Introduction
Permanent iodine-125 implant brachytherapy (PI) with
or without external beam radiotherapy (EBRT) is a standard,
definitive radiotherapy for localized prostate cancer. As the
intraoperative placement of PI seeds has been refined, delivered
radiation doses have increased, thus maximizing the therapeutic
potential of PI (1). However, the
escalation of local radiation doses can potentially lead to acute
and chronic toxicities in other organs. The SpaceOAR®
System (Augmenix Inc.) is a synthetic polyethylene glycol hydrogel
injected between the prostate and rectum that moves the rectum away
from the prostate to reduce irradiation of the anterior rectal wall
(2).
This is the report of spontaneous healing of rectal
penetration associated with SpaceOAR® hydrogel to be
evaluated by both magnetic resonance imaging (MRI) and
colonofiberoscopy (CF).
Case report
A 63-year-old man with previous sigmoidectomy due to
diverticular perforation presented with a serum prostate-specific
antigen level of 7.17 ng/ml. Although digital rectal examination
(DRE) detected no specific firmness of the prostate gland, magnetic
resonance imaging (MRI) revealed the suspicion of prostate cancer
in the transitional zone of the left lobe. The patient underwent
prostate biopsy, and histological examination of the specimen was
interpreted as multifocal adenocarcinoma of the prostate with
Gleason score 4+3 and to be of intermediate risk. PI with EBRT was
elected for treatment. Due to the history of diverticular
perforation, CF was performed prior to PI and showed no abnormal
findings such as hemorrhoids or rectal tumor. PI was performed with
60 radioactive iodine-125 seeds using the ultrasonography-guided
intraoperative transperineal technique (3). The total prescribed dose was 104 Gy.
Subsequently, SpaceOAR® hydrogel was injected into the
space between the prostate and anterior rectal wall using the same
technique as mentioned above (3).
DRE immediately following the injection revealed intact rectal
mucosa. Twenty-four hours after PI, postimplant computed tomography
(CT) scan showed good seed placements within the prostate and that
the rectal volume receiving 100% of the prescribed dose
(R100) was 0.81 ml.
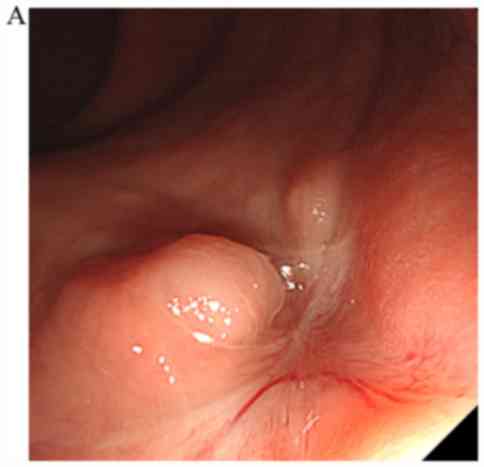
One month after implantation, the patient complained
of repeated incidents of mucous and blood in his stool and
underwent another CF, which confirmed the presence of mucosal
ulceration and necrosis of the anterior rectal wall (Fig. 1). However, the findings did not
suggest proctitis. Although a CT scan revealed air in the space
between the prostate and anterior rectal wall (Fig. 2), the relationship between the rectal
wall and hydrogel was unclear. In contrast, the MRI clearly
indicated penetration of the rectum to the retroperitoneal space
where the hydrogel was injected (Fig.
3). The patient did not complain of constitutional symptoms
including abdominal pain and fever suggesting infection or an
intraperitoneal perforation. Therefore, he decided to be monitored
closely without any treatment. Complete healing was confirmed by
both CF and MRI one month after the diagnosis of penetration
(Fig. 4), therefore he will be
treated by EBRT with less radiation dose for rectum three months
after the healing.
Discussion
The SpaceOAR® System is a safety
technique used to reduce irradiation of the rectum by PI (2). Teh et al reported rectal ulcer
associated with SpaceOAR® hydrogel that was diagnosed by
DRE and CF following spontaneous healing with a low-fiber diet
(4). To the best of our knowledge,
the present report is the first to show spontaneous healing of
SpaceOAR® hydrogel-associated rectal penetration that
was evaluated by MRI and CF. Mechanisms of hydrogel-induced rectal
injury proposed include infection, mechanical injury, ischemic
injury and radiation injury. In this case, no infections and no
radiation proctitis were observed. In fact, the radiation dose to
the rectum was very satisfactory safety and spontaneous healing was
observed without any treatment including antimicrobial agents. In
our hospital, more than grade 3 rectal toxicity evaluated by Common
Terminology Criteria for Adverse Events version 4.0 were only 3
cases of 298 and all cases were treated by PI + EBRT. The incidence
rate of PI-induced rectal toxicity in previous report is 0.33 to
3.1% (5,6), and our incidence rate is 1.0%. Hence,
the other two mechanisms, ischemic injury due to excessive tension
by hydrogel or mechanical injury due to migration of the injection
needle were most likely the same as in a previous report (4). This is the third case of
SpaceOAR® hydrogel in our hospital. It should be
recognized that the hydrogel insertion is a traumatic procedure and
may cause some adverse events including rectal ulcer. Further
clinical study will be needed to elucidate the mechanism of
hydrogel-induced rectal injury.
