Introduction
The brain is a common metastatic site for non-small
cell lung cancer (NSCLC). In patients surgically treated for
early-stage (stage I/II) NSCLC, the 5-year risk of developing brain
metastasis (BM) is 10% (1). In
advanced-stage NSCLC (stage IIIB/IV), BM occurs in 36% of the
patients throughout the course of their disease (2). BM in patients with NSCLC is usually
associated with a poor prognosis, with a median survival time (MST)
of 7 months (3).
Although whole brain radiation therapy (WBRT) has
historically been performed as a standard therapy for multiple BMs
(4), cognitive dysfunction may
develop as a side effect of WBRT (5). At present, not only WBRT, but also
stereotactic radiosurgery (SRS), surgical resection, drug therapy,
and combinations of these modalities, have been performed according
to the clinical background of each patient (5-11).
We herein present a rare case of a patient with
multiple BMs from NSCLC who was treated using a combination of
resection and SRS and has remained relapse-free for >13 years
without cognitive dysfunction.
Case report
In October 2005, a 55-year-old Japanese man visited
the Department of Neurosurgery of Tokyo Dental College Ichikawa
General Hospital (Ichikawa, Japan) with complaints of motor aphasia
and fatigue. Enhanced brain MRI examination revealed multiple brain
tumors (Fig. 1A). A 3-cm tumor was
identified in the left frontal lobe, with an enhancement effect in
the periphery, accompanied by edema of the surrounding tissue. A
nodule 4 mm in diameter was observed in the right parietal lobe.
The Eastern Cooperative Oncology Group performance status (ECOG PS)
score was 1, and the Karnofsky performance score (KPS) was 70. The
patient had a history of lung cancer, hypertension and smoking (35
pack-years), and was working as a civil service employee.
According to information obtained from the previous
doctor, the patient had undergone lung surgery 3 months before
visiting our hospital (July 2005). The primary lung tumor was 4 cm
in diameter and was located in segment 2 of the right upper lobe
(Fig. 2A); the carcinoembryonic
antigen (CEA) level was 12.8 ng/ml (reference range, 0-5 ng/ml). A
right upper lobectomy with lymph node dissection was performed, and
the tumor was diagnosed as lung adenocarcinoma and pathologically
classified as T2N2Mx according to the 6th edition of the TNM
classification (12). The patient
