Introduction
Dyspnea is one of the complications of thyroid
surgery that may have severe consequences, including death. Common
causes of this complication include compression due to formation of
a hematoma, tracheal collapse, laryngeal edema and bilateral
recurrent laryngeal nerve injury, and they should be taken into
consideration to ensure prevention and/or timely treatment of
dyspnea (1,2). However, rarer causes may delay
diagnosis and lead to a poor outcome. We herein report a case of
dyspnea after thyroid surgery, arising from rapid growth of an
intratracheal lymphoma. The aim of the present study is to alert
physicians to this rare possibility and improve the prognosis for
such patients.
Case report
A 53-year-old male patient was referred to Shanghai
General Hospital with a history of a progressively enlarged mass in
the right neck for 5 years and dyspnea for 1 month. Physical
examination revealed a firm, 10-cm tough mass in the right neck,
which did not move on deglutition, without a vascular murmur.
B-ultrasonography revealed a hypoechoic nodule, measuring 50×90 mm,
in the right lobe of the thyroid gland, with an unclear boundary,
inhomogeneous echo, and a dot-like blood flow signal (Fig. 1A). A computed tomography (CT)
examination revealed bilateral thyroid enlargement, more prominent
on the right side, with narrowing of the trachea and shifting to
the left side due to compression (Fig.
1B). No obvious enlargement of the cervical lymph nodes was
observed by either B-ultrasonography or CT imaging. Laboratory data
revealed normal thyroid function, apart from a high thyroglobulin
antibody titer (2,025 IU/ml; normal range 10–115 IU/ml). Given that
the right thyroid mass caused dyspnea by compressing the trachea, a
right thyroidectomy was performed without preoperative biopsy.
During surgery, a solid mass, sized ~10 cm (Fig. 1C) was identified on the right side of
the thyroid gland, of moderate hardness and with a complete
