Introduction
Over the past 20 years, totally laparoscopic distal
gastrectomy (TLDG), in which all procedures including lymph node
dissection, resection of the stomach and duodenum, and anastomosis
are performed intracorporeally, has been developed due to
improvements in the instruments and techniques. Roux-en-Y (R-Y)
reconstruction following TLDG is performed when the remnant stomach
is small, the length of the duodenal bulb is short, or
gastroesophageal reflux due to hiatal hernia is anticipated
(1-8).
Several authors reported the performance of antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side following TLDG combined with the gastrojejunostomy, in which a
functional end-to-end anastomosis is created using endoscopic
linear staplers (1,4,5). In
this gastrojejunostomy technique, first, without dividing the
lifted jejunum, stapling of the greater curvature of the remnant
stomach and the lifted jejunum without creating a gap using one
linear stapler is performed so that the distal side of the lifted
jejunum is located on the patient's left side. Thereafter, closure
of the stapler entry hole and division of the lifted jejunum are
carried out simultaneously by a second stapling. However, one
drawback of this gastrojejunostomy technique is the occurrence of
anastomotic failure at the closing staple line due to slippage of
the alimentary tract during the second stapling (4), even though antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side following TLDG is assumed to be useful thanks to the
prevention of intraoperative and postoperative twisting of the
gastrojejunostomy and lifted jejunum (9). Here, we describe our initial
experience in two patients with a novel gastrojejunostomy technique
consisting of linear stapling and hand suturing in antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side following TLDG to prevent anastomotic failure of the
gastrojejunostomy.
Patients and methods
Patients and ethical approval
Two patients with gastric cancer underwent
intracorporeal gastrojejunostomy consisting of linear stapling and
hand suturing in antecolic R-Y reconstruction with its efferent
loop located on the patient's left side following TLDG. Written
informed consent was obtained from each patient, both of whom
agreed to undergo TLDG. Case 1 (73-year-old female) was operated on
at Otori Stomach and Intestines Hospital (Sakai-City, Osaka, Japan)
in August 2019, and Case 2 (64-year-old male) was operated on at
Tanigawa Memorial Hospital (Ibaraki-City, Osaka, Japan) in March
2021. This procedure was approved by the Institutional Review Board