declined adjuvant chemotherapy.
It was considered likely that these brain tumors
were metastases from the NSCLC. Brain MRI, which is usually
performed, had not been performed prior to lung surgery; thus, it
was unknown whether any BMs existed prior to surgery.
To reduce the risk of cognitive dysfunction as a
side effect of WBRT, surgical resection of the 3-cm brain tumor in
the left frontal lobe was performed, while the remaining small
nodule was treated with SRS.
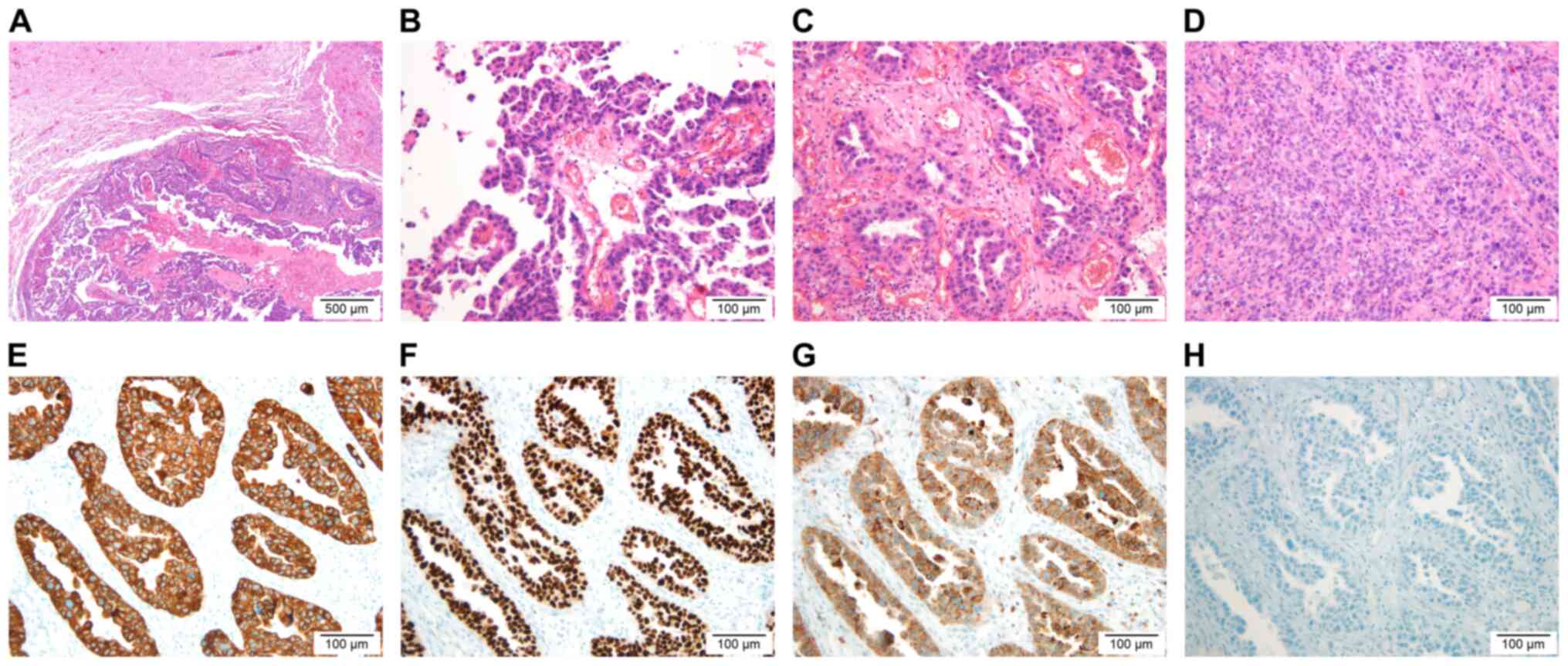
In December 2005, the left frontal lobe tumor was
completely removed at our hospital. On histological examination,
the brain tumor was an adenocarcinoma exhibiting papillary, acinar
and solid growth patterns (Fig.
3A-D), while the primary lung tumor had been diagnosed as an
adenocarcinoma exhibiting acinar and solid growth patterns based on
information obtained from the previous doctor, and no neoplastic
lesions were found in organs other than the lungs. Hence, the brain
tumors were diagnosed as metastatic lesions from lung cancer.
Furthermore, immunohistochemistry (IHC) performed later revealed
that the tumor cells were positive for cytokeratin (CK)7, thyroid
transcription factor-1 (TTF-1) and napsin A, whereas CK20 was
negative (Fig. 3E-H), which were
findings characteristic of metastasis from lung adenocarcinoma. The
brain tumor did not harbor any mutations in the EGFR
gene.
In January 2006, the 4-mm nodule in the right
parietal lobe increased to a diameter of 8.5 mm, and a second new
8.5-mm nodule was observed in the same lobe (Fig. 1B). An 8-mm nodule was also observed
in the left occipital lobe (Fig.
1C). SRS using Leksell Gamma Knife was performed for the three
BMs at a peripheral dose of 20 Gy (50%).
At 9 months after SRS, enhanced brain MRI revealed a
new 3.5-mm nodule in the left frontal lobe (Fig. 1D), and SRS was performed again in
January 2007. The patient did not wish to receive the subsequent
systemic chemotherapy.
In December 2020, enhanced brain MRI (Fig. 1E-G), enhanced chest and abdominal CT
(Fig. 2B) and bone scintigraphy
(data not shown) did not show any recurrence. The patient's CEA
level in March 2021 was within the normal range (4.2 ng/ml). His
ECOG PS score was 0, his KPS was 100 and his mini-mental status
examination (MMSE) score was 30. The patient was considered to be
clinically cured, as he had remained relapse-free for >13 years
since the last SRS treatment.
