Introduction
Rectal cancer has the fourth highest incidence among
malignant tumors in China, and 70% of rectal cancers are located in
the lower rectum (1). Rectal cancer
has a high mortality rate, mainly attributed to local recurrence,
lymphatic metastasis and hematogenous metastasis (2). Surgical resection is the main treatment
for rectal cancer. In recent years, with the rapid development of
endoscopic techniques, laparoscopic resection of rectal cancer has
become the preferred surgical method, as it involves less trauma,
less pain, faster recovery, minor scarring and fewer complications,
among other advantages (3). Total
mesorectal excision (TME) is generally well-received by surgeons,
although whether to preserve the left colic artery (LCA) during
surgery remains controversial (4).
Preservation of the LCA involves the ligation of
blood vessels in the lower part of the LCA that originates from the
lower part of inferior mesenteric artery (IMA), while cutting the
LCA involves the ligation of blood vessels near the origin of the
IMA and dissection of the regional lymph nodes (5). However, further study is required to
determine whether the effects of two surgical methods on patient
prognosis differ significantly and which method is more beneficial
for patients. To this end, systematic evaluation and meta-analysis
were used to comprehensively evaluate the clinical efficacy of
laparoscopic resection of rectal cancer with and without
preservation of the LCA, hoping to provide information that may
serve as a reference for decision making in clinical practice.
Materials and methods
Search strategy
Under the supervision of TJY and CYY, CSZ and DWF
systematically searched the PubMed, Ovid, Embase, Web of Science,
CBM, CNKI, VIP and WanFang Data databases prior to June 2017 for
studies comparing LCA preservation and non-preservation in
laparoscopic resection for rectal cancer. In addition, the
reference lists of the studies were obtained to supplement the
literature. The following free-text terms and MeSH terms were used
to identify the studies: Left colic artery, left colonic artery,
rectal cancer, rectal carcinoma, laparoscopic, randomized
controlled trial and controlled clinical trial.
Study selection and inclusion
criteria
The inclusion criteria were as follows: i)
Randomized controlled trial (RCT) or quasi-RCT, which is a
quasi-randomised trial that uses a quasi-random method of
allocating participants to different interventions (this design is
frequently used when it is not logistically feasible or ethical to
conduct an RCT); ii) patients with rectal cancer diagnosis without
limitations regarding age, race, nationality or disease course;
iii) laparoscopic resection performed for rectal cancer, with the
experimental group retaining and the control group not retaining
the LCA; and iv) the results referred to at least one quantitative
study. The data extraction included: i) Basic information about the
research, including title, author, publication date, etc.; ii) the
baseline objective and the details of the intervention; iii) key
elements of the risk assessment; and iv) outcome indicators and
outcome measurement data, including operative time, estimated blood
loss, percentage of neostomy, amount of anastomotic leakage, number
of retrieved IMA lymph nodes, postoperative hospital stay,
incidence of recurrence and incidence of metastasis. The exclusion
criteria were as follows: i) Previously published literature; ii)
literature not published in Chinese or English; iii) loss of
>20% of patients during follow-up; iv) inability to extract the
relevant data from the original literature or contact the author;
and v) presence of tumors outside the rectum including extra-rectal
metastasis and primary tumors associated with rectal cancer.
Quality assessment
Two researchers (CSZ and XHL) independently reviewed
and extracted the required data, which were cross-checked.
Disagreements were resolved by a third researcher (YW). Attempts
were made to contact the original authors to supplement missing
data. During literature screening, the title of the article we
first read to exclude studies that were clearly irrelevant, and
then the abstract and the full text were read to determine whether
or not to include the study in question. The bias risk assessment
included in the study was independently evaluated by two
researchers (CSZ and CYY) based on the Cochrane Collaboration
Network for RCT bias assessment tools to assess the risk of
inclusion bias. Risk and bias were assessed in the following areas:
Random sequence generation, allocation concealment, blinding of
participants and personnel, blindness of outcome assessment,
incomplete outcome date, selective reporting and other bias. The
studies were divided into three groups based on the assessment of
bias, namely high, low and unclear risk of bias. In the course of
the assessment, in case of divergence, it was settled by discussion
or submitted to a third researcher.
