Introduction
Primary bone tumors, whether benign or malignant,
can cause pathological fractures (1,2). In
particular, cystic bone tumors in the long bones of the extremities
are prone to pathological fractures (3). By contrast, 10% of patients with
primary malignancies develop metastases to the proximal femur. Most
bone metastases originate from the breast, kidney, thyroid,
prostate, or myeloma. In addition, these are either soluble or
mixed; therefore, patients are at high risk of pathologic fractures
(4). In 2001, Scorianz et
al (5) published an algorithm
for the treatment of long bone and pelvic metastases. The patients
were divided into 4 classes: i) isolated lesions with a favorable
prognosis; ii) pathologic fractures; iii) incisional fractures; and
iv) other lesions. The most important factors for selecting the
appropriate treatment for the long bones and pelvis include
prognosis, disease type, visceral metastases, time taken to spread
from the primary site, risk of pathologic fracture, sensitivity to
chemotherapy, hormonal therapy and irradiation. Pathologic
fractures also occur in 5-10% of patients with osteosarcoma, both
at diagnosis and during chemotherapy (6,7). The
role of orthopedic surgeons in the evaluation of patients with
skeletal metastases is likely to increase over time, as improved
treatment of patients with cancer increases survival (8). In addition, pathological fractures of
the proximal femur are 3.5 times more likely to occur than
pathological fractures of the proximal humerus (9). However, there is a lack of literature
describing cases of pathological or impending fractures of the
lower extremities in patients with primary and metastatic
malignancies. Therefore, the present study aimed to provide a
