Introduction
Metastases to the oral region (MOR) are rare and
represent 1-3% of all oral malignancies (1,2). The
occurrence of MOR is associated with unfavorable prognosis and
diminished overall survival (1-6).
The anatomical regions most affected by MOR are the posterior
mandible and, when it is in soft tissue, the gingiva (1-6).
The clinical symptoms of MOR include pain, swelling, local bleeding
due to ulceration and mass formation (4-7).
The predominant primary sites of MOR are the lung, breast and
kidney (1,4-6,8-11).
Although gastric cancer is the fourth leading cause of
cancer-associated mortality (12),
the stomach counts for only ~2.5% of all primary cancer sites
discovered in patients with MOR (5,6).
There is currently no effective treatment for cases of gastric
cancer metastasizing to the gingiva. To the best of our knowledge,
including the present case, 23 cases (13-34)
with gingival metastases from gastric cancer have been reported in
English and Japanese literature. The present study, which was
created based on the Surgical Case Report 2023 guideline (35), presents a rare case of gastric
adenocarcinoma metastasizing to the maxillary gingiva treated with
combination therapy comprising chemotherapy, tumor excision and
Radiation Therapy Oncology Group 8502 ‘QUAD shot’ radiotherapy
(RT).
Case report
A 55-year-old male was referred to the Department of
Dentistry and Oral Surgery, Tohoku Medical and Pharmaceutical
University Hospital (Sendai, Japan) to examine the gingival
swelling and the mobility of the right maxillary second molar in
December 2023. In September 2021, the patient had been diagnosed
with gastric adenocarcinoma with multiple regional lymph nodes and
liver metastases. According to the Japanese Classification of
Gastric Carcinoma 2017 (15th edition) (36), the clinical diagnosis was cT4aN2M1,
stage IVB. Although the patient exhibited hepatic dysfunction that
appeared to be associated with liver metastases, there was no other
remarkable medical history. Serum levels of carcinoembryonic
antigen (normal range, <5 ng/ml) and carbohydrate antigen 19-9
(normal range: <37 U/ml) were 2.5 ng/ml and <2 U/ml,
respectively.
The patient underwent chemotherapy at the Outpatient
Chemotherapy Center of the Department of Medical Oncology, Tohoku
Medical and Pharmaceutical University Hospital (Sendai, Japan).
Based on the Japanese Gastric Cancer Treatment Guidelines 2021 (6th
edition) (37), two cycles of
cisplatin (60 mg/m2) + tegafur-gimeracil-oteraci (80
mg/m2) was administrated as first-line treatment for
gastric cancer over a period of two months. Subsequently, the
patient received chemotherapy with second-line weekly paclitaxel
(PTX; 80 mg/m2) + ramucirumab (RAM; 8 mg/kg) for 16
cycles over a period of five months, followed by weekly
administration of nanoparticle albumin-bound PTX (100
mg/m2) + RAM (8 mg/kg) for 31 cycles for thirteen
months, third-line nivolumab (240 mg) for two cycles for one month
and fourth-line irinotecan (150 mg/m2) for three cycles
for four months. In each cycle of chemotherapy, doses were adjusted
as appropriate based on the patient condition and white blood cell
and platelet counts. However, these cancer chemotherapies were
unsuccessful.
Upon admission, the patient received chemotherapy
with trifluridine/tipiracil (FTD/TPI; 35 mg/m2) for
three cycles for 2 months. Eastern Cooperative Oncology
Group-performance status (ECOG-PS) scale (ecog-acrin.org/resources/ecog-performance-status/) was
grade 2. The swelling had grown rapidly for ~3 weeks since the
patient noticed the localized lesion and tooth mobility in October
2023. The patient also complained of frequent gingival bleeding
when eating and brushing teeth. No palpable enlarged cervical lymph
node was observed. The maximal mouth opening was 35 mm. Intraoral
examination revealed a partially necrotic tumor with exophytic
growth, ~20 mm in size, on the gingiva of the right maxillary
posterior (Fig. 1). The mobility
of the right maxillary second molar was severe.