Statistical analysis
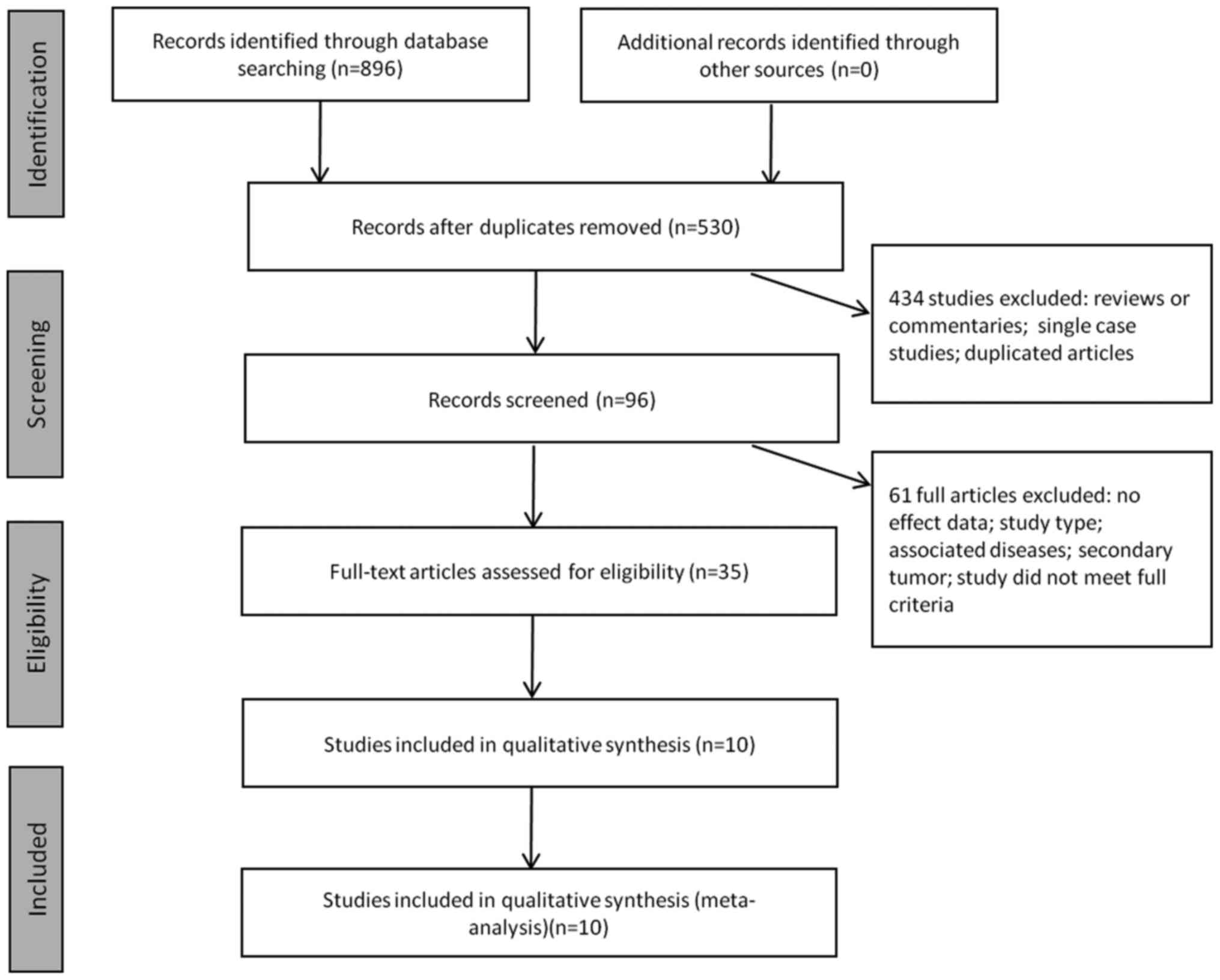
A total of 10 studies (6–15)
involving 1,471 patients with rectal cancer were finally included
in the meta-analysis (Fig. 1). The
search strategy is summarized in File S1. Meta-analysis was
performed using RevMan 5.3 software (Cochrane Community). Relative
risk (RR) was calculated for enumeration data as effect indicators,
and mean deviation (MD) was calculated for measurement data as
effect indicators. Additionally, each effect indicator was given a
point estimate and 95% confidence interval (CI) (16). The heterogeneity of the included
studies was analyzed by χ2 test (test level α=0.1) and
quantitatively determined by I2 statistics. If there was no
statistical heterogeneity among the results, the fixed-effects
model was used for meta-analysis; if statistical heterogeneity was
indeed present in the results of the study, the random-effects
model was used for meta-analysis after the obvious clinical
heterogeneity of the impact was excluded. Subgroup analysis or
sensitivity analysis was used when clinical studies had significant
heterogeneity or when only conducting descriptive analysis
(17). The level of significance was
α=0.05.
