Introduction
Proximal-type epithelioid sarcoma (PES) of the vulva
is an exceedingly rare malignant soft tissue tumor. The first case
of vulvar PES was described in 1972 (1), and <60 cases have been reported in
the literature to date. Compared with other soft tissue tumors,
accurate diagnosis of this neoplasm is generally challenging due to
its rarity and the likelihood of misdiagnosis as a benign lesion,
including Bartholin's gland cyst, Bartholin's gland abscess,
inguinal or femoral hernias or other benign soft tissue tumors
(2).
Several imaging modalities have been used to assess
soft tissue tumors, including ultrasonography (US), computed
tomography (CT) and magnetic resonance imaging (MRI), plain
radiography and positron emission tomography (PET). US in
particular is the most common first-line examination in vulvar
lesions due to its real-time and radiation-free properties. As PES
lesions may present with various and non-specific signs and
symptoms, the US findings of vulvar PES may lack specificity
compared with other solid masses. However, US can assess the mass
size, shape, echogenicity, margin, composition and vascularity
(3). Furthermore, to the best of our
knowledge, US and CDUS findings of vulvar PES have not been
described in the literature to date. In the present study, the case
of a patient with vulvar PES is presented and the US and CDUS
findings are discussed.
Case report
A 41-year old female patient presented to the
Department of Ultrasonography of Chengdu First People's Hospital
(Chengdu, China) in May 2017, with complaints of a painless mass in
the right mons pubis that she had first noticed 3 years prior. The
patient had no other significant medical history and her family
history did not include malignancies in first-degree relatives.
Gynecological examination of the vagina, cervix and uterus appeared
normal. Inspection of the vulva revealed a mass 2 cm in greatest
diameter in the right mons pubis. Physical examination of the mass
revealed a non-tender nodule with a smooth surface and hard
consistency. No other abnormalities were observed on physical
examination. Gray-scale US and CDUS of the vulva were performed
with a MyLab Twice ultrasound scanner (Esaote, Genova, Italy) and a
5–10 MHZ multifrequency linear-array transducer. A prominent
homogenous hypoechoic and ovoid solid mass with a well-defined
border, sized 27×11 mm, was detected in the subcutaneous tissue in
the right mons pubis. CDUS and pulse Doppler US revealed arterial
blood flow with low resistivity index and low systolic peaks (20.9
cm/sec) in the mass (Fig. 1). The
mass was clinically considered to be a benign lesion and was
removed by excisional biopsy.
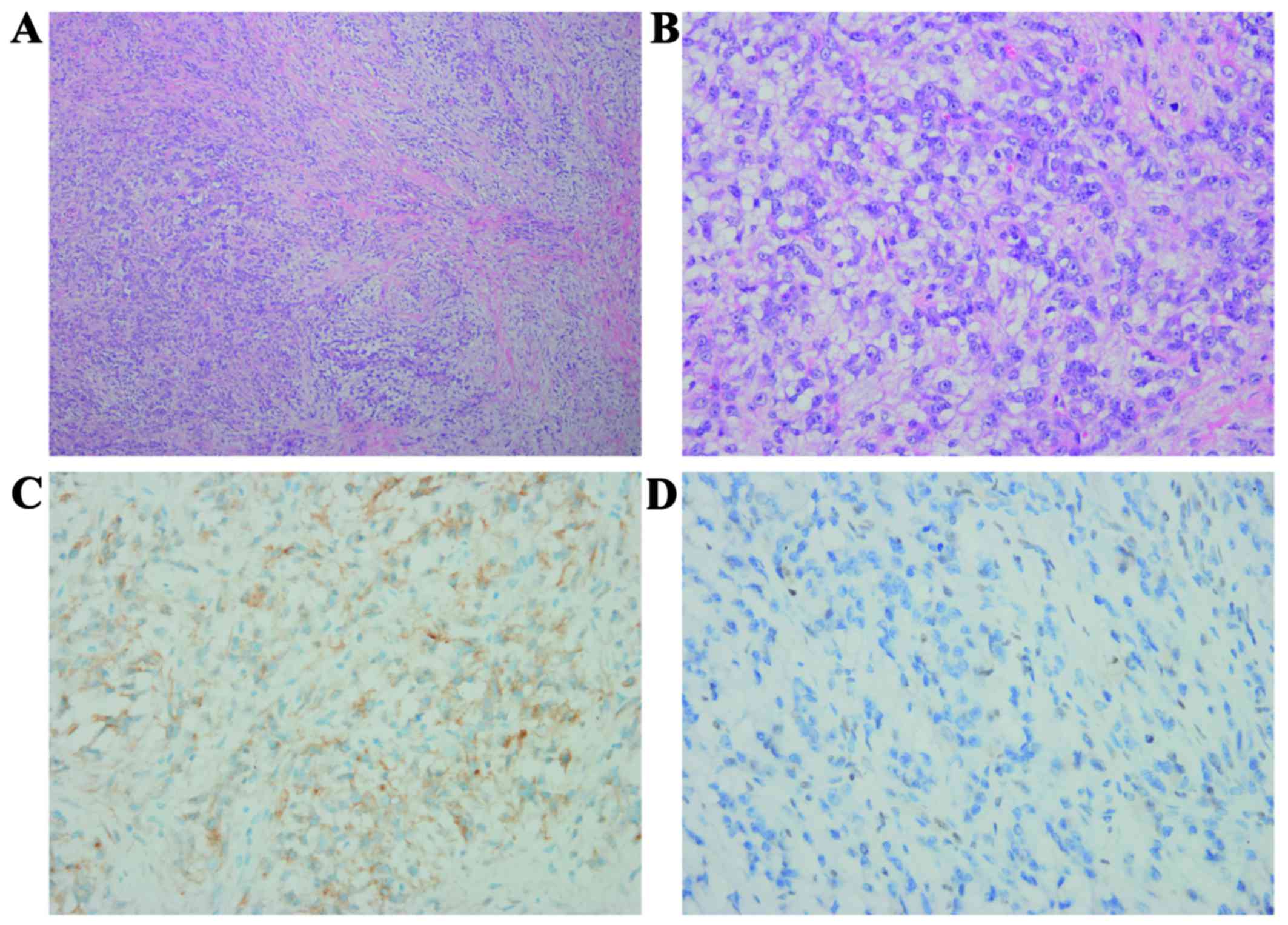
The initial pathology report suggested that the mass
was rich in myxoid stroma. Subsequently, the surgical specimen was
sent to the West China Hospital for consultation. The results of
the immunohistochemical staining of the specimen were as follows:
Negative for S100 protein, desmin, CD31, CD34, P40, P63,
erythroblast transformation-specific-related gene, anaplastic
lymphoma kinase-1, cytokeratin (CK)18, PAN-CK, smooth muscle actin
and myogenin; the Ki-67 (MIB-1) index was positive (15% of the
nuclei); the specimen was positive for epithelial membrane antigen
(EMA) (Fig. 2). Additional INI1