detailed description of the clinical characteristics of patients
with pathological or impending fractures who underwent surgical
treatment. In addition, the authors also aimed to examine the
benefits and drawbacks of their treatment strategy.
Patients and methods
Patients
A total of 38 patients with impending and
pathological fractures were treated in the Department of Orthopedic
Surgery, Kindai University Hospital between March 2011 and November
2023 and were included in the present study. Cases in which the
post-treatment course could be followed were included, and those in
which the course could not be followed were excluded. Data on age,
sex, pathology, number of metastases, pre-fracture Eastern
Cooperative Oncology Group performance status (ECOG-PS) (10), adjuvant therapy, treatment
modality, operative time, blood loss, postoperative complications,
Musculoskeletal Tumor Society (MSTS) score (11), follow-up period and outcomes were
retrospectively studied. Post-treatment MSTS scores in cases of
impending and pathological fractures were compared. The MSTS scores
were also compared between intramedullary nail fixation and
surgical procedures other than intramedullary nail fixation. In
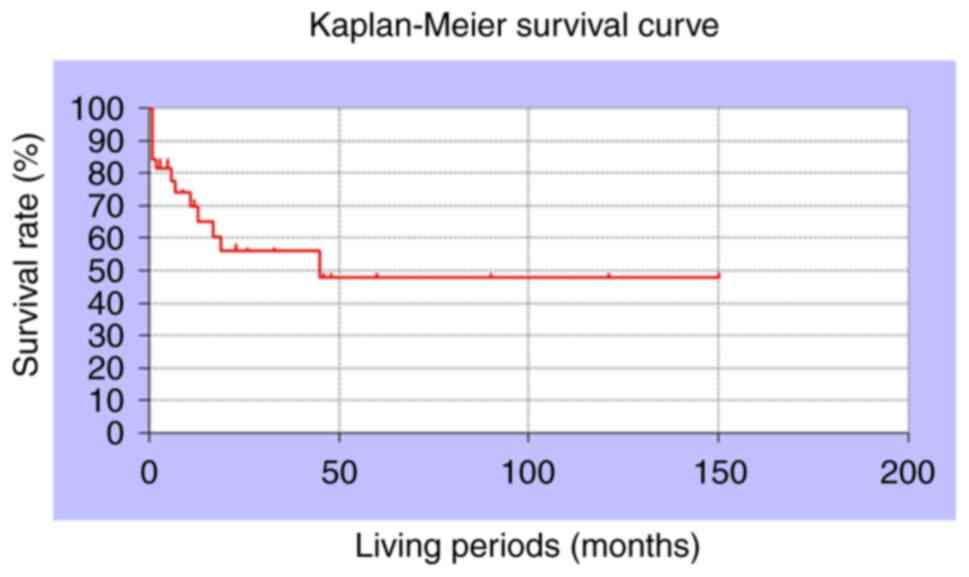
addition, the 1-year overall survival of patients using the
Kaplan-Meier method was investigated. All patients were treated
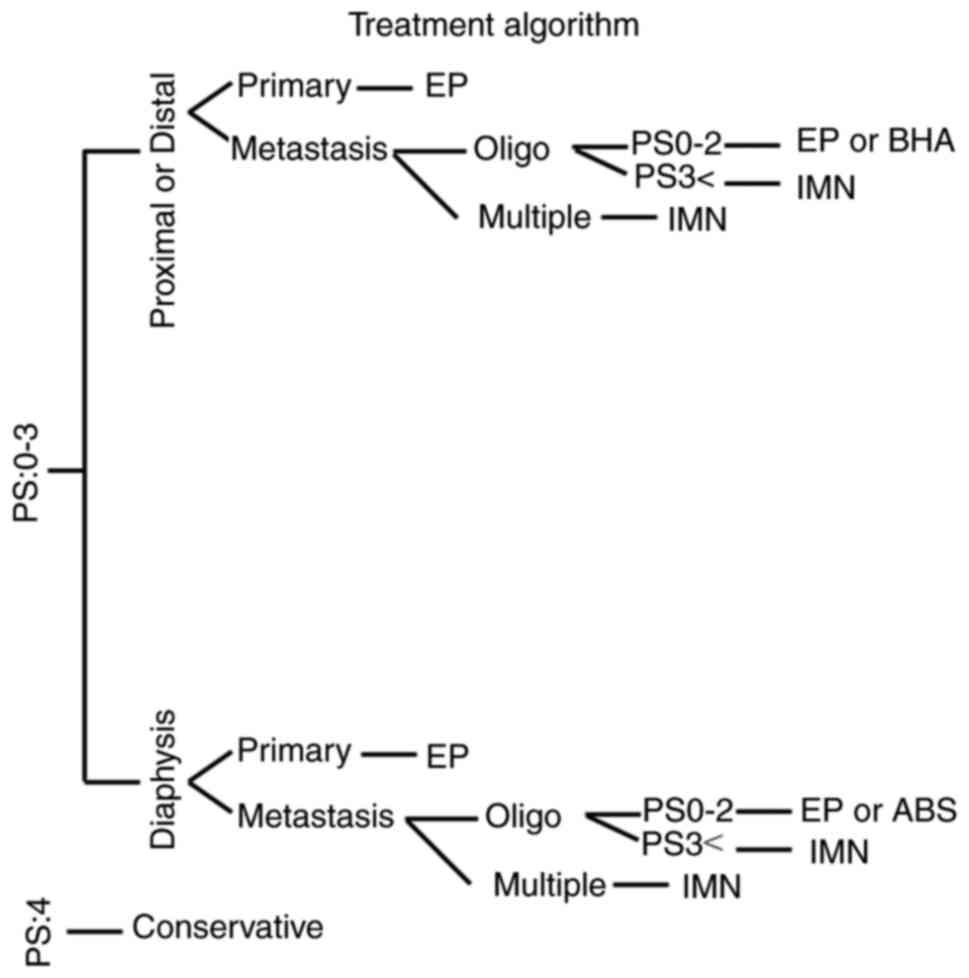
using the algorithm shown in Fig.
1. The MSTS scores and ECOG-PS were compared using Student's
t-test in 8 cases of primary malignant tumors and 30 cases of
metastatic malignant tumors. In brief, the algorithm was as
follows: First, patients were divided by their ECOG-PS (0-3 or 4).