Discussion
Lutterbach et al (13) retrospectively analyzed patients with
NSCLC who had single or multiple BMs and reported a survival rate
of 2.6% at 3 years and <1% at 5 years. There have been few
reports of long-term survival (>10 years) in patients with NSCLC
who had multiple BMs. Kotecha et al (14) reviewed the records of 1,953 patients
who underwent treatment for BMs; among those, only two with
multiple BMs from NSCLC survived for ≥10 years: One survived for
10.1 years and died due to systemic disease; however, there was no
information regarding neurological symptoms after treatment. The
other patient survived for 15.3 years, and the cause of death was
unknown. The KPS after treatment was 50, and the patient required
the assistance of a wheelchair. In the present case, the patient
suffered from NSCLC with multiple BMs and has remained relapse-free
for >13 years, with no neurological dysfunction, including
cognitive deficit.
The questions that remain in the rare clinically
cured cases, such as the present case, are whether the brain lesion
was actually a tumor and whether it was a BM from lung cancer. In
patients with NSCLC who exhibit metastases on enhanced brain MRI,
if there are no concerns regarding the diagnosis, it is common to
proceed to treatment of the brain tumors without a definitive
histological diagnosis (15,16).
In the present case, since surgery was performed, the brain lesion
was histologically confirmed as an adenocarcinoma, and IHC staining
for CK7, TTF-1, napsin A and CK20 strongly suggested that the
primary origin was lung adenocarcinoma (17-20).
It was herein considered that the following reasons
may have contributed to the long-term lack of relapse in the
present case: i) High diagnosis-specific graded prognostic
assessment (DS-GPA) score; ii) controlled primary lung lesion; and
iii) combination of resection and SRS for multiple BMs. In
particular, our decision to combine resection and SRS to avoid WBRT
may be the reason why there was no cognitive dysfunction.
The DS-GPA score is a prognostic factor for the
analysis of patients with BMs. For patients with lung cancer, the
DS-GPA score is determined by scoring four factors: KPS, age,
presence of extracranial metastases and number of BMs. According to
Sperduto et al (3), in
NSCLC, the MST in the poor prognosis group with low DS-GPA scores
(0-1.0) was 3.02 months. The score in our case was 2.5, and the MST
in patients with scores of 2.5-3.0 is hypothesized to be relatively
better at 9.43 months.
Some studies have investigated prognostic factors in
patients with NSCLC who have a small number of BMs. Kim et
al (21) retrospectively
reviewed patients with NSCLC treated with SRS for 1-4 BMs and
determined the following five factors as significant predictors of
OS: i) Status of systemic disease, ii) presence of neurogenic
deficits, iii) size of the brain tumor(s), iv) initial imaging
appearance of intratumoral necrosis and v) initial resection of the
primary lung lesion. Won et al (22) performed a retrospective study of
patients undergoing SRS for 1-5 BMs from NSCLC. Primary disease
control and ECOG PS were found to significantly affected survival.
The common prognostic factor between the two studies was that the
primary lung lesion was controlled. In our case, the primary lung
cancer was excised and controlled.
Andrew et al (6) performed a randomized controlled trial
(RCT) comparing WBRT alone to WBRT plus SRS for 1-3 BMs. Although
there was no difference in MST, WBRT plus SRS achieved longer
survival compared with WBRT alone among patients with a single BM.
Brown et al (5) conducted an
RCT comparing SRS alone to SRS plus WBRT among patients with 1-3
BMs. Although there was no difference in OS, there was less
cognitive deterioration at 3 months after SRS alone compared with
that after SRS plus WBRT. A similar pattern was also observed at 12
months in long-term survivors. Yamamoto et al (7) performed a prospective observational
study in patients with BMs (largest tumor <10 cm3 in
volume and <3 cm in longest diameter; total cumulative volume
≤15 cm3). SRS without WBRT in patients with 5-10 BMs was
non-inferior to that in patients with 2-4 BMs in terms of OS. Shuto
et al (23) analyzed a
subset of patients with BMs from NSCLC in their study. The 60-month
post-SRS rates of neurocognitive preservation were at least 85.7%,
with no difference between the two groups. Thus, if the number and
size of BMs are limited, SRS may be a better treatment option
compared with WBRT for patients with BMs, resulting in comparable
OS and less prominent cognitive dysfunction.
In our case, total resection of the 3-cm tumor was
performed, and SRS was selected for the remaining small nodules.
