Introduction
Glioblastoma (GBM) is the most common primary glial
malignancy (1). Despite its
prevalence, and the resultant abundance of organized clinical
investigation over several decades, GBM remains a challenging
therapeutic entity from its initial diagnosis to its nearly
inevitable recurrence. Multiple treatment modalities are under
active investigation, offering limited promise to improving overall
survival in this patient population (2). Drugs treating this disease through
novel mechanisms are urgently needed.
Recently, proteasome inhibitors have been developed
as an additional treatment option for recurrent and, given their
measured success, newly diagnosed multiple myeloma. The proteasome
is responsible for degrading damaged and ubiquinated proteins
integral to normal cellular functioning (3). Selectively preventing cellular
maintenance in relatively rapidly dividing neoplastic cells has
proven an effective strategy. Bortezomib, an intravenous agent of
this drug class, has been approved in the US for treatment of
multiple myeloma since 2003(4).
Initial studies of bortezomib in mouse models demonstrated a lack
of penetration of the blood brain barrier (5). Despite this, the effective
anti-neoplastic characteristics of proteasome inhibitors were
recognized, and bortezomib has since been investigated in GBM with
good reported response (6-9).
Ixazomib (MLN2238) is a second generation, orally
administered proteasome inhibitor. Following the trail blazed by
the investigation of bortezomib, ixazomib has recently proven
effective against multiple myeloma, offering the practical
advantage of its oral bioavailability (10-12).
In murine xenograft models of lymphoma, ixazomib was found to be a
potent and reversible proteasome inhibitor. These murine xenograft
model investigations explored the pharmacokinetic profiles of these
two drugs and found them comparable. Additionally, ixazomib
administration resulted in more tumor volume improvement compared
with bortezomib (13). It was
further demonstrated to have effect against human multiple myeloma
cell lines with in vitro and in vivo studies
(14-16).
Despite its promise, ixazomib activity against glioblastoma was not
tested during its development.
This phase 0 clinical trial utilized a new assay to
identify and quantify ixazomib after pre-operative administration
in human brain specimens during recurrent glioblastoma
resection.
The primary objective of this clinical trial was to
establish whether ixazomib reached glioblastoma tissue after its
preoperative oral administration. To this end, we sought to
quantify brain tissue concentration of the agent. We also sought to
establish blood and plasma concentrations of this orally
administered agent throughout the course of tumor resection. A
secondary objective was to evaluate the safety and tolerability of
ixazomib after single dose administration in glioblastoma
patients.
Materials and methods
Study design and sample size
selection
A purposely small number of patients was chosen to
assess this new assay of ixazomib in brain tumor tissue in view of
the invasive steps (intracranial tumor sampling via craniotomy)
necessary to obtain the samples. Specifically, it was determined
that only three subjects would be enrolled in this phase 0 study to
balance safety against analyzing enough tumor samples to meet the
objective of the study: a yes or no answer of whether ixazomib
reaches the brain tumor tissue after oral administration.
Summary of enrollment criteria and
clinical management
Enrolled patients had recurrent or progressive
glioblastoma for which surgical resection was indicated. The study
was first approved by the Emory University Institutional Review
Board (IRB00083003). The trial was explained to each patient and
this was documented in their medical record. They then signed the
informed consent after being given an opportunity to ask questions
about its risks and benefits to them. They each had a Karnofsky
performance status of ≥60 (ECOG 2). We studied 3 patients with
recurrent glioblastoma after administration of oral ixazomib
citrate (MLN 9708) at a fixed 4.0 mg dose within a 3-h preoperative
window. The authors believed that three patients were enough to
determine if measurable delivery was feasible and account for
intertumor heterogeneity. To account for intratumor heterogeneity,
three samples from different portions of the tumor were obtained in
patient 3. Their location was described in the operative
report.
MLN2238 analysis
The method of qualification was performed under the
general bioanalytic guidelines for reproducibility that are
utilized internally at Covance Laboratories. This is proprietary.
There is not a currently accepted standard method of qualification
to compare this method against.
Blood samples were taken from each patient at time
of incision, tumor sampling, and closure. Brain tumor samples were
collected during tumor resection. These samples were then used to
measure plasma and brain tumor tissue concentration of MLN2238, the
biologically active boronic form of ixazomib.