Results
The literature screening process and results are
presented in Fig. 1. The clinical
characteristics and related information regarding the patients
included in this study are shown in Table I. The main results of this study are
as follows:
 | Table I.Characteristics of the studies
included in the meta-analysis. |
Table I.
Characteristics of the studies
included in the meta-analysis.
|
|
|
| Tumor size (cm) | Tumor location
(distance from AV, cm) | Sex
(male/female) | Inter-vention |
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Author, year | Patient no.
(T/C) | Age, years (T/C) | T | C | T | C | T | C | T | C | Outcomesa | Follow-up
(months) | (Refs.) |
|---|
| Niu, 2016 | 52/45 | 51.3/49.9 | 4.02±1.71 | 3.91±1.82 | 6.22±2.34 | 7.02±2.09 | 27/24 | 25/20 | T | C | 1, 2, 4, 5, 6, 7,
8 | 24 | (6) |
| Zhang, 2016 | 61/42 | 60.5/61.2 | 5.31±1.42 | 4.92±1.74 | 7.02±1.51 | 6.89±1.05 | 33/28 | 22/20 | T | C | 1, 2, 3, 5, 6, 9 | 4.5 | (7) |
| Rutegård, 2016 | 18/5 | 65.3/67.8 | 4.12±1.13 | 4.37±1.58 | 4.90±1.50 | 5.50±2.20 | 12/6 | 4/1 | T | C | 2, 7 | 30 | (8) |
| Yasuda 2016 | 147/42 | 64.5/68.0 | 4.35±1.33 | 4.51±1.42 | 6.62±2.10 | 6.35±1.72 | 92/55 | 26/16 | T | C | 1, 2, 3, 5, 7,
9 | 60 | (9) |
| Yamamoto, 2014 | 120/91 | 64.0/63.0 | 4.35±4.10 | 5.00±5.75 | – | – | 64/56 | 38/43 | T | C | 1, 3, 4, 5, 8,
9 | 72 | (10) |
| Matsuda, 2015 | 49/51 | 67.0/69.0 | 4.72±1.05 | 4.43±1.31 | 6.00±1.40 | 5.00±1.50 | 34/15 | 33/18 | T | C | 1, 2, 3, 7 | 12 | (11) |
| Tanaka, 2015 | 341/8 | 62.7/59.6 | 3.86±1.91 | 4.77±1.50 | 7.30±1.10 | 7.60±0.90 | 217/132 | 8/0 | T | C | 1, 2 | – | (12) |
| Liu, 2017 | 22/28 | 63.4/63.5 | 4.30±1.30 | 4.10±1.20 | 6.20±1.60 | 6.50±1.40 | 15/7 | 19/9 | T | C | 1, 2, 4, 5, 6, 7,
8 | 21.2 | (13) |
| Shen, 2014 | 72/41 | 65.6/63.4 | 4.04±1.19 | 3.91±1.37 | 6.75±1.41 | 7.10±1.56 | 45/27 | 23/18 | T | C | 1, 2, 4, 5, 6, 7,
8 | 24 | (14) |
| Takao, 2013 | 584/304 | 63.0/61.0 | 3.11±1.74 | 3.85±1.81 | 9.10±1.21 | 9.10±1.40 | 356/219 | 192/112 | T | C | 1, 2, 3, 5, 7,
9 | 24 | (15) |
Operative time
A total of 9 RCTs (6,7,9–15) were
included, involving 1,448 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was a significant difference between preservation and
non-preservation of the LCA during laparoscopic resection of rectal
cancer (RR=5.87; 95% CI: 2.60, 9.14; P<0.01; Fig. 2), with the operative time for
preservation of the LCA being comparatively longer.