Kayama et al (11) conducted
an RCT comparing WBRT to salvage SRS in patients with 1-4 BMs and
only one surgically resected lesion ≥3 cm in diameter. Salvage SRS
was not inferior to WBRT in terms of OS after resection of the BM.
Although the proportion of patients with MMSE scores that did not
worsen at 12 months was similar between the two treatments, the
incidence of grade 2-4 cognitive dysfunction at 91 days after WBRT
was significantly higher compared with that after SRS. It was
therefore concluded that salvage SRS can be established as a
standard therapy for patients with 1-4 BMs.
To the best of our knowledge, this is the first case
report in the literature to describe a patient with multiple BMs
from NSCLC who has remained relapse-free for >13 years with no
neurological dysfunction, including cognitive deficit. Even in
patients with NSCLC and multiple BMs, long-term survival is
probable if the DS-GPA score is high and the lung lesion is
controlled. To reduce the risk of cognitive dysfunction in such
cases, we recommend local treatment without WBRT as the most viable
option, such as combining resection and SRS, if possible. Moreover,
to better understand the clinical and biological background of
patients with multiple BMs from NSCLC who achieve long-term
survival, it is necessary to accumulate data from cases similar to
the one presented herein.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TM designed the study and drafted the initial
manuscript. YS performed surgery for the brain metastasis in our
patient. TSe performed stereotactic radiosurgery for the brain
metastases in our patient. AS evaluated the pathological specimens.
TM, SI, TSh, EI, TN, MK and TT were involved in the patient's
medical care. SI, TSh, EI, TN, MK and TT reviewed and edited the
manuscript. SI and TT confirm the authenticity of the data. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The Ethics Committee of Tokyo Dental College
Ichikawa General Hospital approved this case report. The patient
has provided informed written consent.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of the case details and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hubbs JL, Boyd JA, Hollis D, Chino JP,
Saynak M and Kelsey CR: Factors associated with the development of
brain metastases: analysis of 975 patients with early stage
nonsmall cell lung cancer. Cancer. 116:5038–5046. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hsiao SH, Chung CL, Chou YT, Lee HL, Lin
SE and Liu HE: Identification of subgroup patients with stage
IIIB/IV non-small cell lung cancer at higher risk for brain
metastases. Lung Cancer. 82:319–323. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Sperduto PW, Kased N, Roberge D, Xu Z,
Shanley R, Luo X, Sneed PK, Chao ST, Weil RJ, Suh J, et al: Summary
report on the graded prognostic assessment: An accurate and facile
diagnosis-specific tool to estimate survival for patients with
brain metastases. J Clin Oncol. 30:419–425. 2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Coia LR, Aaronson N, Linggood R, Loeffler
J and Priestman TJ: A report of the consensus workshop panel on the
treatment of brain metastases. Int J Radiat Oncol Biol Phys.
23:223–227. 1992.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Brown PD, Jaeckle K, Ballman KV, Farace E,
Cerhan JH, Anderson SK, Carrero XW, Barker FG II, Deming R, Burri
SH, et al: Effect of radiosurgery alone vs radiosurgery with whole
brain radiation therapy on cognitive function in patients with 1 to
3 brain metastases: A randomized clinical trial. JAMA. 316:401–409.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Andrew DW, Scott CB, Sperduto PW, Flanders
AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary
JP, et al: Whole brain radiation therapy with or without
stereotactic radiosurgery boost for patients with one to three
brain metastases: Phase III results of the RTOG 9508 randomised
trial. Lancet. 363:1665–1672. 2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yamamoto M, Serizawa T, Shuto T, Akabane
A, Higuchi Y, Kawagishi J, Yamanaka K, Sato Y, Jokura H, Yomo S, et
al: Stereotactic radiosurgery for patients with multiple brain
metastases (JLGK0901): A multi-institutional prospective
observational study. Lancet Oncol. 15:387–395. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Bindal RK, Sawaya R, Leavens ME and Lee
JJ: Surgical treatment of multiple brain metastases. J Neurosurg.
