Introduction
The utilization of robotic systems in surgery has
emerged as an alternative to open and laparoscopic surgery with the
preliminary results being promising to date (1). Initially used in urologic operations
(2) and cholecystectomies (3), the application of the Da Vinci platform
has lately expanded to more challenging cases such as aneurysm
repair (4) and liver (5) and pancreatic resections (6). The advantages of this technology
include better visibility via three-dimensional (3D) imaging,
stable field, enhanced maneuverability due to articulated
instruments and greater precision in the dissection of tissues
(7).
Retroperitoneal sarcomas (RPS) are malignant
neoplasms that account for 10–15% of all soft-tissue tumors
(8). Histological tumor type, grade,
location and extension of resection have been well-documented
prognostic factors for long-term survival. Given the complex nature
of RPS surgery, much emphasis has recently been placed on the
appropriate referral and management of these patients at
specialized centers in order to ensure high quality of surgical
care (9).
Herein, we present the first described case of
robotic resection of a retroperitoneal leiomyosarcoma (RPLM) in a
high-volume center for robotic operations.
Case report
A 72-year-old male was admitted due to progressive
abdominal distension, dull abdominal pain for the last 3 months,
constitutional symptoms and constipation. Physical examination
revealed a slightly distended abdomen and an abdominal mass in
right side which appeared hard and immobile.
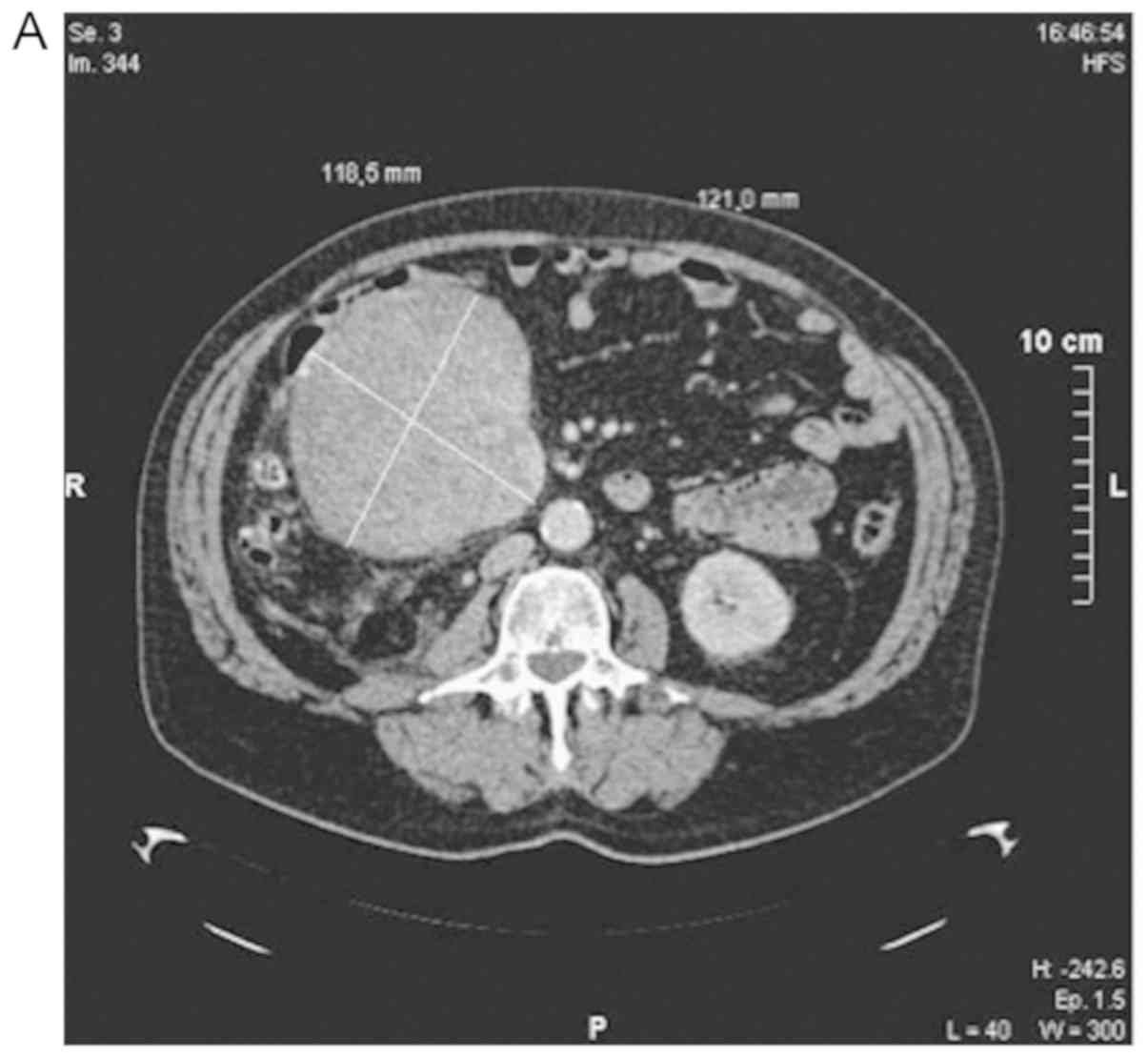
The patient subsequently underwent an abdominal and
pelvic computed tomography (CT) (Fig.