Estimated blood loss
A total of 9 RCTs (7–9,11–15) were
included, involving 1,346 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was a significant difference between preservation and
non-preservation of the LCA during laparoscopic resection of rectal
cancer (RR=3.92; 95% CI; 2.04, 5.81; P<0.01; Fig. 3). In a comparison of the two groups,
preserving the LCA was associated with a larger volume of blood
loss.
Number of retrieved lymph nodes
A total of 5 RCTs (7,9–11,15) were
included, involving 961 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was a significant difference between preservation and
non-preservation of the LCA in laparoscopic resection of rectal
cancer (RR=−2.28; 95% CI: −3.08, −1.48; P<0.01; Fig. 4), higher number of retrieved nodes
were swept with LCA preservation.
Time to first postoperative
exhaust
A total of 4 RCTs (6,7,13,14) were
included, involving 207 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was a significant difference between preservation and
non-preservation of the LCA in laparoscopic resection of rectal
cancer (RR=−0.46; 95% CI: −0.60, −0.31; P<0.01; Fig. 5), as the time to the first
postoperative exhaust was reduced in patients in whom the LCA was
preserved.
Postoperative hospital stay
A total of 4 RCTs (7,9,10,15) were
included, involving 912 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was no statistically significant difference in postoperative
hospital stay between preservation and non-preservation of the LCA
in laparoscopic resection of rectal cancer (RR=−0.29; 95% CI:
−0.81, 0.23; P=0.28; Fig. 6).
Neostomy
A total of 4 RCTs (6,10,13,14)
were included, involving 266 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was a significant difference between preservation and
non-preservation of the LCA in laparoscopic resection of rectal
cancer (RR=0.16, 95% CI: 0.04, 0.62; P=0.008; Fig. 7), with the patients in whom the LCA
was preserved having a lower percentage of neostomy.
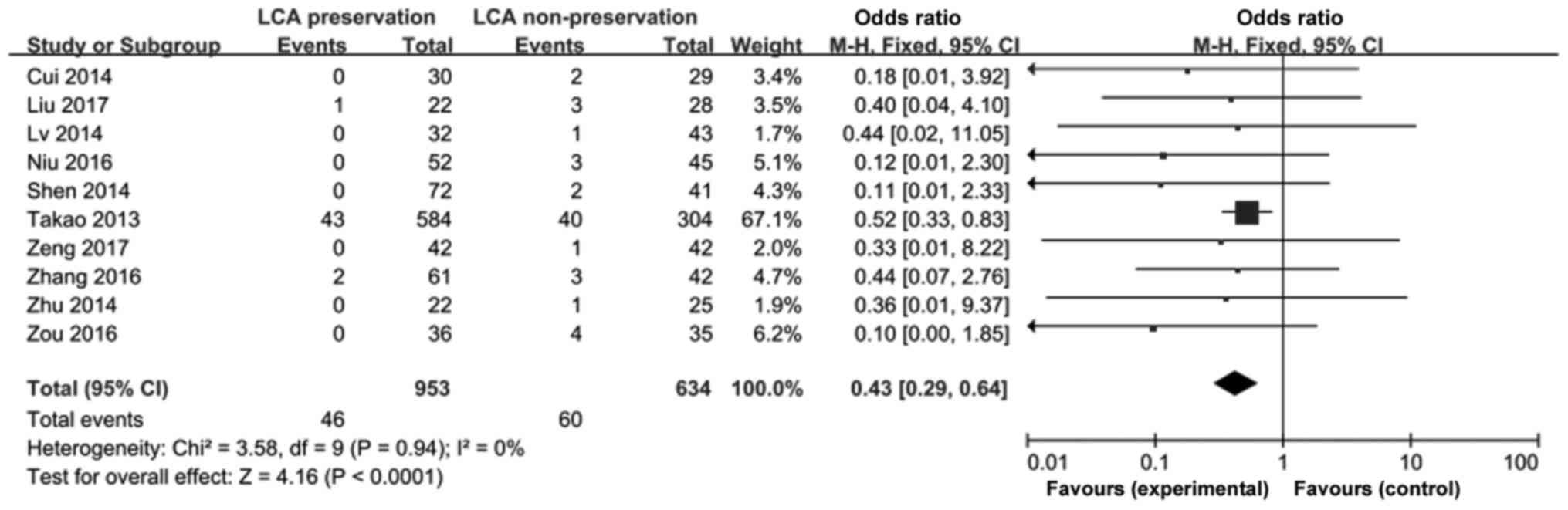
Anastomotic leakage
A total of 7 RCTs (6,7,9,10,13–15)
were included, involving 1,058 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was a significant difference between preservation and
non-preservation of the LCA in laparoscopic resection of rectal
cancer (RR=0.48, 95% CI: 0.32, 0.71; P<0.01; Fig. 8), with patients in whom the LCA was
preserved being less likely to experience anastomotic leakage.