79:210–216. 1993.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Iuchi T, Shingyoji M, Sakaida T, Hatano K,
Nagano O, Itakura M, Kageyama H, Yokoi S, Hasegawa Y, Kawasaki K
and Iizasa T: Phase II trial of gefitinib alone without radiation
therapy for Japanese patients with metastases from EGFR-mutant lung
adenocarcinoma. Lung Cancer. 82:282–287. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Reungwetwattana T, Nakagawa K, Cho BC,
Cobo M, Cho EK, Bertolini A, Bohnet S, Zhou C, Lee KH, Nogami N, et
al: CNS response to osimertinib versus standard epidermal growth
factor receptor tyrosine kinase inhibitors in patients with
untreated EGFR-mutated advanced non-small-cell lung cancer. J Clin
Oncol: Aug 28, 2018 (Epub ahead of print).
|
|
11
|
Kayama T, Sato S, Sakurada K, Mizusawa J,
Nishikawa R, Narita Y, Sumi M, Miyakita Y, Kumabe T, Sonoda Y, et
al: Effects of surgery with salvage stereotactic radiosurgery
versus surgery with whole-brain radiation therapy in patients with
one to four brain metastases (JCOG0504): A phase III,
noninferiority randomized controlled trial. J Clin Oncol: Jun 20,
2018 (Epub ahead of print).
|
|
12
|
Soblin LH and Wittekind C (eds): TNM
Classification of Malignant Tumours (UICC). 6th edition.
Wiley-Liss, New York, NY, 2002.
|
|
13
|
Lutterbach J, Bartelt S and Ostertag C:
Long-term survival in patients with brain metastases. J Cancer Res
Clin Oncol. 128:417–425. 2002.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kotecha R, Vogel S, Suh JH, Barnett GH,
Murphy ES, Reddy CA, Parsons M, Vogelbaum MA, Angelov L, Mohammadi
AM, et al: A cure is possible: A study of 10-year survivors of
brain metastases. J Neurooncol. 129:545–555. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
National Comprehensive Cancer Network:
NCCN Clinical Practice Guidelines in Oncology for Non-Small Cell
Lung Cancer Version 6.2021. http://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf.
Accessed October 19, 2021.
|
|
16
|
Nabors LB, Portnow J, Ahluwalia M,
Baehring J, Brem H, Brem S, Butowski N, Campian JL, Clark SW,
Fabiano AJ, et al: Central nervous system cancers, version 3.2020,
NCCN clinical practice guidelines in oncology. J Natl Compr Canc
Netw. 18:1537–1570. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Travis WD, Brambilla E, Noguchi M,
Nicholson AG, Geisinger KR, Yatabe Y, Beer DG, Powell CA, Riely GJ,
Van Schil PE, et al: International association for the study of
lung cancer/American thoracic society/European respiratory society
international multidisciplinary classification of lung
adenocarcinoma. J Thorac Oncol. 6:244–285. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Varadhachary GR, Abbruzzese JL and Lenzi
R: Diagnostic strategies for unknown primary cancer. Cancer.
100:1776–1785. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Bishop JA, Sharma R and Illei PB: Napsin A
and thyroid transcription factor-1 expression in carcinomas of the
lung, breast, pancreas, colon, kidney, thyroid, and malignant
mesothelioma. Hum Pathol. 41:20–25. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bekaert L, Emery E, Levallet G and
Lechapt-Zalcman E: Histopathologic diagnosis of brain metastases:
Current trends in management and future considerations. Brain Tumor
Pathol. 34:8–19. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kim YS, Kondziolka D, Flickinger JC and
Lunsford LD: Stereotactic radiosurgery for patients with nonsmall
cell lung carcinoma metastatic to the brain. Cancer. 80:2075–2083.
1997.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Won YK, Lee JY, Kang YN, Jang JS, Kang JH,
Jung SL, Sung SY, Jo IY, Park HH, Lee DS, et al: Stereotactic
radiosurgery for brain metastasis in non-small cell lung cancer.
Radiat Oncol J. 33:207–216. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Shuto T, Akabane A, Yamamoto M, Serizawa
T, Higuchi Y, Sato Y, Kawagishi J, Yamanaka K, Jokura H, Yomo S, et
al: Multiinstitutional prospective observational study of
stereotactic radiosurgery for patients with multiple brain
metastases from lung cancer (JLGK0901 study-NSCLC). J Neurosurg.
129 (Suppl 1):S86–S94. 2018.PubMed/NCBI View Article : Google Scholar
|