staining revealed a complete loss of expression in tumor cells.
These immunohistochemical results confirmed the diagnosis of vulvar
PES (myxoid variant) in the right mons pubis. The patient underwent
a second excision at the Sichuan Cancer Hospital. There were no
residual tumor cells found in the first surgical area. The patient
is currently well, without evidence of recurrence or metastasis, 9
months after the operation. During the follow-up period, the
patient did not receive any adjuvant therapy.
Discussion
Epithelioid sarcoma (ES), first described by
Enzinger in 1970 (4), as an
independent entity, is a rare neoplasm accounting for <1% of
adult soft tissue sarcomas. Two histological variants have been
identified: Classic ES (also referred to as distal-type ES) and
proximal-type ES. The former generally occurs in the distal
extremities (mostly the hand or wrist) of adolescents and young
adults, and it may appear as solitary or multinodular lesions
involving either the deep or superficial soft tissues. The latter
is rarer, generally occurring in middle-aged or older patients. It
often develops in the axilla and the genital area (groin, mons
pubis, clitoris and vulva) (5). The
most common initial symptom of vulvar PES is a slowly growing,
relatively painless mass in the labia majora. Due to its benign
appearance as a painless subcutaneous nodule, diagnosis and
treatment may often be delayed (6).
In the present case, PES occurred in the mons pubis as a
slow-growing, painless mass. The mass was clinically considered to
be a benign lesion and was removed by excisional biopsy.
US, CT and MRI, plain radiography and PET have been
used to assess soft tissue tumors. As US is cost-effective,
non-invasive, real-time and easy to perform, it has been used as
the main first-line examination method for evaluating soft tissue
tumors over several years (7). Due
to the technological advances, US can be more sensitive to the
detection of minute lesions. Furthermore, the combination of CDUS
and spectral analysis may depict the vascularity in malignant
tumors, whereas other imaging modalities cannot obtain this type of
information (8). In addition,
together with clinical examination, US-guided needle biopsy is a
more cost-effective method for confirming the final diagnosis
(3). Compared with other benign
masses, soft tissue sarcomas are more likely to recur and
metastasize after surgery. Fornage et al (9) reported that US may not definitively
distinguish between recurrent tumor and postsurgical changes in the
early postoperative period (3–6 months); however, the sensitivity
and specificity of US for identification of recurrent tumors was
comparable to that of routine MRI for long-term follow-up.
Immunohistochemistry is useful for differentiating
epithelioid sarcomas from other tumors, including other sarcomas
with epithelioid cells, malignant melanoma, metastatic carcinoma
and malignant extrarenal rhabdoid tumor (MERT) (10). Generally, vulvar PES expresses
epithelioid and mesenchymal markers, such as vimentin, EMA, CKs and
CD34. Staining for S100 or HMB45 to exclude malignant melanoma is a
particularly useful differential diagnosis for PES and MERT. The
innovative molecular marker INI 1 may also be used in the
differential diagnosis of soft tissue tumors (11).