Recurrence
A total of 7 RCTs (6,8,9,11,13–15)
were included, involving 944 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was no statistically significant difference in the risk of
recurrence between preservation and non-preservation of the LCA in
laparoscopic resection of rectal cancer (RR=0.93; 95% CI: 0.60,
1.44; P=0.73; Fig. 9).
Metastasis
A total of 4 RCTs (6,10,13,14)
were included, involving 266 patients with rectal cancer. A
meta-analysis, which applied the fixed-effects model, revealed that
there was no statistically significant difference in the risk of
metastasis between preservation and non-preservation of the LCA in
laparoscopic resection of rectal cancer (RR=0.81; 95% CI: 0.43,
1.53; P=0.52; Fig. 10).
Risk of bias assessment
Two researchers (CSZ and XHL) independently assessed
the risks and bias of the included studies. The contents of the
specific assessments included were as follows: Selection bias,
performance bias, attrition bias, reporting bias and other types of
bias (18). The details of the
Cochrane risk of bias assessment are shown in Fig. 11.
Discussion
The most serious complication of laparoscopic
surgery for rectal cancer is anastomotic leakage, which leads to
peritoneal infection and peritonitis, increasing the likelihood of
a second surgery, prolonging hospital stay, and affecting patients
undergoing chemotherapy and radiotherapy, which may pose a serious
threat to the patients' life and well-being (19,20). The
principal causes of anastomotic leakage are diverse, such as
anastomotic tension, compromised blood supply, hypoproteinemia,
bleeding and blood transfusion and prolonged operative time.
However, studies have demonstrated that the most frequent cause is
anastomotic bowel blood supply disturbances (21,22).
Traditional rectal cancer resection does not
preserve the LCA due to high ligation of the IMA, and the
anastomotic blood supply mainly comes from the marginal branch of
the middle artery of the colon. Retention of the LCA may provide a
better blood supply for the proximal colon stump. This theory has
been confirmed by intraoperative vascular Doppler surgery in
clinical studies (23–25). Komen et al (26) also confirmed that the blood supply to
the colon stump after preservation of the LCA was significantly
better compared with non-preservation. However, high ligation of
the IMA has more advantages in terms of lymph node dissection, as
the nodes in the region of the mesenteric vascular root are more
thoroughly dissected.
In the present study, systematic review and
meta-analysis were used to evaluate the correlation between
preservation and non-preservation of the LCA in laparoscopic
resection for rectal cancer. The patient complications were
systematically evaluated. Regarding intraoperative factors,
operative time, intraoperative blood loss, lymph node dissection
and the necessity of preventative colostomy were evaluated. In
terms of postoperative complications, first time passing wind
following operation, length of hospital stay, postoperative
anastomotic leakage, recurrence and metastasis were evaluated. The
results of the meta-analysis revealed that, compared with
non-preservation, preservation of the LCA was associated with
increased operative time and intraoperative blood loss. However,
preserving the LCA was associated with faster recovery and lower
incidence of anastomotic leakage. Additionally, higher surgeon
proficiency may also reduce operative time and the volume of
intraoperative blood loss. In this case, preservation of the LCA in
patients with rectal cancer may improve the prognosis.