capsule. The trachea was compressed and shifted to the left,
without tracheomalacia. No obvious adhesions between the tumor and
the trachea were observed during surgery. Intraoperative frozen
section biopsy revealed marked lymphoid hyperplasia in the right
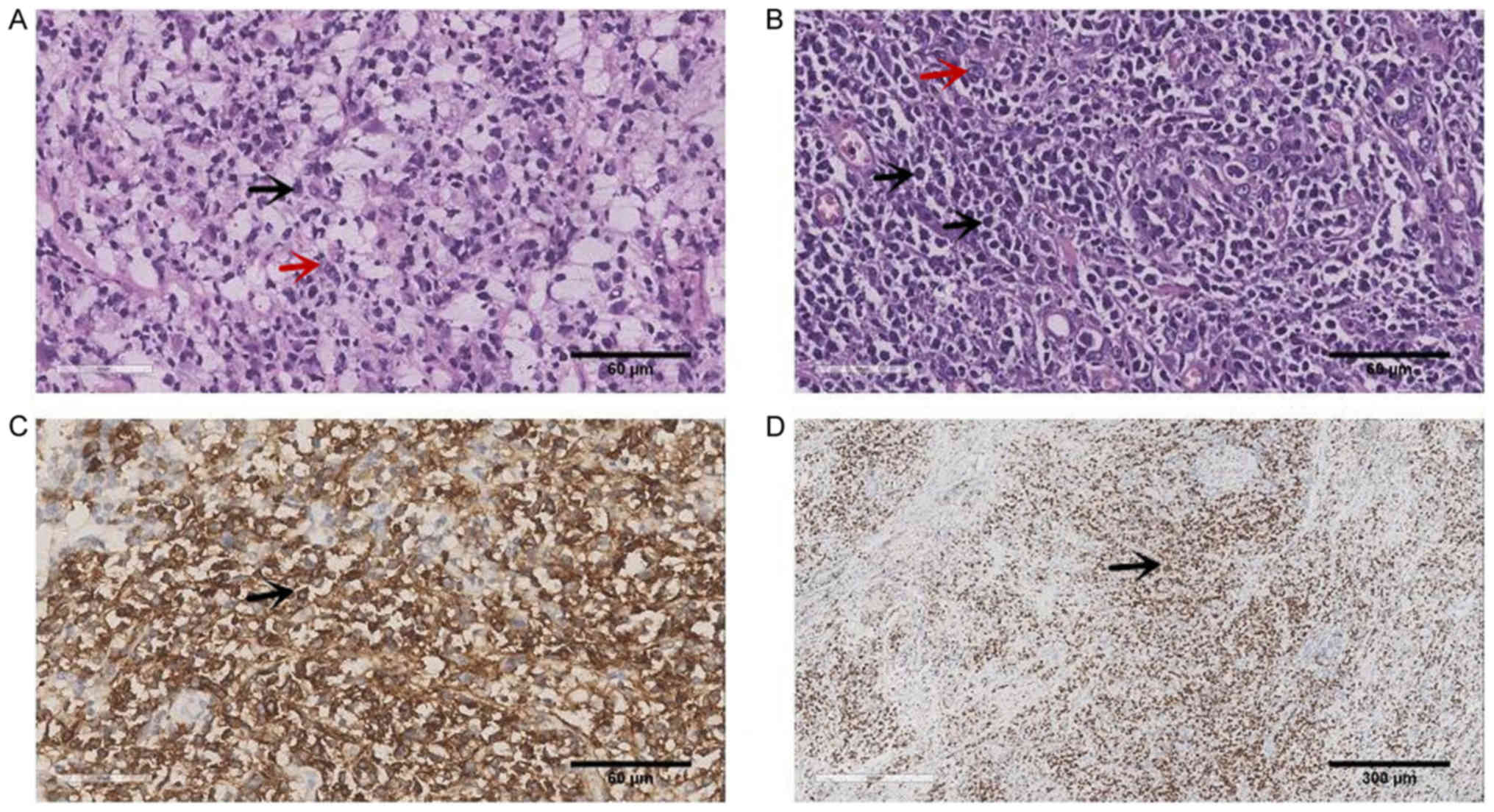
lobe of the thyroid gland (Fig. 2A).
Postoperative pathological examination confirmed non-Hodgkin
diffuse large B-cell lymphoma of the right thyroid (Fig. 2B). The Ki-67 index was 70%,
indicating rapid tumor proliferation (Fig. 2D). Dyspnea was markedly relieved
after surgery, without residual hoarseness, drinking cough,
shakiness or emotional changes. Hospitalization was uneventful and
the patient was discharged on the third postoperative day.
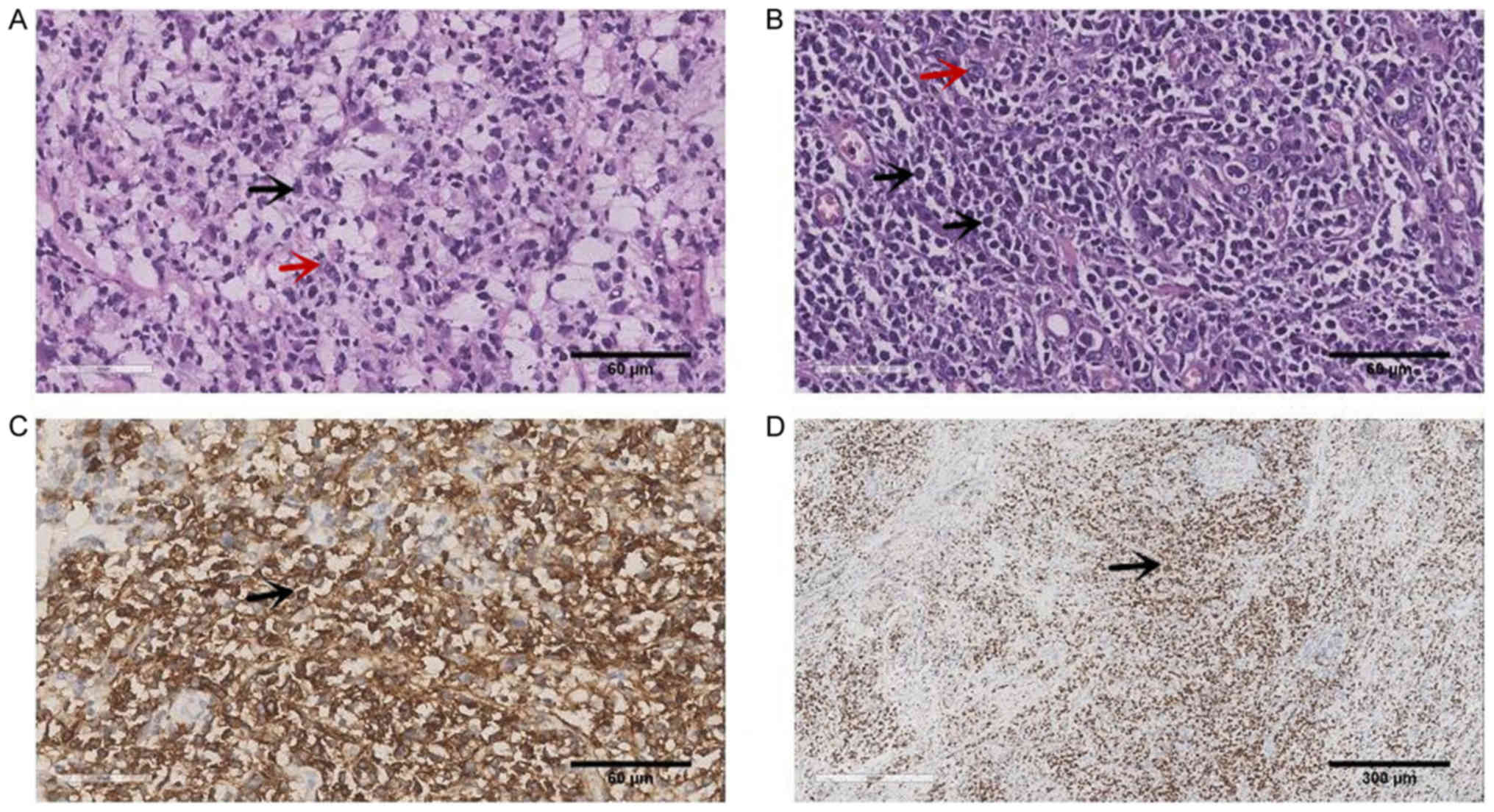 | Figure 2.Histopathological characteristics of
the right thyroid lymphoma. (A) Intraoperative frozen biopsy
examination. (Hematoxylin-eosin staining, magnification, ×400,
black arrow = central cell; red arrow = centroblastic cell). (B)
Postoperative pathological examination. (Hematoxylin-eosin
staining, magnification, ×400, black arrow = central cell; red
arrow = centroblastic cell). (C) Positive immunohistochemical
staining for CD20 (magnification, ×400, black arrow = central
cell). (D) Positive Ki-67 index (70%). (Magnification, ×100, black
arrow = central cell). |
On the 10th postoperative day, the patient suffered
from chest distress and shortness of breath without an obvious
inducing factor, and without significant improvement with rest. On
the 11th day, the dyspnea was aggravated and the patient was
restless, with inspiration difficulty, cyanosis of the lips and
inspiratory three depressions sign. Consequently, the patient
visited the Emergency Department at Shanghai General Hospital.
There was no history of foreign matter aspiration after discharge.
B-ultrasound examination revealed no hematoma in the thyroid
surgery area, uneven rough echo, and normal blood supply in the
residual thyroid gland. The symptoms improved after oxygen
