Case report
A 47-year-old woman with a 1-year history of
resected (right modified radical mastectomy) invasive breast
carcinoma of the right breast (pT1N0M0) presented to the Department
of Breast Surgery of The Second Hospital of Dalian Medical
University (Dalian, China) for a regular follow-up visit in January
2014. Breast ultrasound examination revealed a neoplasm in the left
breast, with sand-like calcifications (0.6×0.7 cm2,
BI-RADS score IVB). Due to the previous history of a malignant
tumor, further surgery was required to reach an accurate diagnosis.
Therefore, segmental left mastectomy was scheduled to remove the
lesion. Ultrasound-guided wire localization of the non-palpable
left breast lesion was performed preoperatively at the Department
of Ultrasound. Due to the numerous surgeries scheduled on that day,
the patient was required to wait for ~6 h. When the patient was
finally taken to the operating theater, the localization wire had
disappeared. It was first considered that the localization wire had
become detached and fallen off; however, we were unable to find it.
We then considered the possibility that the wire was located within
the mammary tissue, and proceeded with the segmental mastectomy,
along with the preoperative skin marker; however, following tumor
resection, the localization wire could not be identified in the
mammary gland. The intraoperative pathology report revealed a
benign breast lesion (breast fibroadenoma). As the possibility that
the localization wire had entered the pleural cavity could not be
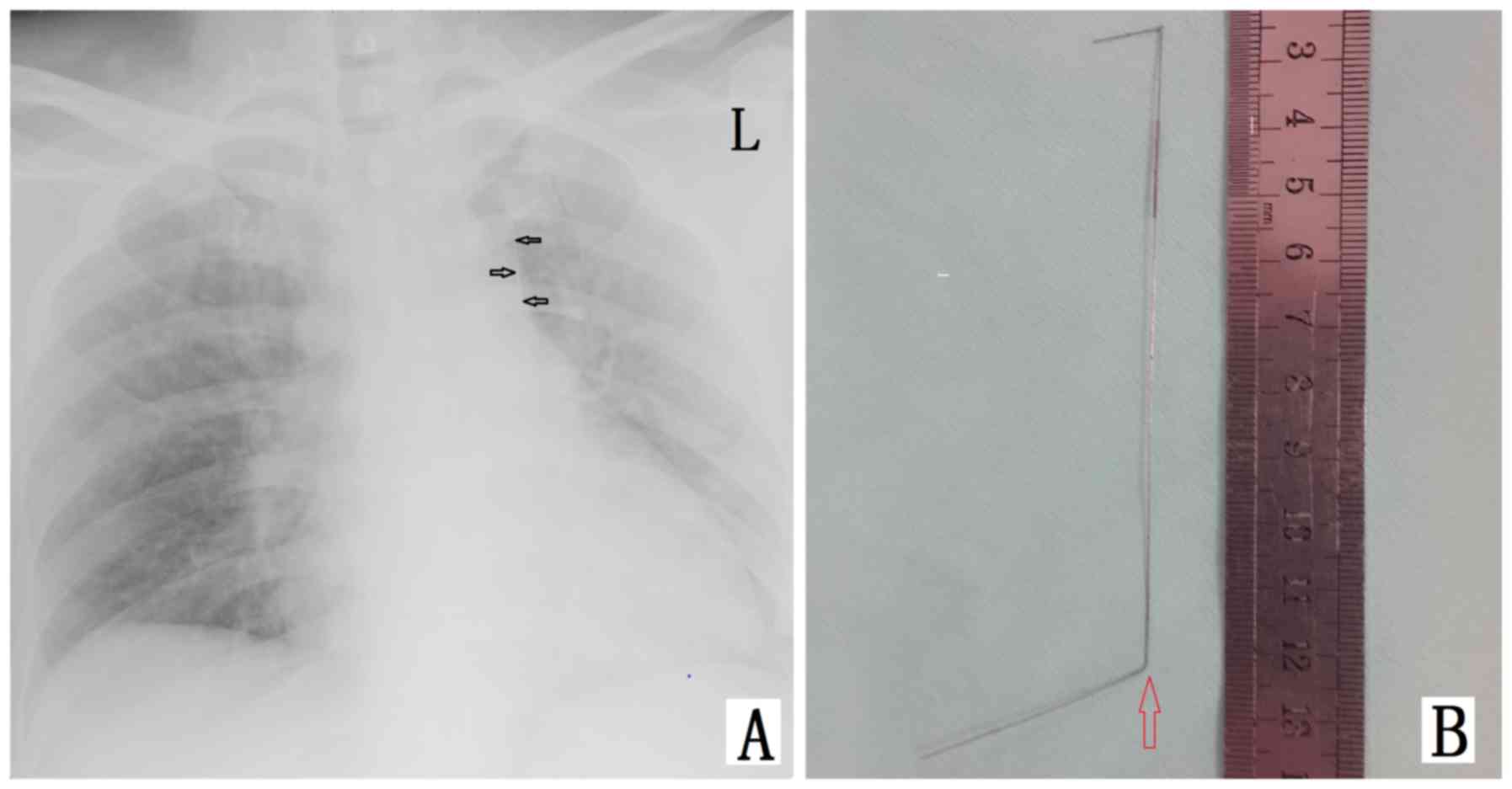
excluded, plain chest X-ray was performed intraoperatively
(Fig. 1), followed by a computed
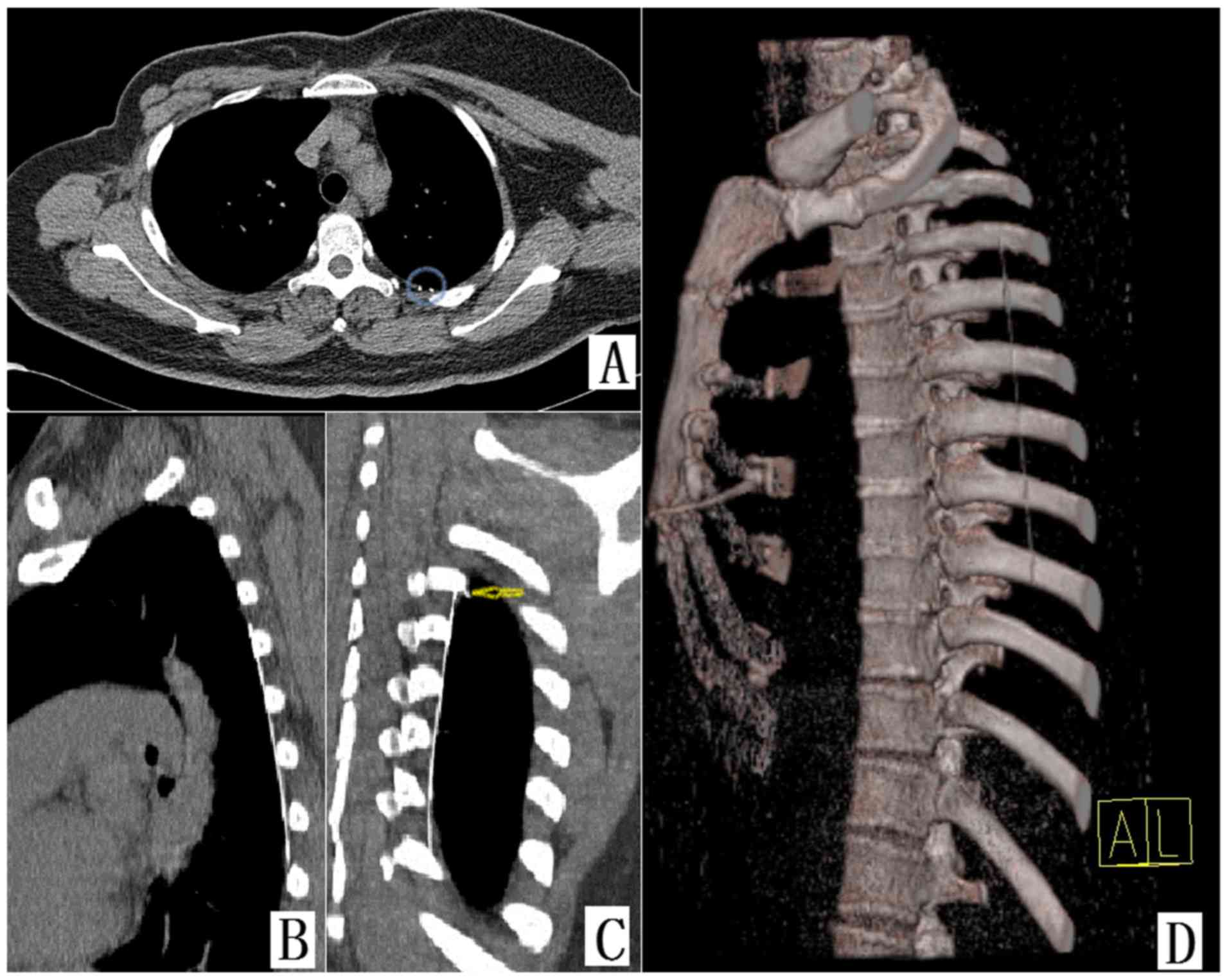
tomography (CT) scan to accurately evaluate the location of the
wire. The wire was located in the left pleural cavity (Fig. 2) and it was removed by the thoracic
surgeons under thoracoscopic guidance. After 1 week, the patient
was re-examined with a CT scan and was released from the
hospital.