If 4, conservative treatment was chosen. Second, patients were then
further divided by fracture site (proximal, distal or diaphyseal),
followed by the focus (primary or metastasis), and number of
metastases throughout the body (oligo or multiple). Finally,
patients were divided by ECOG-PS (0, 2 or 3). The present study was
approved by the Ethics Committee of Kinki University (approval no.
31-153; Osakasayama, Japan).
Statistical analysis
Variables are presented as the mean ± standard
deviation (SD). The MSTS scores were compared using the unpaired
Student's t-test for patients who underwent intramedullary nail
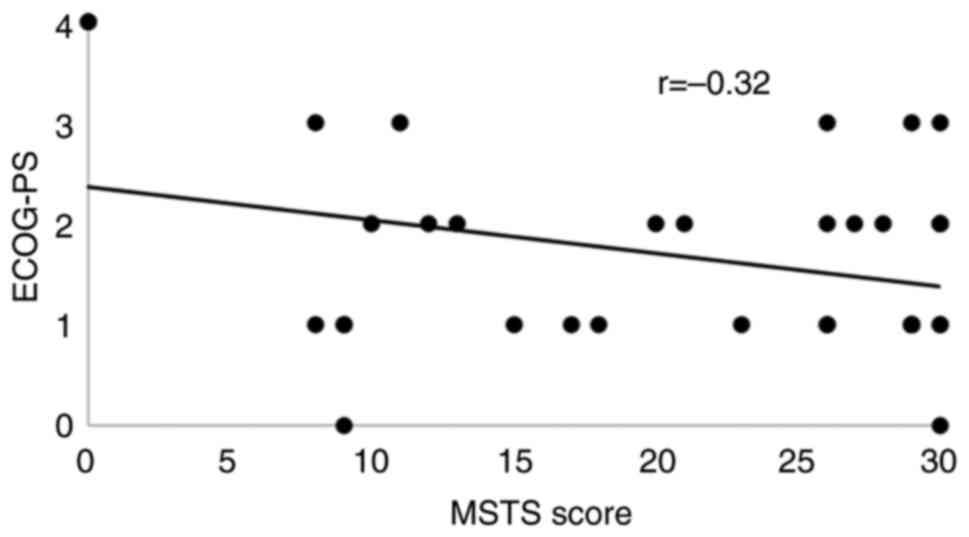
surgery vs. other surgeries. ECOG-PS and MSTS scores were plotted
to create a correlation diagram, and the coefficient of
determination (R²) was calculated by drawing a best-fit line to
assess the correlation between ECOG-PS and MSTS scores. Pearson's
correlation method was employed to determine these correlations.
The strength of the correlation was classified according to
Pearson's correlation coefficient (R) as follows: Very strong
1.0≥|R|≥0.7, strong 0.7≥|R|≥0.5, moderate 0.5≥|R|≥0.4, medium
0.4≥|R|≥0.3, weak 0.3≥|R|≥0.2 and no correlation 0.2≥|R|≥0.0.
Overall postoperative survival was calculated using the
Kaplan-Meier method.
P<0.05 was considered statistically significant
for all analyses. All statistical analyses were performed using
Stat Mate 5.05 (ATMS; (https://atms.shop-pro.jp/?pid=64906245).