of the Otori Stomach and Intestines Hospital (approval no.
19000010) and Tanigawa Memorial Hospital (approval no.
21000001).
Procedure
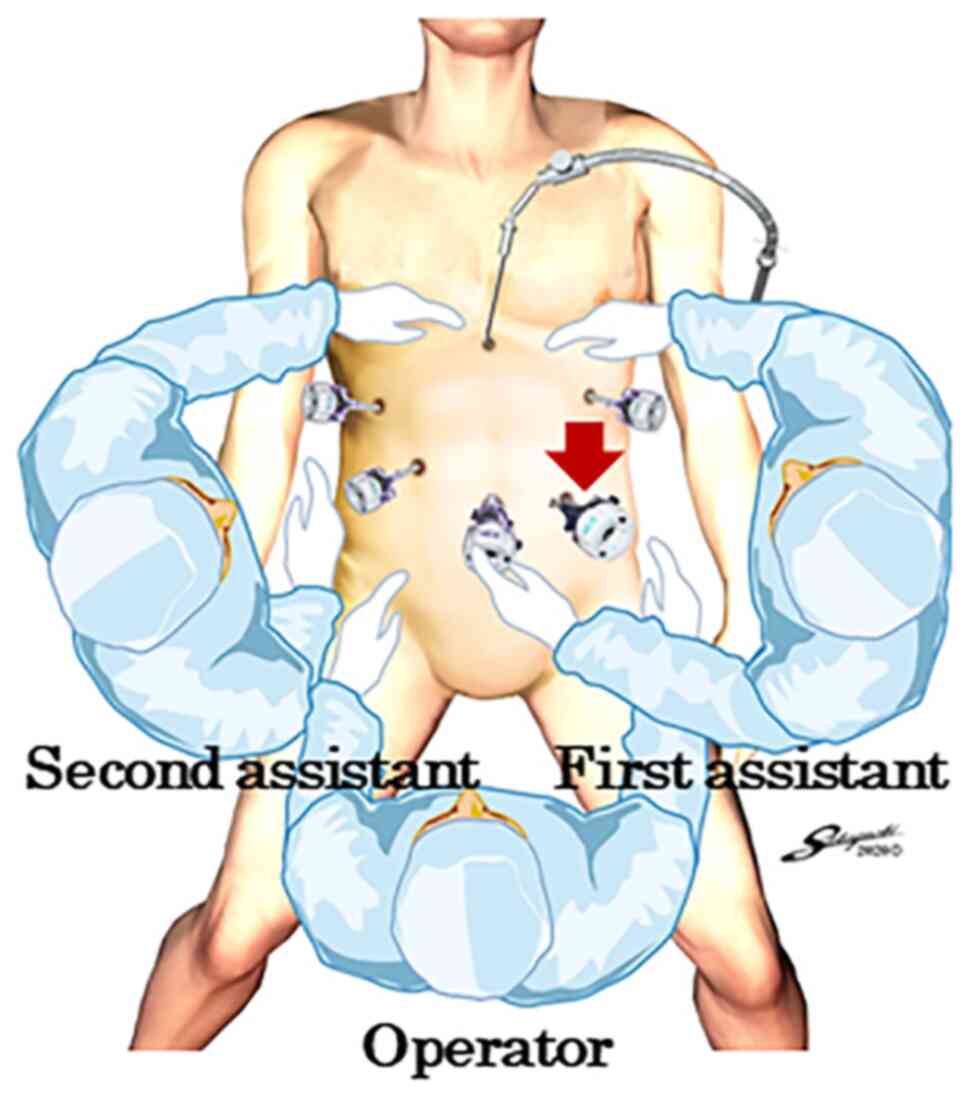
The patients were placed in the modified lithotomy
position. The operator stood between the patient's legs, with the
first assistant manipulating a laparoscope at the patient's left
side and the second assistant at the right side (Fig. 1). After five ports were placed in
the upper abdomen including the umbilicus, a Nathanson's retractor
was inserted from just below the xiphoid process to elevate the
round ligament and the lateral segment of the liver (Fig. 1). Because the endoscopic linear
stapler was inserted through the left lower port, all staplings
were performed by the right hand of the operator positioned between
the patient's legs. LDG with D1+ lymphadenectomy based on the
Japanese treatment guidelines was performed under a
pneumoperitoneum (10). The
duodenal bulb was transected using one endoscopic linear stapler
(60 mm Gold cartridge, Powered ECHELON FLEX® GST SYSTEM;
Ethicon, Cincinnati, OH, USA) during lymphadenectomy. The proximal
stomach was transected using two linear staplers (60 mm Gold
cartridge, Powered ECHELON FLEX® GST SYSTEM; Ethicon)
after lymphadenectomy, referring to preoperative endoscopic
markings (11). The specimen was
retrieved through the extended umbilical wound using a large
plastic bag, after which pneumoperitoneum was re-established.
Antecolic R-Y reconstruction with its efferent loop
located on the patient's left side was then performed in the two
patients. This technique consisted of intracorporeal
gastrojejunostomy and extracorporeal jejunojejunostomy with the use
of linear stapling and hand suturing. The jejunum was grasped
intracorporeally so that the distal side was located on the
patient's left side, and the mesentery was dissected along the
lifted jejunum from a portion 20 cm distal to the ligament of
Treitz to a portion 30 cm distal. Small incisions were made on the
antimesenteric side of the lifted jejunum 33 cm distal to the
ligament of Treitz and the greater curvature side of the remnant
stomach. The operator inserted one linear stapler (60 mm Gold
cartridge, Powered ECHELON FLEX® GST SYSTEM, Ethicon)
into the jejunum toward the distal side. Then, the operator
retracted the jejunum antecolically and inserted the stapler into
the remnant stomach (Fig. 2).
Linear stapling of the greater curvature of the remnant stomach and
the antimesenteric surface of the lifted jejunum was performed
without creating a gap (Fig. 2).