Plasma sample preparation
Plasma samples (200 µl) were aliquoted into a
96-well plate. 50.0 µl of working ixazomib solution were added to
wells. To each well, 50.0 µl of 0.5 N hydrochloric acid was added
and vortexmixed for 2 min. 800 µl of methyl tert-butyl ether was
added to each well. Samples were vortex-mixed for 3 min and
centrifuged for 10 min at 3,700 rpm. Supernatant (600 µl) was then
transferred to a clean 96-well plate and dried to completion under
a stream of nitrogen set at 40˚C. The dried sample extracts were
then reconstituted in 150 µl of (25:75:0.1)
acetonitrile:water:formic acid. The plate was vortex-mixed for 2
min prior to injection onto an equilibrated LC-MS/MS
instrument.
Brain sample preparation
Brain homogenate was prepared using a 4X dilution of
tissue into reverse osmosis water and homogenized using an Omni
Inc. BeadRuptor homogenizer set at 5.0 m/sec. Working calibration
standards were created by dilution of the intermediate solutions
into brain homogenate at final concentrations of 0.500, 1.00, 5.00,
25.0, 50.0, 100, 250, 450 and 500 ng/g in tissue.
Brain homogenate samples (200 µl) were added to
flexi tier glass inserts containing 50.0 µl of working IS solution.
To each insert, 50.0 µl of 0.5 N hydrochloric acid was added and
vortexmixed for 2 min. Methyl tert-butyl ether (800 µl) was added
to each insert to quench the brain homogenate samples. Samples were
vortex-mixed for 3 min and centrifuged for 10 min at 3,700 rpm.
Supernatant (500 µl) was then transferred to a clean 96-well plate
and dried to completion under a stream of nitrogen set at 40˚C. The
dried sample extracts were then reconstituted in 100 µl of
(25:75:0.1) acetonitrile:water:formic acid. The plate was
vortexmixed for 2 min prior to injection onto an equilibrated
LC-MS/MS instrument.
Plasma and brain sample analysis and
instrumentation
The samples were analyzed with a new and unique via
liquid chromatography tandem mass spectrometry assay. This expands
on a prior, and more limited assay method, described by Gupta et
al (17). For this new assay a
qualified curve range of 0.500-500 ng/ml for plasma and 0.500-500
ng/g for brain homogenate was utilized. To accomplish the stock
standard solutions of Ixazomib and
[13C9]-Ixazomib (IS) were prepared separately
in a (55:45:0.1) mixture of acetonitrile:water:formic acid at a
concentration of 0.500 mg/ml and stored at -20˚C. Intermediate
standard solutions of Ixazomib were prepared by dilution of stock
solution at concentrations of 10.0, 20.0, 100, 500, 1,000, 2,000,
5,000, 9,000 and 10,000 ng/m; and stored at -20˚C. Intermediate
quality control (QC) solutions were prepared by dilution of stock
solution at concentrations of 30.0, 800, 4,000 and 8,000 ng/ml and
stored at -20˚C. A working IS solution was prepared from stock into
(100:1) acetonitrile:formic acid at a concentration of 100 ng/ml.
Working calibration standards were created by dilution of the
intermediate solutions into plasma at final concentrations of
0.500, 1.00, 5.00, 25.0, 50.0, 100, 250, 450 and 500 ng/ml.
Similarly, the working QC samples were prepared at concentrations
of 1.50, 40.0, 200 and 400 ng/ml in plasma. Each calibration curve
point was generated by diluting 250 µl of each intermediate
standard HPLC analysis involved a gradient acquisition of 1.5 min
using a C18 column in tandem with triple-quad mass spectrometer in
ESI+ mode. Additional details for the plasma and brain
assay are summarized in Tables I
and II.
 | Table IPlasma assay summary. |
Table I
Plasma assay summary.