Results
The present study included 19 men and 19 women
(Table I). The median patient age
was 68 years (range: 13-83 years). Cancer sites included the
sub-trochanteric femur in 10 patients, the trochanteric femur in 8,
the femoral diaphysis in 7, the femoral neck in 5, the bilateral
trochanteric femur in 3, the tibia in 3, and the distal femur in 2
patients. Primary nodal pathology included lung cancer in 9
patients, breast cancer in 7, renal cancer in 3, multiple myeloma
in 3, osteosarcoma in 3, liver cancer in 2, gastric cancer in 2,
cancer of unknown primary origin in 2 and esophageal cancer,
hemangiopericytoma, hemangiosarcoma, Paget's disease, neuroblastoma
and chondrosarcoma in 1 patient each. Altogether, 10 patients had
metastases between 3-20 sites. The median ECOG-PS score before the
fracture was 1 (range 0-4: 0, 2 patients; 1, 18 patients; 2, 12
patients; 3, four patients; and 4, 2 patients). As adjuvant
chemotherapy, radiotherapy was administered to 5, chemotherapy to 8
and radiotherapy and chemotherapy to 10 patients. Surgical
procedures included intramedullary nail fixation in 18 patients,
endoprosthesis in 4, plate fixation in 3, bipolar head arthroplasty
in 3, compression hip screw (CHS) in 3, conservative treatment in
2, bilateral intramedullary nail fixation in 2 and artificial bone
stem with combined intramedullary nail and plate fixation,
right-sided artificial head replacement and left-sided CHS in one
patient each. The operating time was 100±45.8 min and blood loss
was 63±153.4 ml. The MSTS score was 19.9±8.95 for intramedullary
nail fixation and 24.3±7.45 for procedures other than
intramedullary nail fixation, with no significant difference
(P=0.13) and a negative correlation between the MSTS score and
pre-fracture ECOG-PS (r=-0.32; Fig.
2). Postoperative complications included implant failure after
intramedullary nail fixation, which was replaced by tumor
arthroplasty in 1 patient. The median observation period was 8
months (range: 1-150 months). The outcomes were as follows: Alive
with disease, 23 patients; continued disease-free, 1 patient; and
dead due to disease, 14 patients. The 1-year postoperative survival
rate was 60.5% (Fig. 3). The MSTS
scores of metastatic malignant tumors (18.0±10.0) were
significantly lower than the MSTS scores of primary malignant
tumors (29.1±1.3) (average ± SD; P<0.01) (data not shown). In
addition, the ECOG-PS of metastatic malignant tumors (1.7±1.0) was
significantly worse than that of primary malignant tumors
(0.87±0.35) (average ± SD; P<0.01) (data not shown).
 | Table ICharacteristics of the study
population. |
Table I
Characteristics of the study
population.
| Factor | Patients, n |
|---|
| Age (mean years) | 68 |
|
≤70 | 22 |
|
>70 | 16 |
| Sex | |
|
Male | 19 |
|
Female | 19 |
| Fracture site | |
|
Femoral
neck | 5 |
|
Femoral
diaphysis | 7 |
|
Intertrochanteric | 8 |
|
Subtrochanteric | 10 |
|
Bilateral
intertrochanteric | 3 |
|
Proximal
tibia | 3 |
|
Distal
femur | 2 |
| Type of cancer | |
|
Lung | 9 |
|
Breast | 7 |
|
Kidney | 3 |
|
Multiple
Myeloma | 3 |
|
Osteosarcoma | 2 |
|
Liver | 2 |
|
Gastric | 2 |
|
Unknown | 2 |
|
Esophageal | 1 |
|
Hemangiopericytoma | 1 |
|
Paget | 1 |
|
Neuroblastoma | 1 |
|
Chondrosarcoma | 1 |
| Number of
metastasis | |
|
Equal or
less than 3 | 10 |
|
More than
3 | 20 |
| ECOG-PS | |
|
<2 | 20 |
|
2-3 | 16 |
|
>3 | 2 |
| Adjuvant therapy | |
|
Radiotherapy | 5 |
|
Chemotherapy | 8 |
|
Chemotherapy
and radiotherapy | 10 |
|
None | 2 |
| Treatment
modality | |
|
Intramedullary
nail | 18 |
|
Endoprosthesis | 4 |
|
Fixation
with plate | 3 |
|
Bipolar head
arthroplasty | 3 |
|
Fixation
with CHS | 3 |
|
Bilateral
intramedullary nail | 2 |
|
Conservative | 2 |
|
Artificial
bone stem | 1 |
|
Rt. Bipolar
head arthroplasty, Lt. fixation with CHS | 1 |
| Operating time
(min) | |
|
0-100 | 18 |
|
>100 | 18 |
| Blood loss | |
|
0-60 | 17 |
|
>60 | 19 |
| MSTS score | |
|
0-10 | 9 |
|
11-20 | 7 |
|
21-30 | 22 |
| Outcome | |
|
CDF | 1 |
|
AWD | 23 |
|
DOD | 14 |
| Follow-up periods
(months) | |
|
Mean | 8 |
|
Range | 1-150 |
Discussion
In this retrospective investigation of outcomes for
malignant bone tumors of the lower extremities, the treatment
outcomes according to the utilized treatment algorithm were
favorable.
