not be obtained.
An advantage of the study design is the presentation
of a large and current sample of routine demographic data from the
German healthcare system (real-world data), which allows for a
certain reliability of the results and associations. To the best of
our knowledge, this is the first time that the association of vocal
cord leukoplakia with laryngeal cancer has been analyzed
systematically using a representative nationwide practice database.
In comparison to previous studies with hospital-based data, a
sampling or case selection bias is most likely reduced by the
present study design.
In conclusion, this representative nationwide study
of otorhinolaryngology practices in Germany revealed that
approximately 1 in 5 patients with vocal cord leukoplakia exhibited
either carcinoma at diagnosis or malignant transformation within 5
years. A high index of suspicion by physicians is required in older
patients, particularly in men. A close follow-up of high-risk
patients is recommended, even if the results of the initial biopsy
were negative.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KK contributed substantially to the conception,
design and interpretation of the data and critically revised the
manuscript for important content. DUS, AS and MK critically revised
the manuscript for important content. LJ contributed to the
analysis and interpretation of the data and drafted the manuscript.
All authors have read and approved the final version of the
manuscript to be published.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
German law allows the use of anonymous electronic
medical records for research purposes under certain conditions.
According to this legislation, it is not necessary to obtain
informed consent from patients or approval from a medical ethics
committee for this type of observational study that contains no
directly identifiable data. Therefore, no waiver of ethical
approval was obtained from an Institutional Review Board or ethics
committee. The authors had no access to any identifying information
at any moment during the analysis of the data.
Competing interests
All authors declare that they have no competing
interests.
References
|
1
|
Parker NP: Vocal fold leukoplakia:
Incidence, management, and prevention. Curr Opin Otolaryngol Head
Neck Surg. 25:464–468. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Frangez I, Gale N and Luzar B: The
interpretation of leukoplakia in laryngeal pathology. Acta
Otolaryngol Suppl. 527 sup527:142–144. 1997.https://doi.org/10.3109/00016489709124058
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang D, Zhou J, Chen B, Zhou L and Tao L:
Gastroesophageal reflux and carcinoma of larynx or pharynx: A
meta-analysis. Acta Otolaryngol. 134:982–989. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gale N, Michaels L, Luzar B, Poljak M,
Zidar N, Fischinger J and Cardesa A: Current review on squamous
intraepithelial lesions of the larynx. Histopathology. 54:639–656.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Flint PW, Haughey PH, Robbins KT, Thomas
JR, Niparko JK, Lund VJ and Lesperance MM: Cummings Otolaryngology
- Head and Neck Surgery. 6th edition. Saunders; 2015, PubMed/NCBI
|
|
6
|
Bouquot JE and Gnepp DR: Laryngeal
precancer: A review of the literature, commentary, and comparison
with oral leukoplakia. Head Neck. 13:488–497. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Isenberg JS, Crozier DL and Dailey SH:
Institutional and comprehensive review of laryngeal leukoplakia.
Ann Otol Rhinol Laryngol. 117:74–79. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bouquot JE, Kurland LT and Weiland LH:
Laryngeal keratosis and carcinoma in the Rochester, MN, population
1935–1984. Cancer Detect Prev. 15:83–91. 1991.PubMed/NCBI
|
|
9
|
Becher H, Kostev K and Schröder-Bernhardi
D: Validity and representativeness of the ‘Disease Analyzer’
patient database for use in pharmacoepidemiological and
pharmacoeconomic studies. Int J Clin Pharmacol Ther. 47:617–626.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jacob L, Hadji P and Kostev K: Age-related
differences in persistence with bisphosphonates in women with
metastatic breast cancer. J Bone Oncol. 5:63–66. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jacob L, Kalder M, Arabin B and Kostev K:
Impact of prior breast cancer on mode of delivery and
pregnancy-associated disorders: A retrospective analysis of
subsequent pregnancy outcomes. J Cancer Res Clin Oncol.