1A) and magnetic resonance imaging (MRI) (Fig. 1B) which revealed a solid
heterogeneous lesion 12,1×11,8×15 cm located from the descending
part of the duodenum and head of the pancreas to transverse
mesocolon and a second smaller lesion 3×2,7 cm infiltrating the
ascending colon. No major vessels were invaded and no liver
metastases were reported.
The patient was scheduled for elective robotic tumor
excision after acknowledging the risks of this challenging
operation and the benefits derived from utilizing the robotic
system in this particular occasion.
Intraoperatively, a gigantic retroperitoneal mass
was revealed compressing the duodenum and the pancreatic groove,
yet did not invade it. The second smaller mass was infiltrating the
ascending colon. The mass was dissected from the duodenum, head of
the pancreas and the right kidney using sharp and blunt dissection
without any breach of tumor capsule. After dissection, the tumor
was extracted completely. An upper midline incision was performed
and a right hemicolectomy was performed (Fig. 2). A frozen section was sent from the
margin of remaining tissue, which was negative for malignancy.
Meticulous hemostasis was performed to ensure no residual bleeding.
The operative time was 7.5 h including the robotic docking time of
30 min. There were no intraoperative or postoperative complications
and the patient was discharged home on the 4th postoperative
day.
The histopathology report described a 19×17,5 cm
retroperitoneal pleomorphic leiomyosarcoma, grade 3, mitotic index
of 10 mitoses per 50 high power fields, CD 117 [C-KIT (−)], CD 68,
Ki67 (MIBI)(+). The surgical margins were free of disease.
Postoperatively the patient was evaluated by medical oncology and
radiation oncology.
Discussion
Patients with RPS are usually diagnosed late, when
the tumor is already of considerable size and close or attached to
critical retroperitoneal structures and organs. This physical
history limits the ability of surgeons to perform wide resections
with clear margins. Importantly, incomplete surgical resection
comprises one of the greatest risk factors locoregional recurrence
and poor survival (10).
The management of bulky intra-abdominal
extra-luminal tumors is challenging due to their close proximity or
diffusion of other structures. The surgical resection of RPLM can
be associated with significant morbidity given that they usually
invade important vascular structures such as the inferior vena cava
(IVC) and tributaries, the duodenum and the ureter (11). The intraoperative 30-day mortality
rate has been reported to be as high as 15% in resections of RPLMs
arising from the IVC (12). However,
a curative intent operation entails a wide resection incorporating
the tumor and all the involved structures (e.g duodenum, colon,
kidney, IVC) in order to achieve adequate resection margins
(13).
Robotic surgery is a minimally invasive approach
that has gained significant popularity over the last decade.
Advantages of this procedure include less intraoperative blood
loss, better visualization, shorter hospital stay, and rapid
patient recovery (14). Importantly,
thanks to the highly articulated instruments and the increased
precision in surgical manipulation, the robotic system is even more
important in cases requiring fine dissection, such as cases
invading the IVC or the aorta (5).
Although in our case the patient recovered rapidly, uneventfully,
after a resection with clear margins, there is a paucity of data on
the oncologic outcomes of such operations in large series; yet
preliminary results in several cancer centers are promising
(15).