It was already reported that MRI detects
SpaceOAR® hydrogel more clearly than CT scanning
(7). Teh et al also noted
that routine MRI evaluation of SpaceOAR® hydrogel is not
necessary unless rectal symptoms and signs are present (4). There is no studies demonstrating the
importance of MRI for hydrogel-induced rectal injury, however some
studies reported that MRI plays an important role in the evaluation
of carcinoma induced rectal perforation and depth of perianal
fistulas (8–11). In our patient, MRI helped to diagnose
the exact depth of the ulcer with no perforation and the
relationship between the ulcer and the SpaceOAR®
hydrogel.
In summary, SpaceOAR® hydrogel-associated
rectal penetration could be healed spontaneously without any
treatment only if the patient shows no severe symptoms suggesting
rectal perforation. In such a case, MRI may be considered to
evaluate exact depth of penetration same as rectal perforation by
rectal cancer or anal fistula (8–11).
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
KI and KM acquired the data and wrote the
manuscript. TK, KN, MN and TK acquired the data and contributed
clinical advice. HT and MM interpreted the radiographic data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of Gifu University (approval no. 2018-169).
Patient consent for publication
The patient provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kao J, Cesaretti JA, Stone NN and Stock
RG: Update on prostate brachytherapy: Long-term outcomes and
treatment-related morbidity. Curr Urol Rep. 12:237–242. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Karsh LI, Gross ET, Pieczonka CM, Aliotta
PJ, Skomra CJ, Ponsky LE, Nieh PT, Han M, Hamstra DA and Shore ND:
Absorbable Hydrogel spacer use in prostate radiotherapy: A
comprehensive review of phase 3 clinical trial published data.
Urology. 115:39–44. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ohashi T, Yorozu A, Toya K, Saito S, Momma
T, Nagata H, Kosugi M, Shigematsu N and Kubo A: Comparison of
intraoperative ultrasound with postimplant computed
tomography-dosimetric values at Day 1 and Day 30 after prostate
brachytherapy. Brachytherapy. 6:246–253. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Teh AY, Ko HT, Barr G and Woo HH: Rectal
ulcer associated with SpaceOAR hydrogel insertion during prostate
brachytherapy. BMJ Case Rep. 2014(pii): bcr20142069312014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Buckstein M, Carpenter TJ, Stone NN and
Stock RG: Long-term outcomes and toxicity in patients treated with
brachytherapy for prostate adenocarcinoma younger than 60 years of
age at treatment with minimum 10 years of follow-up. Urology.
81:364–368. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Price JG, Stone NN and Stock RG:
Predictive factors and management of rectal bleeding side effects
following prostate cancer brachytherapy. Int J Radiat Oncol Biol
Phys. 86:842–847. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sheridan AD, Nath SK, Huber S, Rosasco S,
Weinreb JC and Israel GM: Role of MRI in the use of an absorbable
hydrogel spacer in men undergoing radiation therapy for prostate
cancer: What the radiologist needs to know. AJR Am J Roentgenol.
209:797–799. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tapan U, Ozbayrak M and Tatli S: MRI in
local staging of rectal cancer: An update. Diagn Interv Radiol.
20:390–398. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Khera PS, Badawi HA and Afifi AH: MRI in
perianal fistulae. Indian J Radiol Imaging. 20:53–57. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Spencer JA, Chapple K, Wilson D, Ward J,
Windsor AC and Ambrose NS: Outcome after surgery for perianal
fistula: Predictive value of MR imaging. AJR Am J Roentgenol.
171:403–406. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
de Miguel Criado J, del Salto LG, Rivas
PF, del Hoyo LF, Velasco LG, de las Vacas MI, Marco Sanz AG,
Paradela MM and Moreno EF: MR imaging evaluation of perianal
fistulas: Spectrum of imaging features. Radiographics. 32:175–194.
2012. View Article : Google Scholar : PubMed/NCBI
|