The operator transected the lifted jejunum at the portions 20 cm
and 30 cm distal to the ligament of Treitz using one linear stapler
(60 mm, White cartridge, Powered ECHELON FLEX® GST
SYSTEM, Ethicon) at each location (Fig. 3A and B), and the sacrificed jejunum was removed
in a cut finger of a surgical glove.
The operator closed the stapler entry hole with the
right hand using a single-layer full-thickness, serosubmucosal
suturing technique with knotted sutures and a knotless barbed
suture after confirming that there was no bleeding in the
intraluminal staple line. After removing the edge of the anterior
side of the stapler entry hole, a full-thickness suture of 3-0
Prolene (Ethicon) using the extracorporeal slip knot technique
(Roeder's knot) was placed on the anterior side of the stapler
entry hole (Fig. 4A). The second
assistant retracted this knotted suture toward the ventral side to
create a good view of the posterior side of the stapler entry hole
(Fig. 4B). Single-layer
full-thickness and serosubmucosal continuous suturing with a
15-cm-long absorbable barbed suture (3-0 V-Loc 180; VLOCL0604;
taper point, 1/2 circle/26 mm; Covidien) was performed from the
posterior side to the anterior side. The first full-thickness
stitch was placed on the posterior side, and the needle was passed
through the loop (Fig. 5A). The
second stitch was made between the serosubmucosal layers of the
lifted jejunum and remnant stomach (Fig. 5B and C). This single-layer serosubmucosal
continuous suturing with a 15-cm-long absorbable barbed suture (3-0
V-Loc 180) was performed until the last stitch was made (Fig. 5D). The last full-thickness stitch
was placed on the anterior side so that the suture crossed over the
knotted 3-0 Prolene suture (Fig.
5E). The suture end was cut simply to be as short as possible.
Some full-thickness knotted sutures of 3-0 Prolene were added at
the site with a broad pitch (Fig.
5F). Thereafter, the gastrojejunostomy in antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side was completed (Fig.
6A-C).
After a wound retractor (Alexis Wound Retractor S,
Applied Medical) was attached to the extended umbilical wound, a
side-to-side jejunojejunostomy with the use of linear stapling and
hand suturing was performed extracorporeally to create a 30-cm R-Y
limb. No stitches needed to be placed in the duodenal stump and the
antimesenteric side of the lifted jejunum. Petersen's defect and
the jejunojejunal mesenteric defect were closed intracorporeally
with two 15-cm-long nonabsorbable barbed sutures (3-0 V-Loc PBT;
VLOCN0604; taper point, 1/2 circle/26 mm; Covidien) (12). Finally, the antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side following TLDG was completed (Fig. 7).
Results
No twisting of the gastrojejunostomy and lifted
jejunum was encountered intraoperatively in either patient
(Fig. 7), nor were there any
postoperative complications including anastomotic failure,
anastomotic stenosis, stasis, or pancreatic fistula. Upper
gastrointestinal fluoroscopic images on postoperative day 10 show
no anastomotic failure or stenosis of the gastrojejunostomy in
either patient (Fig. 8A and
B). The follow-up period was 25.8
months in Case 1 and 7.9 months in Case 2. The efferent loop in
both patients was confirmed to be located on the patient's left
side by endoscopic examination 3 months after the operation along
with confirmation that no twisting of the gastrojejunostomy and
lifted jejunum had occurred postoperatively (Fig. 9A and B). Moreover, there was no occurrence of
other complications including internal hernia or ileus.
Discussion
Following TLDG, Billroth-II (B-II) or R-Y
reconstruction is generally performed when the remnant stomach is
small or the length of the duodenal bulb is short. We carry out R-Y
reconstruction in this situation because it is thought to cause
less bile reflux into the remnant stomach and esophagus compared
with B-II reconstruction (13,14).
In the present patients, no findings of reflux esophagitis and
gastritis were encountered on endoscopic examination 3 months after
the operation.