Optimal treatment for PES of the vulva has not been
established due to its rarity. There is no universally accepted
treatment for vulvar epithelioid sarcoma (12). However, the cornerstone of initial
management is wide surgical excision with an adequate margin (≥2
cm) (13). The role and selection of
adjuvant therapy also remain unclear due to the rarity of this
disease. Adjuvant radiotherapy is advocated in high-grade tumors or
cases with inadequate surgical margins (14), and also due to the high incidence of
local recurrence and distant metastasis (15). However, the results of radiotherapy
are controversial and show no statistically significant reduction
in mortality (16). The role of
chemotherapy in the adjuvant setting appears marginally effective
at best for the treatment of metastatic disease (17).
In conclusion, US and CDUS may be used to evaluate
vulvar PES, a rare soft tissue sarcoma, by location, echogenicity,
margin, shape, composition, sound transmission and vascularity,
although vulvar PES generally presents as a non-specific solid
mass. Combination with other imaging modalities may aid the
diagnosis. However, definite diagnosis relies on the
histopathological examination.
Acknowledgements
The authors gratefully acknowledge the assistance of
Dr Buyun Ma, Department of Ultrasonography, West China Hospital,
Sichuan University (Chengdu, China).
Funding
No funding was received.
Availability of materials and data
Not applicable.
Authors' contributions
YY analyzed the clinical data and drafted the
manuscript. YL provided the pathological results. YC provided
ultrasound examination results and conducted follow-up on the
patient in the outpatient clinic. ZT provided professional guidance
on pathological results. XM contributed to critical review and
supervised the entire study. All the authors have read and approved
the final version of this manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
The authors declare no potential conflicts of
interest with respect to the research, authorship and/or
publication of this article.
References
|
1
|
Piver MS, Tsukada Y and Barlow J:
Epithelioid sarcoma of the vulva. Obstet Gynecol. 40:839–842.
1972.PubMed/NCBI
|
|
2
|
Altundag K, Dikbas O, Oyan B, Usubutun A
and Turker A: Epithelioid sarcoma of vulva: A case report and
review of the literature. Med Oncol. 21:367–372. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fornage BD: Soft-tissue masses: The case
for increased utilization of sonography. Ald Radiol. 29:8–22.
2000.
|
|
4
|
Enzinger FM: Epithelioid sarcoma. A
sarcoma simulating a granulomas or a carcinom. Cancer.
26:1029–1041. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Moore RG, Steinhoff MM, Granai CO and
Demars LR: Vulvar epithelioid sarcoma in pregnancy. Gynecol Oncol.
85:218–222. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ulutin HC, Zellars RC and Frassica D: Soft
tissue sarcoma of the vulva: A clinical study. Int J Gynecol
Cancer. 13:528–531. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi H, Varma DG, Fornage BD, Kim EE and
Johnston DA: Soft-tissue sarcoma: MR Imaging vs sonography for
detection of local recurrence after surgery. AJR Am J Roentgenol.
157:353–358. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Belli P, Costantini M, Mirk P, Maresca G,
Priolo F and Marano P: Role of Color Doppler Sonography in the
assessment of musculoskeletal soft tissue masses. J Ultrasound Med.
19:823–830. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fornage BD: Soft tissue masses: The
underutilization of sonography. Semin Musculoskelet Radiol.
3:115–134. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Guillou L, Wadden C, Coindre JM, Krausz T
and Fletcher CD: ‘Proximal-type’ epithelioid sarcoma, distinctive
aggressive neoplasm showing rhabdoid features. Clinico pathologic,
immunohistochemical, and ultrastructural study of a series. Am J
Surg Pathol. 21:130–146. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hornick JL, Dal Cin P and Fletcher CD:
Loss of INI1 expression is characteristic of both conventional and
proximal-type epithelioid sarcoma. Am J Surg Pathol. 33:542–550.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lacazzo C, Gkegkes ID and Vrachnis N:
Dilemmas in the management of patients with vulvar epithelioid
sarcoma: A literature review. Eur J Obstet Gynecol Reprod Biol.
176:1–4. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bos GD, Pritchard DJ, Reiman HM, Dobyns
JH, Ilstrup DM and Landon GC: Epithelioid sarcoma. An analysis of
fifty-one cases. J Bone Joint Surg. 70:862–870. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Casanova M, Ferrari A, Collini P, Bisogno
G, Alaggio R, Cecchetto G, Gronchi A, Meazza C, Garaventa A, Di
Cataldo A, et al: Epithelioid sarcoma in children and adolescents:
A report from the Italian soft tissue sarcoma committee. Cancer.
106:708–717. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hasegawa T, Matsuno Y, Shimoda T, Umeda T,
Yokoyama R and Hirohashi S: Proximal-type epithelioid sarcoma: A
clinicopathologic study of 20 cases. Mod Pathol. 14:655–663. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Evans HL and Baer SC: Epithelioid sarcoma:
A clinicopathologic and prognostic study of 26 cases. Semin Diagn
Pathol. 10:286–291. 1993.PubMed/NCBI
|
|
17
|
Argenta PA, Thomas S and Chura JC:
Proximal-type epithelioid sarcoma vs. malignant rhabdoid tumor of
the vulva: A case report, review of the literature, and an argument
for consolidation. Gynecol Oncol. 107:130–135. 2007. View Article : Google Scholar : PubMed/NCBI
|