The limitations of this study include the following:
i) The number of studies and the total number of cases is
relatively small, and the meta-analysis of test performance may
still be insufficient; ii) part of the studies do not describe the
method for generation of random sequence and the allocation of
hidden methods, which may indicate the presence of selective bias
and implementation bias; iii) the meta-analysis was limited to
literature in Chinese and English, with the studies in Chinese
accounting for a larger proportion, which is a potential source of
bias.
In summary, the evidence presented herein suggests
that preserving the LCA is associated with a more favourable
outcome in laparoscopic resection for rectal cancer compared with
non-preservation. Ensuring clinical efficacy requires long-term
follow-up and further investigation. Due to the number and quality
of research restrictions, the abovementioned conclusions require
verification by further research with larger samples and
high-quality RCTs.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Graduate
Innovation Program of Bengbu Medical College (grant no.
Byycx1752).
Availability of data and materials
All data generated or analysed during this study are
included in this published article.
Authors' contributions
Conceptualization: TJY, CSZ, DWF, XHL and CYY. Data
curation: DWF, CSZ and TJY. Formal analysis: DWF, CSZ, XHL and CYY.
Funding acquisition: TJY. Investigation: DWF, CSZ and XHL.
Methodology: TJY, DWF and CSZ. Project administration: TJY and CYY.
Resources: TJY, DWF. Software: XHL, DWF and CYY. Supervision: TJY.
Validation: DWF, CSZ and XHL. Visualization: TJY, DWF and CSZ.
Writing-original draft: DWF, CSZ and TJY. Writing-review &
editing: TJY.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
All the authors declare that they have no competing
interests to disclose.
References
|
1
|
Zhang H, Yuan W, Zhou Q, Gu X and Wang F:
Efficacy comparison of robotic and laparoscopic radical surgery in
the treatment of middle-low rectal cancer. Zhonghua Wei Chang Wai
Ke Za Zhi. 20:540–544. 2017.(In Chinese). PubMed/NCBI
|
|
2
|
Bjørn MX and Perdawood SK: Surgical
treatment of mid- and low rectal cancer. Ugeskr Laeger. 179:pii:
V11160801. 2017.(In Danish).
|
|
3
|
Kube R, Ptok H, Steinert R, Sahm M,
Schmidt U, Gastinger I and Lippert H: Clinical value of
laparoscopic surgery for colon cancer. Chirurg. 79:1145–1150.
2008.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mabardy A, Lee L, Valpato AP and Atallah
S: Transanal total mesorectal excision with intersphincteric
resection and use of fluorescent angiography and a lighted urethral
stent for distal rectal cancer. Tech Coloproctol. 21:581–582. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Guo Y, Wang D, He L, Zhang Y, Zhao S,
Zhang L, Sun X and Suo J: Marginal artery stump pressure in left
colic artery-preserving rectal cancer surgery: A clinical trial.
ANZ J Surg. 87:576–581. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Niu JW, Ning W, Wang WY, Pei DP, Meng FQ,
Liu ZZ and Cai DG: Clinical effect of preservation of the left
colonic artery in laparoscopic anterior resection for rectal
cancer. Zhonghua Yi Xue Za Zhi. 96:3582–3585. 2016.(In Chinese).
PubMed/NCBI
|
|
7
|
Zhang L, Zang L, Ma J, Dong F, He Z and
Zheng M: Preservation of left colic artery in laparoscopic radical
operation for rectal cancer. Zhonghua Wei Chang Wai Ke Za Zhi.
19:886–891. 2016.(In Chinese). PubMed/NCBI
|
|
8
|
Rutegård M, Hassmén N, Hemmingsson O,
Haapamäki MM, Matthiessen P and Rutegård J: Anterior resection for
rectal cancer and visceral blood flow: An explorative study. Scand
J Surg. 105:78–83. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yasuda K, Kawai K, Ishihara S, Murono K,
Otani K, Nishikawa T, Tanaka T, Kiyomatsu T, Hata K, Nozawa H, et
al: Level of arterial ligation in sigmoid colon and rectal cancer
surgery. World J Surg Onco. 14:992016. View Article : Google Scholar
|
|
10
|
Yamamoto M, Okuda J, Tanaka K, Ishii M,
Hamamoto H and Uchiyama K: Oncological impact of laparoscopic
lymphadenectomy with preservation of the left colic artery for
advanced sigmoid and rectosigmoid colon cancer. Dig Surg.