inhalation, and a contrast-enhanced CT of the neck was scheduled.
On the 15th postoperative day, during the CT examination, the
patient suddenly lost consciousness and went into respiratory
arrest, recovering breathing and consciousness only after
tracheotomy and assisted ventilation. An urgent neck CT scan
revealed that the thyroid gland exhibited widespread enlargement
with decreased density. The soft tissue of the subglottic cavity
and upper trachea was notably thickened compared with prior to
surgery, and the airway was markedly narrowed (Fig. 3). The CT scan revealed no laryngeal
edema. Combined with the postoperative pathology, it was concluded
that rapid growth of a rare upper airway lymphoma was the cause of
the postoperative dyspnea.
No evidence of lymphoma involving the bone marrow
was detected by bone marrow aspiration. A positron emission
tomography (PET)/CT examination demonstrated that the left thyroid
gland was diffusely enlarged and the glucose metabolism of the
intratracheal soft tissues was high, raising the suspicion of
lymphoma infiltration. No lymphoma lesions were identified in other
areas of the body. On the 17th day after thyroidectomy, the patient
received chemotherapy with the CHOP regimen combined with rituximab
(R) 8 times; the specific regimen was as follows: R 800 mg +
vindesine 4 mg d1 + cyclophosphamide 1.5 g d1 + epirubicin 120 mg
d1 + prednisone 50 mg b.i.d. d1-5 and mesna 0.4 g. When
chemotherapy was concluded, we attempted to plug the tube, and the
patient experienced no dyspnea. At 6 months after the
thyroidectomy, a tracheal stoma suture was performed, and dyspnea
did not reoccur. After 8 rounds of chemotherapy, PET/CT
re-examination revealed that the residual thyroid glucose
metabolism was relatively decreased, and no abnormalities were
detected in the trachea. On June 3, 2019, 21 months after
thyroidectomy, no lymphoma recurrence in the patient was discovered
by cervical CT or B-ultrasound.