The most commonly reported sites of pathological
fractures are the femur, humerus, and tibia (12). The other reported sites of
pathological fractures besides the lower extremities include the
neck (50%), adductor region (30%) and sub-acetabulum (20%)
(12). A different study reported
47.5% fractures in the femoral head and neck, 27.5% in the femoral
metaphyseal area, and 25% in the region below the femoral
metaphyseal area (13). In the
present study, fractures were more common in the femoral and
sub-trochanteric areas than in the femoral neck area.
In a previous study, the most common primary sites
of pathological femoral fractures were breast cancer, myeloma,
renal cancer, colorectal cancer, thyroid cancer and lung cancer
(14). Breast, lung, myeloma, and
kidney cancers are the most common primary lesions resulting in
pathological fractures of the proximal femur (13). Lung cancer was relatively common in
the current study, with reconstructive surgery with oncological
arthroplasty, intramedullary nail fixation, or plate fixation as
the most commonly adopted options (15-17).
The advantages of tumor arthroplasty include a quick
return to stability, independent of the degree of fracture healing,
and minimal risk of local progression or implant failure (18). The disadvantages include surgical
invasiveness, bleeding, relative difficulty in muscle
reconstruction and high costs (18). The advantages of intramedullary
nail fixation include relatively low surgical invasion, the
possibility of additional radiation therapy and the ability to load
immediately after radiation (18).
The disadvantages of plate fixation include the need for adequate
bone stock, lack of stability in close proximity to the joint, risk
of implant fracture, large incision, long surgical procedure, and
lack of prophylactic fixation of the entire bone (18). The advantages of plate fixation
include prevention of damage to the muscle cuff, strong fixation
with locking screws, fixation of distal fractures and a relatively
large operative field that allows visual resection of the tumor
(18). Intramedullary nail
fixation was used in the present study. The authors' department
policy is to reconstruct pathological fractures of the femoral neck
using either artificial head replacement or tumor arthroplasty;
this choice is based on tumor spread, prognosis, invasiveness and
the patient's ability to engage in rehabilitation including
load-bearing. For pathological fractures of the femoral condyle and
sub-trochanteric region, reconstruction using an intramedullary
nail was performed in anticipation of postoperative radiotherapy.
Impending fractures of the femoral neck or transverse condyle are
treated with bipolar head arthroplasty or fixation using
intramedullary nails or CHS plates. The selection of reconstruction
was based on a comprehensive evaluation of postoperative
radiotherapy, fixation stability and the amount of lesion removed.
Functional prognosis was generally favorable for both types of
fixation but was poor when rehabilitation did not proceed as
expected owing to the patient's general condition.
Several studies have reported different outcomes and
failure rates between the use of an intramedullary nail and
endoprosthesis (19-22).
Patients with malignancies are at the highest risk of
thromboembolic complications and infections (14), with the rate of infectious
complications ranging from 1.2-19.5%. Preoperative radiotherapy is
one of the most important risk factors for radiotherapy (14); in addition, location in the
proximal lower extremity has been reported as a risk factor for
major wound complications such as infection (23).