31:452–458. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Matsuda K, Hotta T, Takifuji K, Yokoyama
S, Oku Y, Watanabe T, Mitani Y, Ieda J, Mizumoto Y and Yamaue H:
Randomized clinical trial of defaecatory function after anterior
resection for rectal cancer with high versus low ligation of the
inferior mesenteric artery. Br J Surg. 102:501–508. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tanaka J, Nishikawa T, Tanaka T, Kiyomatsu
T, Hata K, Kawai K, Kazama S, Nozawa H, Yamaguchi H, Ishihara S, et
al: Analysis of anastomotic leakage after rectal surgery: A
case-control study. Ann Med Surg (Lond). 4:183–186. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu F and Zhang LA: A clinical comparative
study on reservation of left colic artery in laparoscopic resection
of rectal cancer. J Clin Experimental Med. 16:1013–1016. 2017.
|
|
14
|
Shen J, Li MZ, Du YF, Qu H and Zhang Y: A
comparative study of laparoscopic anterior resection of rectal
carcinoma with and without preservation of the left colonic artery.
Chin J Min Inv Surg. 14:22–24. 2014.(In Chinese).
|
|
15
|
Hinoi T, Okajima M, Shimomura M, Egi H,
Ohdan H, Konishi F, Sugihara K and Watanabe M: Effect of left
colonic artery preservation on anastomotic leakage in laparoscopic
anterior resection for middle and low rectal cancer. World J Surg.
37:2935–2943. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nonaka S, Saito Y, Takisawa H, Kim Y,
Kikuchi T and Oda I: Safety of carbon dioxide insufflation for
upper gastrointestinal tract endoscopic treatment of patients under
deep sedation. Surg Endosc. 24:1638–1645. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wolf FM: Meta-Analysis: Quantitative
methods for research synthesis by Fredric M. 1st edition. Sage
Publications Beverly Hills; CA: pp. 77–92. 1986
|
|
18
|
Gu H, Wang Y and Li W: The application of
cochrane risk of bias tools in meta-analysis of RCT. Chin Circ J.
29:147–148. 2014.
|
|
19
|
Murray AC, Chiuzan C and Kiran RP: Risk of
anastomotic leak after laparoscopic versus open colectomy. Surg
Endosc. 30:5275–5282. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Leake PA, Plummer JM, Rhoden A, Frankson
MA, Gordon-Strachan G, Powell LP and Roberts PO: Colorectal
anastomotic leakage at the university hospital of the west indies:
An analysis of risk factors. West Indian Med J. 62:711–715.
2013.PubMed/NCBI
|
|
21
|
Tocchi A, Mazzoni G, Fornasari V, Miccini
M, Daddi G and Tagliacozzo S: Preservation of the inferior
mesenteric artery in colorectal resection for complicated
diverticular disease. Am J Surg. 182:162–167. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thomas MS and Margolin DA: Management of
colorectal anastomotic leak. Clin Colon Rectal Surg. 29:138–144.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sekimoto M, Takemasa I, Mizushima T, Ikeda
M, Yamamoto H, Doki Y and Mori M: Laparoscopic lymph node
dissection around the inferior mesenteric artery with preservation
of the left colic artery. Surg Endosc. 25:861–866. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dworkin MJ and Allen-Mersh TG: Effect of
inferior mesenteric artery ligation on blood flow in the marginal
artery-dependent sigmoid colon. J Am Coll Surg. 183:357–360.
1996.PubMed/NCBI
|
|
25
|
Seike K, Koda K, Saito N, Oda K, Kosugi C,
Shimizu K and Miyazaki M: Laser Doppler assessment of the influence
of division at the root of the inferior mesenteric artery on
anastomotic blood flow in rectosigmoid cancer surgery. Int J
Colorectal Dis. 22:689–697. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Komen N, Slieker J, de Kort P, de Wilt JH,
van der Harst E, Coene PP, Gosselink MP, Tetteroo G, de Graaf E,
van Beek T, et al: High tie versus low tie in rectal surgery:
Comparison of anastomotic perfusion. Int J Colorectal Dis.
26:1075–1083. 2011. View Article : Google Scholar : PubMed/NCBI
|