Discussion
Preoperative ultrasound-guided wire localization is
an effective method for assisting surgeons in resecting
non-palpable breast lesions (1–4).
However, little is known on the complications associated with the
use of ultrasound-guided wire localization. We herein present an
unusual case of an ectopic breast localization wire in the pleural
cavity. To the best of our knowledge, this is the first report of
this type of complication.
Apart from ultrasound-guided wire localization,
alternative methods for breast tumor localization include
preoperative skin markers and intraoperative ultrasound. However,
these techniques may result in inaccurate tumor localization due to
skin mobility and body position changes (3–5). Two
main factors may have contributed to this unusual complication: One
was the unusually long waiting period, during which the
localization wire may have been pushed out of its original
position, which is considered to be quite dangerous. In addition,
the depth of the localization wire was questioned. If the
localization wire is erroneously inserted to a greater depth, it
may enter the pleural cavity. However, the pectoralis major is a
thick fan-shaped muscle with a tough fascia. In fact, it would be
quite difficult to advance the wire to that depth; furthermore, the
ultrasound doctors who performed the procedure are highly
experienced (>10 years of clinical practice) and were assisted
by experienced surgeons. Therefore, it is extremely unlikely that
the localization wire was introduced into the pleural cavity under
ultrasound guidance, without any patient-reported symptoms. None of
the two possibilities appears to be a plausible explanation for
this complication. However, in the future, the operation time
should be better coordinated with the time of ultrasound-guided
wire localization to reduce the waiting period.
Needle-track seeding is a rare but important
complication of ultrasound-guided procedures (1–5). In the
present case, as the lesion was reported to be benign based on
postoperative pathology, the risk of pleural metastasis did not
appear to be a concern. In addition, the patient had fully
recovered after 1 week. However, the risk of needle-track seeding,
as well as that of other high-risk complications, such as lethal
left pneumothorax and severe pulmonary injury, should not be
ignored. To the best of our knowledge, there have been no reports
of an ectopic breast localization wire in the pleural cavity in the
English literature to date.
The patient provided written informed consent to the
publication of the case details and associated images, and the
study protocol and the sample collection were approved by the
Ethics Committee of Dalian Medical University.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81071127, 81471751
and 81673762 to Dr Zuowei Zhao; grant no. 81650018 to Dr Man Li),
and the Provincial Natural Science Foundation of Liaoning (grant
no. 2014921059 to Dr Zuowei Zhao; grant no. 2014023025 to Dr Man
Li).
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Plecha D, Bai S, Patterson H, Thompson C
and Shenk R: Improving the accuracy of axillary lymph node surgery
in breast cancer with ultrasound-guided wire localization of biopsy
proven metastatic lymph nodes. Ann Surg Oncol. 22:4241–4246. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Krekel NM, Zonderhuis BM, Stockmann HB,
Schreurs WH, van der Veen H, de Lange de Klerk ES, Meijer S and van
den Tol MP: A comparison of three methods for nonpalpable breast
cancer excision. Eur J Surg Oncol. 37:109–115. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dua SM, Gray RJ and Keshtgar M: Strategies
for localisation of impalpable breast lesions. Breast. 20:246–253.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Postma EL, Verkooijen HM, van Esser S,
Hobbelink MG, van der Schelling GP, Koelemij R, Witkamp AJ, Contant
C, van Diest PJ, Willems SM, et al: Efficacy of ‘radioguided occult
lesion localisation’ (ROLL) versus ‘wire-guided localisation’ (WGL)
in breast conserving surgery for non-palpable breast cancer: A
randomised controlled multicentre trial. Breast Cancer Res Treat.
136:469–478. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ishizuna K, Ota D, Okamoto J, Fukuuchi A,
Tanaka R, Fujii A, Mori M and Nishi T: A case of mucinous carcinoma
of the breast in which needle tract seeding was diagnosed by
preoperative diagnostic imaging. Breast Cancer. 18:324–327. 2011.
View Article : Google Scholar : PubMed/NCBI
|