| Laboratory
information | Description |
|---|
| Analyte | MLN2238 |
| Species | Human |
| Analytical
matrix | K2EDTA
Plasma |
| ISTD |
[13C9]-MLN2238 |
| Qualified method
(non-GLP) | Covance 8383722 |
| Qualified range | 0.500-500 ng/ml |
| LLOQ | 0.500 ng/ml |
| QC levels | 1.50, 40.0, 200 and
400 ng/ml |
| Analytical
technique/method of detection | Liquid-liquid
extraction/ LC-MS/MS |
| Sample volume | 200 µl |
| Calibration
model | Linear
regression |
| Weighting factor | 1/x2 |
| R2 | 0.9885 |
| Accuracy and
precision | Requirements of ≥75%
of STDS within ±25% (±30% LLOQ) fulfilled; Requirements of ≥67% of
QCs within ±25% fulfilled |
| Carryover | Passes acceptance
criteria of <LLOQ |
 | Table IIBrain assay summary. |
Table II
Brain assay summary.
| Laboratory
information | Description |
|---|
| Analyte | MLN2238 |
| Species | Human |
| Analytical
matrix | Brain |
| ISTD |
[13C9]-MLN2238 |
| Qualified method
(non-GLP) | Covance 8383722 |
| Qualified range | 1.00-500 ng/g |
| LLOQ | 1.00 ng/g |
| QC levels | 3.00, 40.0, 200 and
400 ng/g |
| Analytical
technique/ | Liquid-liquid
extraction/ |
| method of
detection | LC-MS/MS |
| Sample volume | 200 µl |
| Calibration
model | Linear
regression |
| Weighting factor | 1/x2 |
| R2 | 0.9618 |
| Accuracy and
precision | Requirements of ≥75%
of STDS within ±30% fulfilled; Requirements of ≥67% of QCs within
±30% fulfilled |
| Carryover | Passes acceptance
criteria of <LLOQ |
Safety was assessed with routine postoperative
laboratory, vital sign, neurologic exam, and imaging studies
through the day of surgery to staple or suture removal. This data
was collected and any adverse events graded and their relationship
to ixazomib administration determined.
Results
Drug concentrations found in
plasma
Basic patient descriptive characteristics are
reviewed in Table III. Patient 1
had plasma concentrations of ixazomib averaging 26.2, 21.8, and
15.3 ng/ml at incision, tumor sampling, and closure respectively
(Fig. 1).
 | Table IIIDescriptive patient information. |
Table III
Descriptive patient information.
| Patient | Age, years | Sex | Ethnicity | KPS | Tumor location |
|---|
| 1 | 46 | Male | Black | 60 | Right frontal
lobe |
| 2 | 36 | Female | White | 70 | Left parietal
lobe |
| 3 | 69 | Male | White | 70 | Right frontal
lobe |
Patient 2 had the same interval plasma concentration
measurements drawn. These averaged 19.0, 18.0, and 8.93 ng/ml at
incision, tumor sampling, and closure (Fig. 2).
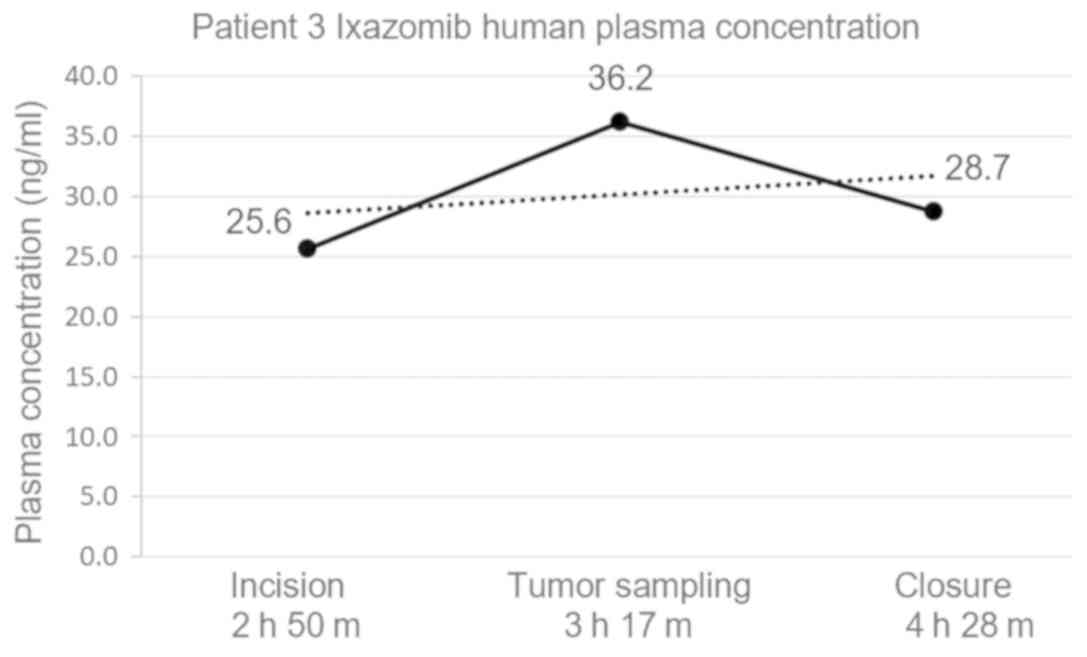
Patient 3 had the same interval measurements of
ixazomib plasma concentration drawn. These averaged 25.6, 36.2, and
28.7 ng/ml at incision, tumor sampling, and closure (Fig. 3).