Complications have been reported in 9-20% of
patients who undergo intramedullary nail fixation, with primary
complications including deep infection, myocardial infarction and
stroke. Furthermore, 20% of the patients require revision surgery
within 3 months. On the other hand, dislocation is reported to
occur in 3-22% of the patients as a complication of tumor
arthroplasty. The risk of periprosthetic failure has also been
previously reported. In the present study, implant failure occurred
in one patient who underwent intramedullary nail fixation, which
was subsequently replaced by an oncological prosthesis. Previous
studies have reported MSTS scores of 6.4-25.2 after implant have
been used for pathological fractures (13,14,24).
The results of the present study are comparable, and it is
considered by the authors that their surgical indications (Fig. 1) are generally recommended.
Typically, treatment for this condition is
individually tailored as these patients are in the terminal disease
stage (25,26). In terms of overall patient
survival, the 1-year survival rate reported in the literature
ranges from 42-75% (21,27,28).
Fractures are also associated with an increased mortality risk in
patients with malignant bone disease (29). Until now, the Mirels' score has
been used in surgical treatment algorithms for malignant metastatic
bone tumors (30). According to
this algorithm, surgery is not indicated unless the patient has a
life expectancy of at least 6 weeks. Although the survival rate of
patients with metastases remains low, medical advances have led to
some differences related to tumor histology. In the present study,
ECOG-PS and MSTS scores revealed a negative correlation. Based on
these findings, it would be advisable to operate on patients with
an ECOG-PS of 3 or higher to maintain ADLs until death, regardless
of life expectancy. The authors consider the novelty of the
algorithm is its focus on deciding whether or not to operate based
on ECOG-PS, independent of life expectancy.
The present study is similar to a recent study by
the authors (31). The novelty of
the present study lies in the proposal of an algorithm for a larger
cohort that includes primary tumors. Although primary and
metastatic malignant tumors naturally exhibit different
characteristics (32), it is
considered that the algorithm proposed in the present study can be
applied to both types. Cancer rehabilitation is strongly influenced
by the local and systemic effects of the cancer itself, treatment
side effects, and physical disabilities associated with periods of
bed rest and cachexia (a state of generalized weakness due to
cancer progression) (33,34). In fact, the group with metastatic
malignant tumors, which had significantly worse ECOG-PS, also had
significantly lower MSTS scores compared with the group with
primary malignant tumors. This observation ensures the validity of
the algorithm proposed in the present study.
The current study has several limitations. First,
the sample size was small, with few cases of primary malignancies.
Comprehensive discussions have not been made. However, no problems
were encountered during statistical analyses. Second, the study's
retrospective design might have resulted in selection bias.
Finally, the follow-up period was relatively short, which is
unavoidable given the inclusion of cases with metastatic bone
tumors and associated short postoperative survival. Despite these
limitations, as numerous patients as possible were enrolled during
the study period. Future research should aim to increase the number
of cases and conduct a prospective randomized control study.
Specifically, prospective randomized cohort studies are needed with
a control group treated without the algorithm and a group treated
with the algorithm.
In conclusion, the treatment of primary and
metastatic malignant bone tumors should be based on a comprehensive
assessment of the extent of malignant tumor resection, surgical
invasiveness, and the patient's general condition and
prognosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
KH, SN, TI and KG conceptualized the study. KH, SN,
TI, RK and KG contributed to the study's methodology. KH, RK and SN
handled the software used. SN, TI, RK and KG validated the data. KH
and SN confirm the authenticity of all the raw data. SN, TI and KG
analyzed the data. KH, TI, RK, SN and KG curated the data, wrote
the original draft, and reviewed and edited the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Ethical approval for the present study was obtained
from the Ethics Committee of Kindai University Hospital (approval
no. 31-153; Osakasayama, Japan), and it was conducted in line with
the guidelines of The Declaration of Helsinki. Comprehensive
consent for the current study was obtained. Written informed
consent by individual signature was waived by the Ethics Committee
of Kindai University Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hoshi M, Iwai T, Oebisu N, Shimatani A,
Takada N and Nakamura H: Pathological fracture of a solitary bone
cyst in the calcaneus: A case series and literature review. Arch
Orthop Trauma Surg. 143:1155–1162. 2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Salunke AA, Chen Y, Tan JH, Chen X, Khin
LW and Puhaindran ME: Does a pathological fracture affect the
prognosis in patients with osteosarcoma of the extremities?: A
systematic review and meta-analysis. Bone Joint J. 96 B:1396–1403.