143:1069–1074. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rathmann W and Kostev K: Association of
dipeptidyl peptidase 4 inhibitors with risk of metastases in
patients with type 2 diabetes and breast, prostate or digestive
system cancer. J Diabetes Complications. 31:687–692. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
McGavran MH, Bauer WC and Ogura JH:
Isolated laryngeal keratosis: Its relation to carcinoma of the
larynx based on a clinicopathologic study of 87 consecutive cases
with long-term follow-up. Laryngoscop. 70:932–950. 1960. View Article : Google Scholar
|
|
14
|
Gabriel CE and Jones DG: Hyperkeratosis of
the larynx. J Laryngol Otol. 76:947–957. 1962. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Norris CM and Peale AR: Keratosis of the
larynx. J Laryngol Otol. 77:635–647. 1963. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kleinsasser O: Über die verschiedenen
Formen der Plattenepithelhyperplasien im Kehlkopf und ihre
Beziehungen zum Carcinom. Arch Ohren Nasen Kehlkopfheilkd.
174:290–313. 1959. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kleinsasser O: Über den Krankheitsverlauf
bei Epithelhyperplasien der Kehlkopfscheimhaut und die Entstehung
von Karzinomen: IV. Mitteilung. Z Laryngol Rhinol Otol. 42:541–558.
1963.PubMed/NCBI
|
|
18
|
Crissman JD and Zarbo RJ: Dysplasia, in
situ carcinoma, and progression to invasive squamous cell carcinoma
of the upper aerodigestive tract. Am J Surg Pathol. 13 Suppl
1:5–16. 1989.PubMed/NCBI
|
|
19
|
Resta L, Colucci GA, Troia M, Russo S,
Vacca E and Delfino Pesce V: Laryngeal intraepithelial neoplasia
(LIN). An analytical morphometric approach. Pathol Res Pract.
188:517–523. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kambic V and Lenart I: [Our classification
of hyperplasia of the laryngeal epithelium from the prognostic
point of view]. J Fr Otorhinolaryngol Audiophonol Chir Maxillofac.
20:1145–1150. 1971.(Our classification of hyperplasia of the
laryngeal epithelium from the prognostic point of view). PubMed/NCBI
|
|
21
|
Gale N, Pilch BZ, Sidransky D, Westra WH
and Califano J: Epithelial precursor lesionsWorld Health
Organization classification of tumour Pathology and genetics of
head and neck tumours. Barnes LEJ, Reichart P and Sidransky D:
IARC; Lyon: pp. 140–143. 2005
|
|
22
|
Fleskens S and Slootweg P: Grading systems
in head and neck dysplasia: Their prognostic value, weaknesses and
utility. Head Neck Oncol. 1:112009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gale N, Blagus R, El-Mofty SK, Helliwell
T, Prasad ML, Sandison A, Volavšek M, Wenig BM, Zidar N and Cardesa
A: Evaluation of a new grading system for laryngeal squamous
intraepithelial lesions-a proposed unified classification.
Histopathology. 65:456–464. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Blackwell KE, Calcaterra TC and Fu YS:
Laryngeal dysplasia: Epidemiology and treatment outcome. Ann Otol
Rhinol Laryngol. 104:596–602. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lampert T, von der Lippe E and Müters S:
Verbreitung des Rauchens in der Erwachsenenbevölkerung in
Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in
Deutschland (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung
Gesundheitsschutz. 56:802–808. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mourad M, Jetmore T, Jategaonkar AA,
Moubayed S, Moshier E and Urken ML: Epidemiological Trends of Head
and Neck Cancer in the United States: A SEER Population Study. J
Oral Maxillofac Surg. 75:2562–2572. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gallo A, de Vincentiis M, Della Rocca C,
Moi R, Simonelli M, Minni A and Shaha AR: Evolution of precancerous
laryngeal lesions: A clinicopathologic study with long-term
follow-up on 259 patients. Head Neck. 23:42–47. 2001. View Article : Google Scholar
|