Discussion
Dyspnea is one of the complications of thyroid
surgery that may have severe consequences, including death. Common
causes, including hematoma compression, tracheal collapse,
laryngeal edema, and bilateral recurrent laryngeal nerve injury,
are not to be overlooked, so that dyspnea can be prevented and/or
treated it in a timely manner (1,2).
However, rarer causes may delay the etiological diagnosis, leading
to a poor prognosis. To improve the prognosis of such patients, we
herein report a case of dyspnea arising from a rare cause, namely
the rapid growth of an intratracheal lymphoma after thyroid
surgery.
The patient developed severe dyspnea 2 weeks after
surgery and underwent a tracheostomy for temporary relief.
Identifying the cause of postoperative dyspnea is crucial. The
characteristics of the present case may be summarized as follows:
i) Dyspnea was relieved after the right thyroidectomy, but worsened
to the point of asphyxia 2 weeks later. ii) Dyspnea was relieved
immediately after tracheotomy. iii) Preoperative imaging
examination revealed a soft tissue shadow on the right side of the
trachea. After the surgery, the soft tissue located in the
subglottic cavity and upper trachea was notably thicker compared
with prior to surgery, and the airway was significantly narrowed.
iv) Postoperative pathology suggested thyroid non-Hodgkin B-cell
lymphoma. v) After chemotherapy, from the completion of the
tracheostomy to date, dyspnea did not reoccur, and no abnormalities
were observed on PET/CT. i and ii) Consideration of upper airway
obstruction; i-iii) consideration of upper airway obstruction
caused by neoplasm in the trachea; i-v) consideration of a rapid
growth of rare upper airway lymphoma causing postoperative dyspnea
after thyroidectomy.
First, reviewing the process of diagnosis and
treatment, dyspnea occurred within 2 weeks rather than 48 h of
surgery, no tracheomalacia was found intraoperatively, and
postoperative CT did not reveal laryngeal edema; therefore,
laryngeal edema and tracheal collapse can be excluded as the causes
of dyspnea (3). No apparent
hoarseness was observed in the patient, therefore excluding the
possibility of bilateral recurrent laryngeal nerve injury. In
addition, when postoperative dyspnea occurred, neck ultrasound
examination excluded the possibility of hematoma compression. Thus,
excluding other common causes of postoperative dyspnea, in
combination with the rapid growth of the intratracheal tumor within
2 weeks postoperatively, its sensitivity to chemotherapy and its
characteristic appearance on PET/CT imaging, even without a soft
tissue biopsy, it was concluded clinically that the rapid growth of
the intratracheal lymphoma was the cause of progressive dyspnea
after thyroidectomy.
The patient was admitted to the hospital for
dyspnea, and the etiological diagnosis was compression of the
trachea by a thyroid mass based on medical history, physical and
imaging examinations. Dyspnea was immediately relieved after right
thyroidectomy, which suggested that compression of the trachea by a
large mass on the right lobe of the thyroid gland was at least one
of the causes of preoperative dyspnea. Combined with a rapid
postoperative tumor growth in the trachea and preoperative CT
indicating curved intratracheal soft tissue, intratracheal lymphoma
was also determined to be one of the causes of preoperative
dyspnea. Thus, when preoperative dyspnea occurs and CT indicates
the presence of intratracheal soft tissue, a transbronchial biopsy
should be performed to define the nature of the intratracheal soft
tissue. If postoperative dyspnea occurs, the possibility of rapid
growth of intratracheal soft tissues should also be considered.