2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Urakawa H, Tsukushi S, Hosono K, Sugiura
H, Yamada K, Yamada Y, Kozawa E, Arai E, Futamura N, Ishiguro N and
Nishida Y: Clinical factors affecting pathological fracture and
healing of unicameral bone cysts. BMC Musculoskelet Disord.
15(159)2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fontanella C, Fanotto V, Rihawi K, Aprile
G and Puglisi F: Skeletal metastases from breast cancer:
Pathogenesis of bone tropism and treatment strategy. Clin Exp
Metastasis. 32:819–833. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Scorianz M, Gherlinzoni F and Campanacci
DA: Metastases to the long bones: Algorithm of treatment. In:
Management of bone metastases. Denaro V, Di Martino A and Piccioli
A (eds). Springer, Berlin, pp93-102, 2019.
|
|
6
|
Scully SP, Ghert MA, Zurakowski D,
Thompson RC and Gebhardt MC: Pathologic fracture in osteosarcoma:
Prognostic importance and treatment implications. J Bone Joint Surg
Am. 84:49–57. 2002.PubMed/NCBI
|
|
7
|
Chung LH, Wu PK, Chen CF, Weng HK, Chen TH
and Chen WM: Pathological fractures in predicting clinical outcomes
for patients with osteosarcoma. BMC Musculoskelet Disord.
17(503)2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hage WD, Aboulafia AJ and Aboulafia DM:
Incidence, location, and diagnostic evaluation of metastatic bone
disease. Orthop Clin North Am. 31:515–528. 2000.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Piccioli A, Spinelli MS and Maccauro G:
Impending fracture: A difficult diagnosis. Injury. 45 (Suppl
6):S138–S141. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Blagden SP, Charman SC, Sharples LD, Magee
LR and Gilligan D: Performance status score: Do patients and their
oncologists agree? Br J Cancer. 89:1022–1027. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Enneking WF, Dunham W, Gebhardt MC,
Malawar M and Pritchard DJ: A system for the functional evaluation
of reconstructive procedures after surgical treatment of tumors of
the musculoskeletal system. Clin Orthop Relat Res. 286:241–246.
1993.PubMed/NCBI
|
|
12
|
Hu YC, Lun DX and Wang H: Clinical
features of neoplastic pathological fracture in long bones. Chin
Med J (Engl). 125:3127–3132. 2012.PubMed/NCBI
|
|
13
|
Angelini A, Trovarelli G, Berizzi A, Pala
E, Breda A, Maraldi M and Ruggieri P: Treatment of pathologic
fractures of the proximal femur. Injury. 49 (Suppl 3):S77–S83.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Guzik G: Oncological and functional
results after surgical treatment of bone metastases at the proximal
femur. BMC Surg. 18(5)2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ji Y, Wu Y and Li J: Use of
three-dimensional-printed custom-made prosthesis to treat
unicondylar femoral defect secondary to pathological fracture
caused by giant cell tumor. J Int Med Res.
49(3000605211025347)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Johnson NA, Uzoigwe C, Venkatesan M,
Burgula V, Kulkarni A, Davison JN and Ashford RU: Risk factors for
intramedullary nail breakage in proximal femoral fractures: A
10-year retrospective review. Ann R Coll Surg Engl. 99:145–150.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kosygan KP, Mohan R and Newman RJ: The
Gotfried percutaneous compression plate compared with the
conventional classic hip screw for the fixation of
intertrochanteric fractures of the hip. J Bone Joint Surg Br.
