Introduction
Soft tissue sarcomas of the knee often require wide
excisions, affecting normal healthy tissues such as the joint
capsule, ligaments, muscles, and bones. After the resection of a
sarcoma, ligament and/or soft tissue reconstruction is recommended
(1-3).
Insufficiency or injury to the collateral ligament of the knee
affects its stability and function (2,4).
Reconstruction of the collateral ligaments using various types of
grafts has been reported (1,5-7).
Interestingly, the plantaris tendon has been used for the
reconstruction of the anterolateral ligament of the ankle, the
medial collateral ligament of the knee, and the Achilles tendon
(8-12).
However, there is a lack of literature on the reconstruction of the
lateral collateral ligament using the plantaris tendon after wide
excision of a malignant soft tissue sarcoma.
Herein, we present a case report of the
reconstruction of the lateral collateral ligament using the
plantaris tendon, after wide excision of soft tissue sarcoma in the
knee.
Case report
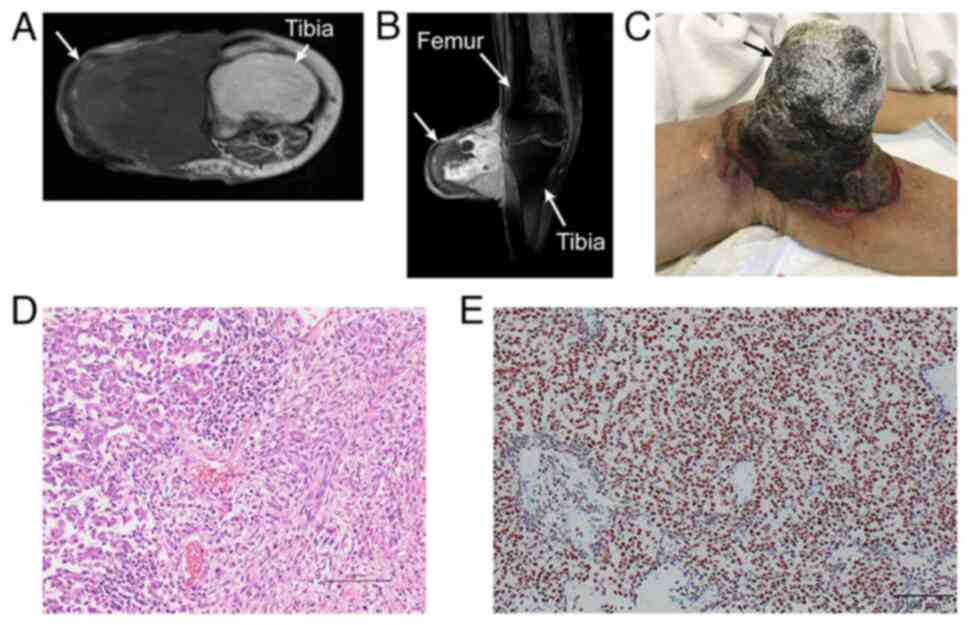
An 83-year-old woman presented to a hospital with a
three-month history of a growing mass on the lateral surface of the
right knee. Magnetic resonance imaging (MRI) revealed a soft tissue
tumor measuring 15x27x30 mm in the subcutis of the right knee
(Fig. 1A-D). The patient was
referred to University of the Ryukyus Hospital (Nishihara, Japan)
for further examination and treatment in July 2020. However, the
patient did not visit our institution since she was not
experiencing any pain. The size of the mass rapidly increased, and
hemorrhage from the tumor occurred two weeks ago. The patient then
decided to revisit the initial hospital, where MRI revealed a large
tumor measuring 65x73x80 mm (Fig.
2A and B). The patient was
referred to our institution again. On admission, she had no knee
pain due to the tumor. We applied Mohs paste (13) to the surface of the tumor to
control the bleeding (Fig. 2C).
Distant pulmonary metastases were not found on chest computed
tomography. Subsequently, needle biopsy and histopathological
examination revealed biphasic spindle and epithelial cell
components by hematoxylin and eosin staining (Fig. 2D). Most of the tumor cells were
positive for SS18-SSX fusion-specific antibody (Fig. 2E), and breakaparts of SS18 in the
tumor cells were confirmed with fluorescence in situ
hybridization (data not shown). The patient was diagnosed with
biphasic synovial sarcoma.
The patient underwent a wide excision and
reconstruction of the right knee. The tumor was excised with
adequate margins, including the joint capsule, lateral collateral
ligament, and fascia of the anterolateral compartment of the lower
leg (Fig. 3A). A lateral
gastrocnemius flap was elevated to cover the soft tissue defect in
the right knee (Fig. 3B). The
11-cm plantaris tendon was harvested for lateral collateral
ligament reconstruction (Fig. 3C
and D). The double-folded
plantaris tendon was attached to the lateral femoral condyle and
the head of the fibula using suture anchors with manual maximum
tension at 0 degrees of knee extension to reconstruct the lateral
collateral ligament (Fig. 3E).