The relative plasma concentrations between the 3
patients relative to the drugs preoperative administration were
analyzed (Fig. 4).
Drug concentrations found in brain
tissue
Patient 1 had brain tissue concentration of ixazomib
of 7.88 ng/g. Patient 2 had brain tissue ixazomib concentration of
2.03 ng/g.
Patient 3 had 3 separate brain tissue samples taken
from different regions of the tumor to account for intratumor
variability. Tissue sample no. 1 had an ixazomib concentration of
4.17 ng/g. Tissue sample no. 2 had an ixazomib concentration of
2.70 ng/g. Tissue sample no. 3 had an ixazomib concentration of
3.25 ng/g. The average ixazomib concentration between these 3
samples in patient 3 was 3.37 ng/g (Table IV).
 | Table IVBrain tissue concentrations of
ixazomib in tumor samples. |
Table IV
Brain tissue concentrations of
ixazomib in tumor samples.
| Patient no. | Brain tissue ixazomib
concentration, ng/g |
|---|
| Patient 1 | 7.88 |
| Patient 2 | 2.03 |
| Patient 3 | 3.37 (average) |
| Tissue sample 1 | 4.17 |
| Tissue sample 2 | 2.70 |
| Tissue sample 3 | 3.25 |
Adverse events reporting
We used the National Cancer Institute (NCI) Common
Terminology Criteria for Adverse Events (NCI CTCAE) to stratify any
adverse patient response to ixazomib. There were no clinically
relevant adverse events as a result of ixazomib administration.
Patient 1 experienced grade 1 anemia,
thrombocytopenia, an elevated alanine aminotransferase level,
confusion and dysarthria. All of these were managed expectantly
without medication administration. They also experienced grade 2
headache and nausea, which were treated with medication as deemed
appropriate by the evaluating physician. Patient 2 experienced
grade 1 proteinuria, anemia, an elevated lipase level, confusion,
and lethargy. None of these required treatment. They also
experienced grade 2 oral mucosal thrush, which was treated with
medication deemed appropriate by the evaluating physician. Patient
3 experienced grade 1 fatigue, early satiety, generalized weakness.
None of these merited treatment. This patient also experienced
grade 2 hyperthyroidism, which was treated with the appropriate
medication by the evaluating physician.
Discussion
As further drug classes demonstrate their
anti-neoplastic potential, it is imperative that we utilize the
scientific and administrative groundwork already accomplished to
evaluate their efficacy in devastating diseases such as GBM. This
small phase 0 clinical trial establishes that ixazomib reaches
brain tumor tissue after simple fixed dose pre-operative
administration. There are measureable plasma concentrations
commensurate with previously established time and dose-dependent
pharmacokinetic profiles in both mice and humans with multiple
myeloma. There were no serious adverse effects related to its
administration. Dosing was simple. The oral administration offers
the advantage of convenience in a patient population beleaguered
with frequent medical office visits and medication administration.
Better understanding of what comprises therapeutic drug
concentrations and the extent of this efficacy on tumors will
require further investigation in future clinical trials.