Several authors reported antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side using only endoscopic linear staplers following TLDG (1,4,5). In
this gastrojejunostomy technique, first, without dividing the
lifted jejunum, stapling of the greater curvature of the remnant
stomach and the lifted jejunum without creating a gap is performed
using one linear stapler so that the distal side of the lifted
jejunum is located on the patient's left side, and closure of the
stapler entry hole and division of the lifted jejunum are carried
out simultaneously by a second stapling. In this procedure,
twisting of the lifted jejunum when performing the
gastrojejunostomy is prevented because the first stapling of the
remnant stomach and lifted jejunum is performed without dividing
the jejunum. Moreover, because the jejunal arteries diverge from
the superior mesenteric artery toward the patient's left side, it
is physiological that the distal side of the jejunum be located on
the left side (9). Thus, twisting
of the lifted jejunum after performing gastrojejunostomy is
prevented when the efferent loop is located on the left side, and
it is assumed that this reconstruction system prevents twisting of
the linear-stapled gastrojejunostomy and lifted jejunum both
intraoperatively and postoperatively (9).
However, because closure of the stapler entry hole
and division of the lifted jejunum are performed simultaneously by
a second stapling in this gastrojejunostomy technique, this second
stapling for the posterior side of the entry hole tends to be
uncertain due to the presence of the undivided lifted jejunum
(4). Because anastomotic failure
of the gastrojejunostomy can occur for this reason, we carried out
the gastrojejunostomy in the present two patients by 1) creating
the sacrificed jejunum from a portion 20 cm distal to the ligament
of Treitz to a portion 30 cm distal; 2) dividing the sacrificed
jejunum using two linear staplers; 3) retracting the knotted 3-0
Prolene suture on the anterior side of the stapler entry hole
toward the ventral side to create a good view of the posterior
side; 4) performing single-layer full-thickness and serosubmucosal
continuous suturing with a 15-cm-long absorbable barbed suture (3-0
V-Loc 180) from the posterior side to the anterior side; and 5)
adding several full-thickness knotted sutures of 3-0 Prolene on the
site with a broad pitch. Irwin et al reported that a
single-layer serosubmucosal anastomosis resulted in no incidence of
anastomotic failure of the gastrojejunostomy (15), and no such failure occurred in the
present patients.
Noshiro et al reported that when linear
stapling of the greater curvature of the remnant stomach and the
lifted jejunum is performed without dividing the jejunum in
antecolic R-Y reconstruction with its efferent loop located on the
patient's left side following TLDG, the outlet of the lifted
jejunum is sometimes raised cranially, leading to bending of the
lifted jejunum (3). As they
indicated, when the remnant stomach is very small in antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side following TLDG, linear stapling of the posterior wall of the
remnant stomach and the lifted jejunum after dividing the jejunum
and hand suturing of the stapler entry hole is considered to be
advisable because the outlet of the lifted jejunum is arranged
caudally, which prevents bending of the lifted jejunum (3).
In conclusion, intracorporeal gastrojejunostomy
consisting of linear stapling and hand suturing can be one
suggested option for gastrojejunostomy in antecolic R-Y
reconstruction with its efferent loop located on the patient's left
side following TLDG because this procedure can aid in the
prevention of anastomotic failure.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TaT and KY performed the operations. AO, ToT, and IK
advised on patient treatment. TaT, KK, SH and KY obtained the
medical images (e.g., upper gastrointestinal fluoroscopy and
endoscopy). TaT and EN analyzed and interpreted the patient data
regarding the surgical technique. TaT and EN confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
This surgical procedure was approved by the
Institutional Review Board of the Otori Stomach and Intestines
Hospital (approval no. 19000010; Osaka, Japan) and Tanigawa
Memorial Hospital (approval no. 21000001; Osaka, Japan). Written
informed consent was obtained from the patients. The identities of
the patients are fully anonymized in this report.
Patient consent for publication
Written informed consent was obtained from the
patients for the publication of their data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Takaori K, Nomura E, Mabuchi H, Lee SW,
Agui T, Miyamoto Y, Iwamoto M, Watanabe H and Tanigawa N: A secure
technique of intracorporeal Roux-Y reconstruction after
laparoscopic distal gastrectomy. Am J Surg.
189(178183)2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Uyama I, Sakurai Y, Komori Y, Nakamura Y,
Syoji M, Tonomura S, Yoshida I, Masui T, Inaba K and Ochiai M:
Laparoscopy-assisted uncut Roux-en-Y operation after distal
gastrectomy for gastric cancer. Gastric Cancer. 8:253–257.