Intratracheal tumor growth is a rare cause of airway
stenosis. In addition, primary thyroid non-Hodgkin lymphoma is even
rarer (4), and its clinical and
imaging manifestations lack specificity; therefore, it is easy to
misdiagnose and underdiagnose. Definitive diagnosis mainly relies
on pathological examination, including immunohistochemistry
(CD20+) (5,6). The chief complaint of patients is rapid
enlargement of the mass, which may also invade the trachea. The
patient in the present case was discharged from the hospital
postoperatively following relief of the dyspnea; however, asphyxia
developed rapidly within 2 weeks. Thyroid cancer invading the
trachea may also cause dyspnea, and should be included in the
differential diagnosis. The incidence of differentiated thyroid
cancer invading the larynx and trachea is low, ~13% (7). Causes of dyspnea in differentiated
thyroid cancer cases include the primary tumor or paratracheal
lymph node metastases invading the tracheal adventitia, or the
tumor invading the whole thickness of the tracheal wall, finally
leading to tracheal compression and stenosis. As differentiated
thyroid carcinoma develops slowly and is characterized by a long
disease course, the development of dyspnea is progressive, which
differs significantly from undifferentiated carcinoma. The degree
of malignancy of undifferentiated carcinoma is very high, and
readily invades surrounding tissues and organs. If there is
invasion of the trachea, the tumor will increase rapidly and result
in dyspnea. However, undifferentiated carcinoma is relatively easy
to cure and common among elderly female patients, with fast
progression (8). Upon seeking
medical advice, the majority of the patients have non-specific
symptoms related to varying degrees of dysphagia, dyspnea,
hoarseness or neck pain, and approximately 1/3 of the patients have
involvement of adjacent regional lymph nodes at initial
presentation. Distant metastases also occur frequently; the most
common site of metastasis is the lung, followed by the bone
(9). Most undifferentiated
carcinomas involving the trachea completely destroy the tracheal
wall. Combined with the CT findings, the probability of an
anaplastic thyroid carcinoma, which can be differentiated by
biopsy, was low in our patient.
In conclusion, if common causes are excluded when
postoperative dyspnea occurs, rare causes, such as the possibility
of rapid growth of an intratracheal lymphoma, should be considered.
Furthermore, preoperative needle biopsy of the thyroid mass should
be routinely performed. If the patient is diagnosed with lymphoma
following needle biopsy, chemotherapy may be immediately used
rather than surgery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of materials and data
All the data generated and/or analyzed in the
present study are included in the published manuscript.
Authors' contributions
All the authors have read and approved the final
version of the manuscript for publication. CW drafted and wrote the
manuscript, DD, GQ, XM collected the data, JW supported in the
pathology, MZ gave suggestions, YJ did the thyroidectomy and gave
suggestions, JL conceived the study and contributed to writing the
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient agreed of the publication of this case
details and any associated image with informed consent.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Haugen BR, Alexander EK, Bible KC, Doherty
GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM,
Schlumberger M, et al: 2015 American thyroid association management
guidelines for adult patients with thyroid nodules and
differentiated thyroid cancer: The American thyroid association
guidelines task force on thyroid nodules and differentiated thyroid
cancer. Thyroid. 26:1–133. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rosato L, Avenia N, Bernante P, De Palma
M, Gulino G, Nasi PG, Pelizzo MR and Pezzullo L: Complications of
thyroid surgery: Analysis of a multicentric study on 14,934
patients operated on in Italy over 5 years. World J Surg.
28:271–276. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Goldfarb M, Perry Z, A Hodin R and Parangi
S: Medical and surgical risks in thyroid surgery: Lessons from the
NSQIP. Ann Surg Oncol. 18:3551–3558. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Green LD, Mack L and Pasieka JL:
Anaplastic thyroid cancer and primary thyroid lymphoma: A review of
these rare thyroid malignancies. J Surg Oncol. 94:725–736. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Stein SA and Wartofsky L: Primary thyroid
lymphoma: A clinical review. J Clin Endocrinol Metab. 98:3131–3138.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen C, Yang Y, Jin L, Dong L, Zhang X and
Xiang Y: Primary thyroid T-lymphoblastic lymphoma: A case report
and review of the literature. Int J Clin Exp Pathol. 7:443–450.
2013.PubMed/NCBI
|
|
7
|
Shindo ML, Caruana SM, Kandil E, McCaffrey
JC, Orloff LA, Porterfield JR, Shaha A, Shin J, Terris D and
Randolph G: Management of invasive well-differentiated thyroid
cancer: An American head and neck society consensus statement. AHNS
consensus statement. Head Neck. 36:1379–1390. 2014.PubMed/NCBI
|
|
8
|
Sugitani I, Miyauchi A, Sugino K, Okamoto
T, Yoshida A and Suzuki S: Prognostic factors and treatment
outcomes for anaplastic thyroid carcinoma: ATC research consortium
of Japan cohort study of 677 patients. World J Surg. 36:1247–1254.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Besic N and Gazic B: Sites of metastases
of anaplastic thyroid carcinoma: Autopsy findings in 45 cases from
a single institution. Thyroid. 23:709–713. 2013. View Article : Google Scholar : PubMed/NCBI
|