This clinical trial has several important
limitations. Investigational drugs must be deliberately and
conservatively evaluated, accentuating some of these limitations
(17,18). Obviously, our results are tempered
by the trial's small sample size and absence of patient follow up
data. Dose escalation studies in the future may reveal problems
with safety or tolerability. While the phase I and II trials of
ixazomib for multiple myeloma have been promising, there is no such
guarantee with GBM. While ixazomib was present in the tumor tissue
of our patients, we do not know if it could reach tumor in
locations where the blood brain barrier is intact or if it can do
so in a meaningful dose for tumor control. Also, normal brain
samples from the three subjects were not obtained. The brain within
centimeters of glioblastomas is known to be infiltrated with tumor
and would not be representative of normal (19,20).
Taking samples of normal brain beyond those would not be feasible
as surgical working space is not extended beyond that needed for
the tumor surgery, and more importantly would deemed unethical in
the eyes of the investigators. The blood and tissue assay used here
are unique and we do not plan to submit for FDA review until more
patient data is obtained and there are plans to use it as a
standard diagnostic test.
Additionally, all 3 of our patients had recurrent
glioblastoma. The development of recurrence with this tumor is
associated with a poor prognosis with mean survival of 20-30 weeks
with treatment (21). It is
possible that their altered post-treatment anatomy and physiology
made their blood brain barriers more permeable to ixazomib
penetration. A newly diagnosed glioblastoma may be more resilient
to treatment. We anticipate a future phase I analysis comparing
ixazomib alone with ixazomib and a cytotoxic agent such as
temozolomide.
In conclusion, orally administered ixazomib reaches
brain tumor tissue. It reaches blood concentrations in human
recurrent GBM patients similar to previously established
pharmacokinetic profiles in mice and humans with multiple myeloma.
Its therapeutic potential needs to be determined with further
analysis.
Acknowledgements
Not applicable.
Funding
Clinical trial support was provided by Takeda,
Inc.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JO designed the experiments. RP and JO implemented
the experiments. JQ, EH, DA, GB, LG and JO analyzed and interpreted
the data. JQ, RP, EH, DA, GB, LG and JO drafted and revised the
manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All procedures performed in studies involving human
participants were in accordance with the ethical standards of the
institutional and/or national research committee and with the 1964
Helsinki declaration and its later amendments or comparable ethical
standards. Informed consent for collection of the data was obtained
from all individual participants included in the study.
Patient consent for publication
Informed consent for publication of the results was
obtained from all individual participants included in the present
study.
Competing interests
JO receives research grant support and clinical
trial support from Takeda, Inc. and the National Cancer Institute.
JO serves on the editorial board of the American Cancer
Society.
References
|
1
|
Porter KR, McCarthy BJ, Freels S, Kim Y
and Davis FG: Prevalence estimates for primary brain tumors in the
United States by age, gender, behavior, and histology. Neuro Oncol.
12:520–527. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Omuro A and DeAngelis LM: Glioblastoma and
other malignant gliomas: A clinical review. JAMA. 310:1842–1850.
2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Voss P and Grune T: The nuclear proteasome
and the degradation of oxidatively damaged proteins. Amino Acids.
32:527–534. 2007.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bladé J, Cibeira MT and Rosiñol L:
Bortezomib: A valuable new antineoplastic strategy in multiple
myeloma. Acta Oncol. 44:440–448. 2005.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Adams J, Palombella VJ, Sausville EA,
Johnson J, Destree A, Lazarus DD, Maas J, Pien CS, Prakash S and
Elliott PJ: Proteasome inhibitors: A novel class of potent and
effective antitumor agents. Cancer Res. 59:2615–22. 1999.PubMed/NCBI
|
|
6
|
Yin D, Zhou H, Kumagai T, Liu G, Ong JM,
Black KL and Koeffler HP: Proteasome inhibitor PS-341 causes cell
growth arrest and apoptosis in human glioblastoma multiforme (GBM).
Oncogene. 24:344–354. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kubicek GJ, Werner-Wasik M, Machtay M,
Mallon G, Myers T, Ramirez M, Andrews D, Curran WJ Jr and Dicker
AP: Phase I trial using proteasome inhibitor bortezomib and
concurrent temozolomide and radiotherapy for central nervous system
malignancies. Int J Radiat Oncol Biol Phys. 74:433–439.