84:19–22. 2002.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Willeumier JJ, van der Linden YM, van de
Sande MAJ and Dijkstra PDS: Treatment of pathological fractures of
the long bones. EFORT Open Rev. 1:136–145. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Swanson KC, Pritchard DJ and Sim FH:
Surgical treatment of metastatic disease of the femur. J Am Acad
Orthop Surg. 20:56–65. 2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Dijstra S, Wiggers T, van Geel BN and
Boxma H: Impending and actual pathological fractures in patients
with bone metastases of the long bones. A retrospective study of
233 surgically treated fractures. Eur J Surg. 160:535–542.
1994.PubMed/NCBI
|
|
21
|
Wedin R and Bauer HC: Surgical treatment
of skeletal metastatic lesions of the proximal femur:
Endoprosthesis or reconstruction nail? J Bone Joint Surg Br.
87:1653–1657. 2005.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Harvey N, Ahlmann ER, Allison DC, Wang L
and Menendez LR: Endoprostheses last longer than intramedullary
devices in proximal femur metastases. Clin Orthop Relat Res.
470:684–691. 2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Moore J, Isler M, Barry J and Mottard S:
Major wound complication risk factors following soft tissue sarcoma
resection. Eur J Surg Oncol. 40:1671–1676. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Goryń T, Pieńkowski A, Szostakowski B,
Zdzienicki M, Ługowska I and Rutkowski P: Functional outcome of
surgical treatment of adults with extremity osteosarcoma after
megaprosthetic reconstruction-single-center experience. J Orthop
Surg Res. 14(346)2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Roudier MP, True LD, Higano CS, Vesselle
H, Ellis W, Lange P and Vessella RL: Phenotypic heterogeneity of
end-stage prostate carcinoma metastatic to bone. Hum Pathol.
34:646–653. 2003.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ganesh K and Massagué J: Targeting
metastatic cancer. Nat Med. 27:34–44. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Mavrogenis AF, Pala E, Romagnoli C,
Romantini M, Calabro T and Ruggieri P: Survival analysis of
patients with femoral metastases. J Surg Oncol. 105:135–141.
2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chandrasekar CR, Grimer RJ, Carter SR,
Tillman RM, Abudu A and Buckley L: Modular endoprosthetic
replacement for tumours of the proximal femur. J Bone Joint Surg
Br. 20:108–112. 2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Saad F, Lipton A, Cook R, Chen YM, Smith M
and Coleman R: Pathologic fractures correlate with reduced survival
in patients with malignant bone disease. Cancer. 110:1860–1867.
2007.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Mirels H: Metastatic disease in long
bones. A proposed scoring system for diagnosing impending
pathologic fractures. Clin Orthop Relat Res. 249:256–264.
1989.PubMed/NCBI
|
|
31
|
Hashimoto K, Nishimura S, Ito T, Kakinoki
R and Goto K: Treatment algorithm for metastatic malignancies in
the lower extremities. Mol Clin Oncol. 21(51)2024.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Gharibi A, La Kim S, Molnar J, Brambilla
D, Adamian Y, Hoover M, Hong J, Lin J, Wolfenden L and Kelber JA:
ITGA1 is a pre-malignant biomarker that promotes therapy resistance
and metastatic potential in pancreatic cancer. Sci Rep.
7(10060)2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Mariean CR, Tiucă OM, Mariean A and Cotoi
OS: Cancer Cachexia: New insights and future directions. Cancers
(Basel). 15(5590)2023.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Law ML: Cancer cachexia: Pathophysiology
and association with cancer-related pain. Front Pain Res
(Lausanne). 3(971295)2022.PubMed/NCBI View Article : Google Scholar
|