Further, the soft tissue defect of the lateral aspect of the right
knee was covered with the lateral gastrocnemius flap. The skin
defect was covered with an artificial dermis
(Terudermis®, ALCARE Co., Ltd., Japan) and continuous
negative-pressure wound therapy was applied to it. Postoperatively,
the right knee was immobilized with an extended position knee brace
for three weeks. The patient was encouraged to walk with the knee
brace fixation as much as possible, and range of motion exercises
of the knee were allowed three weeks after surgery. The patient was
discharged from our hospital two months after surgery. In order to
cover the skin defect, split-thickness skin grafting was performed
at the initial hospital four months after the primary surgery.
At the 24-month follow-up, the patient could walk
using a T-cane without the lateral thrust of the right knee. Joint
space narrowing and osteophytes were found, but no lateral
instabilities of the right or left knee were found on varus stress
radiographs of the knee (Fig. 4A
and B). She had no complications
from the plantaris tendon harvesting. The range of motion of the
right knee was measured from 110˚ in flexion to 0˚. The patient had
a Musculoskeletal Tumor Society (MSTS) score of 86%, and MRI
revealed survival of the grafted plantaris tendon (Fig. 4C). No recurrence or distant
metastases were observed at the latest follow-up.
Discussion
We successfully reconstructed the lateral collateral
ligament of the knee using the plantaris tendon after wide excision
of a soft tissue sarcoma. Moreover, the soft tissue defect was
covered with a lateral gastrocnemius flap and artificial dermis.
Subsequently, the skin defect was covered with a skin graft.
Various types of grafts have been reported to be
used for the reconstruction of the lateral collateral ligament of
the knee, including gracilis and biceps femoris grafts (5), semitendinosus grafts (6), quadriceps tendon-patellar bone
autografts (7), and
bone-tendon-bone grafts (1). These
tendons were advantageous for the reconstruction of collateral knee
ligaments due to their biomechanical strength. The disadvantages of
harvesting the above-mentioned tendons wee not well-described
(1,5-7).
However, the disadvantage of harvesting major tendons may be the
potential risk of causing functional impairments. One study
reported the utilization of a bone-tendon-bone graft for the
reconstruction of the collateral ligament of the knee after the
resection of soft tissue sarcomas (1). In the study, reconstruction of the
medial and lateral collateral ligaments was performed in three
separate cases. Knee stability was achieved without any
complications in all cases.
We used the plantaris tendon for the reconstruction
of the lateral collateral ligament of the knee in this case. In a
cadaveric study, 9% of the examined limbs lacked the plantaris
tendon (14). Several reports have
revealed that ultrasonography was helpful to confirm the presence
of the plantaris tendon (15,16).
Biomechanically, the single-strand plantaris tendon has a much
lower ultimate load compared to the peroneus longus and Achilles
tendons due to the plantaris tendon's small cross-sectional area
(17). However, the biomechanical
properties of the double-folded plantaris tendon are comparable to
those of the original medial patellofemoral ligament, and thus the
plantaris tendon may be suitable for medial patellofemoral ligament
reconstruction (9). The plantaris
tendon displays excellent biomechanical properties for
anterolateral ligament (ALL) reconstruction (18). After using a double-folded
plantaris tendon in ALL reconstruction, during anterior cruciate
ligament (ACL) repair, patients were able to perform normal
rehabilitation without any restrictions. Despite the evidence for
the use of the plantaris tendon in reconstructive surgery, there is
a lack of literature on its use in collateral ligament
reconstruction for soft tissue tumor surgery. In this study, the
plantaris tendon was used for the reconstruction of the lateral
collateral ligament of the knee following the wide excision of a
malignant soft tissue sarcoma.
Reconstruction using the plantaris tendon has some
advantages. First, the functional loss of the knee is minimized if
the plantaris tendon is harvested. Second, harvesting the plantaris
tendon is straightforward when the gastrocnemius flap is elevated
to cover the soft tissue defect. To the best of our knowledge, this
is the first report of reconstruction of the lateral collateral
ligament using the plantaris tendon. The patient was able to walk
using a T-cane without the lateral thrust of the knee, and no
instabilities of the right knee were observed 24 months after the
primary surgery. Although the patient had a favorable MSTS score
and satisfactory knee function, the patient required careful
long-term follow-up for the tumor and knee function. In conclusion,
reconstruction of the lateral collateral ligament using the
plantaris tendon may be useful for preserving the function of the
knee joint after resection of soft tissue sarcoma of the knee.
Acknowledgements
The authors would like to thank Dr. Ryo Katsuki for
his data collection at the Okinawa Prefectural Yaeyama
Hospital.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated and analyzed during this study
are included in this published article.