In this report, we describe the utilization of the
robotic Da Vinci platform by our experienced team made the
resection of the giant tumor feasible without limiting the
oncologic outcome of the operation. The three-dimensional imaging
system was beneficial in understanding the relationship of the mass
to the ureter, aorta and vena cava as well as colon and small
bowel. Further reports are needed to elucidate the cases that can
take advantage of the robotic technology.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MCM, PGA, MK, PC, FA, AM, DIT, KMK and AI conceived
and designed the present work. MKK, KMK and DM performed the data
analysis. MCM and KMK drafted the manuscript. MCM, PGA, MK, PC, FA,
AM, DIT, AI, MKK, DM and KMK critically revised the manuscript,
provided approval of the final version and agreed to be accountable
for all aspects of the work.
Ethics approval and consent to
participate
The study was conducted according to the Declaration
of Helsinki.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this Case Report/any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hazey JW and Melvin WS: Robot-assisted
general surgery. Semin Laparosc Surg. 11:107–112. 2004.PubMed/NCBI
|
|
2
|
Vince R, Hampton LJ, Vartolomei MD,
Shariat SF, Porpiglia F and Autorino R: Robotic assisted simple
prostatectomy: Recent advances. Curr Opin Urol. 28:309–314. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Angelou A, Skarmoutsos A, Margonis GA,
Moris D, Tsigris C and Pikoulis E: Robotic single port
cholecystectomy: Current data and future perspectives. Minerva
Chir. 72:140–145. 2017.PubMed/NCBI
|
|
4
|
Makris MC, Moris D, Papalouca K, Malietzis
G and Makris GC: The current status of robotic vascular surgery in
the abdominal cavity. Int Angiol. 35:1–7. 2016.PubMed/NCBI
|
|
5
|
Tsilimigras DI, Moris D, Vagios S, Merath
K and Pawlik TM: Safety and oncologic outcomes of robotic liver
resections: A systematic review. J Surg Oncol. 117:1517–1530. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kornaropoulos M, Moris D, Beal EW, Makris
MC, Mitrousias A, Petrou A, Felekouras E, Michalinos A, Vailas M,
Schizas D and Papalampros A: Total robotic pancreaticoduodenectomy:
A systematic review of the literature. Surg Endosc. 31:4382–4392.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Konstantinidis KM, Hiridis S and
Karakitsos D: Robotic-assisted surgical removal of pelvic
schwannoma: A novel approach to a rare variant. Int J Med Robot.
7:55–59. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
von Mehren M, Randall RL, Benjamin RS,
Boles S, Bui MM, Conrad EU III, Ganjoo KN, George S, Gonzalez RJ,
Heslin MJ, et al: Soft tissue sarcoma, version 2.2016, NCCN
clinical practice guidelines in oncology. J Natl Compr Canc Netw.
14:758–786. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Moris D, Petrou A, Papalampros A,
Tsilimigras DI and Felekouras E: Retroperitoneal sarcomas: Does the
center really matter? Surgery. 163:971–972. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stahl JM, Corso CD, Park HS, An Y, Rutter
CE, Han D and Roberts KB: The effect of microscopic margin status
on survival in adult retroperitoneal soft tissue sarcomas. Eur J
Surg Oncol. 43:168–174. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Petrou A, Constantinidou A, Kontos M,
Papalampros A, Moris D, Bakoyiannis C, Neofytou K, Kourounis G and
Felekouras E: Comprehensive surgical treatment as the mainstay of
management in retroperitoneal sarcomas: Retrospective study from
two non-sarcoma specialist centers. Anticancer Res. 37:2025–2031.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Konofaos P, Spartalis E, Moris D,
Athanasiou A, Dimitroulis D, Markakis C, Kostakis ID, Nikiteas N
and Kouraklis G: Challenges in the surgical treatment of
retroperitoneal sarcomas. Indian J Surg. 78:1–5. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Trans-Atlantic RPS Working Group, .
Management of recurrent retroperitoneal sarcoma (RPS) in the adult:
A consensus approach from the trans-atlantic RPS working group. Ann
Surg Oncol. 23:3531–3540. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jayne D, Pigazzi A, Marshall H, Croft J,
Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, et
al: Effect of robotic-assisted vs. conventional laparoscopic
surgery on risk of conversion to open laparotomy among patients
undergoing resection for rectal cancer: The rolarr randomized
clinical trial. JAMA. 318:1569–1580. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Holmer C and Kreis ME: Systematic review
of robotic low anterior resection for rectal cancer. Surg Endosc.
32:569–581. 2018. View Article : Google Scholar : PubMed/NCBI
|