2009.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kong XT, Nguyen NT, Choi YJ, Zhang G,
Nguyen HN, Filka E, Green S, Yong WH, Liau LM, Green RM, et al:
Phase 2 study of bortezomib combined with temozolomide and regional
radiation therapy for upfront treatment of patients with newly
diagnosed glioblastoma multiforme: Safety and efficacy assessment.
Int J Radiat Oncol Biol Phys. 100:1195–1203. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Styczynski J, Olszewska-Slonina D,
Kolodziej B, Napieraj M and Wysocki M: Activity of bortezomib in
glioblastoma. Anticancer Res. 26:4499–4503. 2006.PubMed/NCBI
|
|
10
|
Kumar SK, Berdeja JG, Niesvizky R, Lonial
S, Laubach JP, Hamadani M, Stewart AK, Hari P, Roy V, Vescio R, et
al: Safety and tolerability of ixazomib, an oral proteasome
inhibitor, in combination with lenalidomide and dexamethasone in
patients with previously untreated multiple myeloma: An open-label
phase 1/2 study. Lancet Oncol. 15:1503–1512. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kumar SK, Bensinger WI, Zimmerman TM,
Reeder CB, Berenson JR, Berg D, Hui AM, Gupta N, Di Bacco A, Yu J,
et al: Phase 1 study of weekly dosing with the investigational oral
proteasome inhibitor ixazomib in relapsed/refractory multiple
myeloma. Blood. 124:1047–1055. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Richardson PG, Baz R, Wang M, Jakubowiak
AJ, Laubach JP, Harvey RD, Talpaz M, Berg D, Liu G, Yu J, et al:
Phase 1 study of twice-weekly ixazomib, an oral proteasome
inhibitor, in relapsed/refractory multiple myeloma patients. Blood.
124:1038–1046. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kupperman E, Lee EC, Cao Y, Bannerman B,
Fitzgerald M, Berger A, Yu J, Yang Y, Hales P, Bruzzese F, et al:
Evaluation of the proteasome inhibitor MLN9708 in preclinical
models of human cancer. Cancer Res. 70:1970–1980. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chauhan D, Tian Z, Zhou B, Kuhn D,
Orlowski R, Raje N, Richardson P and Anderson KC: In vitro and in
vivo selective antitumor activity of a novel orally bioavailable
proteasome inhibitor MLN9708 against multiple myeloma cells. Clin
Cancer Res. 17:5311–5321. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gupta N, Diderichsen PM, Hanley MJ, Berg
D, van de Velde H, Harvey RD and Venkatakrishnan K: Population
pharmacokinetic analysis of ixazomib, an oral proteasome inhibitor,
including data from the phase III TOURMALINE-MM1 study to inform
labelling. Clin Pharmacokinet. 6L:1355–1368. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Gentile M, Offidani M, Vigna E, Corvatta
L, Recchia AG, Morabito L, Morabito F and Gentili S: Ixazomib for
the treatment of multiple myeloma. Expert Opin Investig Drugs.
24:1287–1298. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gupta N, Zhao Y, Hui AM, Esseltine DL and
Venkatakrishnan K: Switching from body surface area-based to fixed
dosing for the investigational proteasome inhibitor ixazomib: A
population pharmacokinetic analysis. Br J Clin Pharmacol.
79:789–800. 2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kummar S, Rubinstein L, Kinders R,
Parchment RE, Gutierrez ME, Murgo AJ, Ji J, Mroczkowski B, Pickeral
OK, Simpson M, et al: Phase 0 clinical trials: Conceptions and
misconceptions. Cancer J. 14:133–137. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Burger PC, Heinz ER, Shibata T and
Kleihues P: Topographic anatomy and CT correlations in the
untreated glioblastoma multiforme. J Neurosurg. 68:698–704.
1988.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Louis DN, Ohgaki H, Wiestler OD and
Cavenee WK (eds.): WHO Classification of Tumours of the Central
Nervous System. (Revised 4th edition), IARC, Lyon, 2016.
|
|
21
|
Wu W, Lamborn KR, Buckner JC, Novotny PJ,
Chang SM, O'Fallon JR, Jaeckle KA and Prados MD: Joint NCCTG and
NABTC prognostic factors analysis for high-grade recurrent glioma.
Neuro Oncol. 12:164–172. 2010.PubMed/NCBI View Article : Google Scholar
|