Authors' contributions
YTs, HO, KM, YTo and KN contributed to conception of
this study. YTs, HO and KM contributed to acquisition of data. YTs,
YTo, HO, KM and KN wrote and edited the manuscript. YTo and KN
conducted revision of the manuscript for important intellectual
content. YTo and HO performed the surgery and postoperative
management. TT and NW perfrmed the pathological
examination/diagnosis and the immunohistochemistry staining of the
SS18-SSX fusion-specific antibody. YTs and YTo confirmed the
authenticity of all the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
YTo is on the editorial board for Cancer
Diagnosis and Prognosis. KN is on the editorial board of the
Journal of Orthopaedic Research and is a board member of the
International Society for the Study of Lumbar Spine.
References
|
1
|
Popov P, Barner-Rasmussen I and Tukiainen
E: Microvascular flaps and collateral ligament reconstructions for
soft tissue sarcomas at the knee joint. Ann Plast Surg. 64:24–27.
2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Abdel MP, Papagelopoulos PJ, Morrey ME,
Inwards CY, Wenger DE, Rose PS and Sim FH: Malignant proximal
fibular tumors: Surgical management of 112 cases. J Bone Joint Surg
Am. 94(e165)2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zhao SC, Zhang CQ and Zhang CL:
Reconstruction of lateral knee joint stability following resection
of proximal fibula tumors. Exp Ther Med. 7:405–410. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Erler K, Demiralp B, Ozdemir MT and
Basbozkurt M: Treatment of proximal fibular tumors with en bloc
resection. Knee. 11:489–496. 2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Senevirathna S, Stragier B and Geutjens G:
Posterolateral corner reconstruction of the knee using gracilis
autograft and biceps femoris. Arthrosc Tech. 11:e741–e753.
2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Buzzi R, Aglietti P, Vena LM and Giron F:
Lateral collateral ligament reconstruction using a semitendinosus
graft. Knee Surg Sports Traumatol Arthrosc. 12:36–42.
2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chen CH, Chen WJ and Shih CH: Lateral
collateral ligament reconstruction using quadriceps tendon-patellar
bone autograft with bioscrew fixation. Arthroscopy. 17:551–554.
2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Vlaic J, Josipovic M, Bohacek I and Jelic
M: The plantaris muscle: Too important to be forgotten. A review of
evolution, anatomy, clinical implications and biomechanical
properties. J Sports Med Phys Fitness. 59:839–845. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Vlaic J, Josipovic M, Bohacek I, Pilipovic
A, Skavic P, Schauperl Z and Jelic M: Plantaris tendon is valuable
graft for the medial patellofemoral ligament reconstruction: A
biomechanical study. Knee. 38:212–219. 2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Walther M: Management on chronic lateral
ankle instability with an autologous plantaris longus graft. In:
Operative Techniques in Foot and Ankle Surgery. Easley ME, Wiesel
SW and Albert TJ (eds). Lippincott Williams & Wilkins, a
Wolters Kluwer Business, Philadelphia, PA, pp1076-1083, 2021.
|
|
11
|
Hamid K and Easley ME: Subacute and
chronic Achilles tendon disorders and ruptures. In: Operative
Techniques in Foot and Ankle Surgery. Easley ME, Wiesel SW and
Albert TJ (eds). Lippincott Williams & Wilkins, a Wolters
Kluwer Business, Philadelphia, PA, pp1141-1165, 2021.
|
|
12
|
Lynn TA: Repair of the torn achilles
tendon, using the plantaris tendon as a reinforcing membrane. J
Bone Joint Surg Am. 48:268–272. 1966.PubMed/NCBI
|
|
13
|
Mohs FE, Sevringhaus EL and Schmidt ER:
Conservative amputation of gangrenous parts by chemosurgery. Ann
Surg. 114:274–282. 1941.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Simpson SL, Hertzog MS and Barja RH: The
plantaris tendon graft: An ultrasound study. J Hand Surg Am.
16:708–711. 1991.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chang KV, Wu WT and Özçakar L:
Ultrasonograpy imaging for the dignosis and guided injection of
plantaris tendo strain in a paitnet with tennis leg. Am J Phys Med
Rehabil. 97:e60–e61. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hung CY and Chang KV: An uncommon cause of
posterior leg pain-ultrasound image of plantaris tendinopathy. J
Clin Diagn Res. 10:YJ01–YJ02. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bohnsack M, Sürie B, Kirsch IL and Wülker
N: Biomechanical properties of commonly used autogenous transplants
in the surgical treatment of chronic lateral ankle instability.
Foot Ankle Int. 23:661–664. 2002.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Josipović M, Vlaić J, Serdar J, Šimunović
M, Nizić D, Schauperl Z, Bojanić I and Jelić M: Plantaris tendon: a
novel graft for anterolateral ligament reconstruction and
additional reinforcement for anterior cruciate ligament autografts
in combined reconstructive procedures. Knee Surg Sports Traumatol
Arthrosc. 28:2604–2608. 2020.PubMed/NCBI View Article : Google Scholar
|