2005.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Noshiro H, Ohuchida K, Kawamoto M,
Ishikawa M, Uchiyama A, Shimizu S and Tanaka M: Intraabdominal
Roux-en-Y reconstruction with a novel stapling technique after
laparoscopic distal gastrectomys totally laparoscopic gastrectomy.
Gastric Cancer. 12:164–169. 2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bouras G, Lee SW, Nomura E, Tokuhara T,
Nitta T, Yoshinaka R, Tsunemi S and Tanigawa N: Surgical outcomes
from laparoscopic distal gastrectomy and Roux-en-Y reconstruction:
Evolution in a totally intracorporeal technique. Surg Laparosc
Endosc Percutan Tech. 21:37–41. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lee SW, Tanigawa N, Nomura E, Tokuhara T,
Kawai M, Yokoyama K, Hiramatsu M, Okuda J and Uchiyama K: Benefits
of intracorporeal gastrointestinal anastomosis following
laparoscopic distal gastrectomy. World J Surg Oncol.
10(267)2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Motoyama K, Kojima K, Hayashi M, Kato K,
Inokuchi M and Sugihara K: β-Shaped intracorporeal Roux-en-Y
reconstruction after totally laparoscopic distal gastrectomy.
Gastric Cancer. 17:588–593. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ma JJ, Zang L, Yang A, Hu WG, Feng B, Dong
F, Wang ML, Lu AG, Li JW and Zheng MH: A modified uncut Roux-en-Y
anastomosis in totally laparoscopic distal gastrectomy: Preliminary
results and initial experience. Surg Endosc. 31:4749–4755.
2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nakamura K, Suda K, Suzuki A, Nakauchi M,
Shibasaki S, Kikuchi K, Nakamura T, Kadoya S, Inaba K and Uyama I:
Intracorporeal isosceles right triangle-shaped anastomosis in
totally laparoscopic distal gastrectomy. Surg Laparosc Endosc
Percutan Tech. 28:193–201. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Tokuhara T, Nakata E, Tenjo T, Kawai I,
Kondo K, Ueda H and Tomioka A: Stenosis after esophagojejunostomy
with the hemi-double-stapling technique using the transorally
inserted anvil (OrVil™) in Roux-en-Y reconstruction with its
efferent loop located on the patient's left side following
laparoscopic total gastrectomy. Surg Endosc. 33:2128–2134.
2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Japanese Gastric Cancer Association.
Japanese gastric cancer treatment guidelines 2018 (5th edition).
Gastric Cancer. 24:1–21. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tokuhara T, Nakata E, Tenjo T, Kawai I,
Satoi S, Inoue K, Araki M, Ueda H and Higashi C: A novel option for
preoperative endoscopic marking with India ink in totally
laparoscopic distal gastrectomy for gastric cancer: A useful
technique considering the morphological characteristics of the
stomach. Mol Clin Oncol. 6:483–486. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hara K, Hayashi T, Nakazono M, Nagasawa S,
Shimoda Y, Kumazu Y, Yamada T, Yamamoto N, Shiozawa M, Morinaga S,
et al: An easy and reliable method to close Petersen's defect using
barbed suture to prevent internal hernia from developing after
gastrectomy with Roux-en-Y reconstruction. Asian J Endosc Surg.
13:238–241. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fukuhara K, Osugi H, Takada N, Takemura M,
Higashino M and Kinoshita H: Reconstructive procedure after distal
gastrectomy for gastric cancer that best prevents
duodenogastroesophageal reflux. World J Surg. 26:1452–1457.
2002.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Shim JH, Oh SI, Yoo HM, Jeon HM, Park CH
and Song KY: Roux-en-Y gastrojejunostomy after totally laparoscopic
distal gastrectomy: Comparison with Billorth II reconstruction.
Surg Laparosc Endosc Percutan Tech. 24:448–451. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Irwin ST, Krukowski ZH and Matheson NA:
Single layer anastomosis in the upper gastrointestinal tract. Br J
Surg. 77:643–644. 1990.PubMed/NCBI View Article : Google Scholar
|