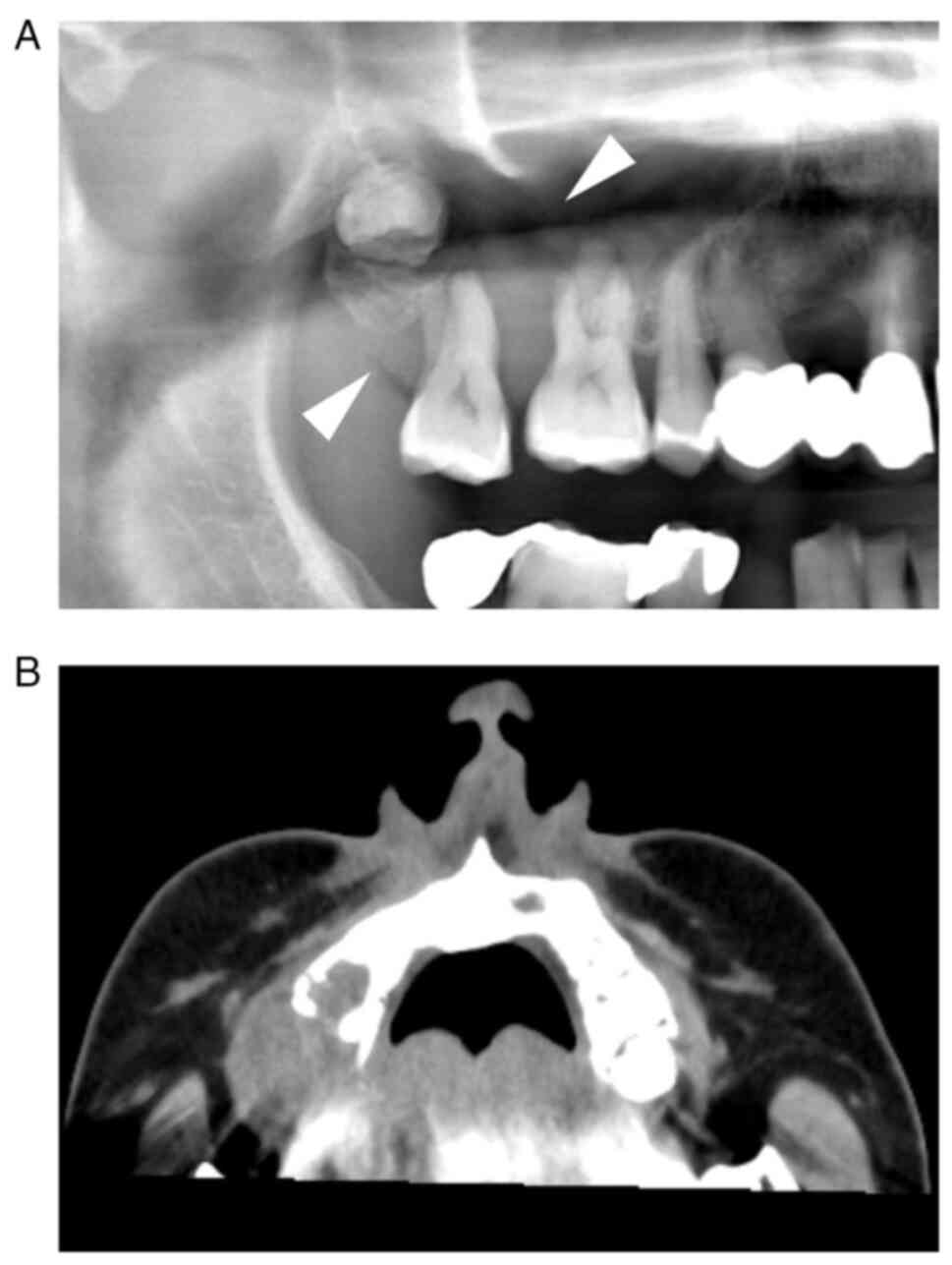
Panoramic radiography showed bone resorption around
the maxillary molar region (Fig.
2A). Computed tomography (CT; tube voltage, 120 kVp; exposure
time, 2.25 sec; scanning length, 225 s; slice thickness, 1 mm)
showed a mass with irregular bony destruction of the right side of
the posterior maxilla with soft tissue density in the maxillary
sinus (Fig. 2B). There was no
evidence of cervical lymphadenopathy. Fluorodeoxyglucose
positron-emission tomography/CT in September 2021 showed increased
accumulation in the stomach [standardized uptake value (SUV)max
6.2] with regional lymph nodes (SUVmax ~3.4) and liver (SUVmax 9.2
and 9). On the other hand, there was no accumulation in the oral
region (Fig. 3).
Due to rapid growth of the gingival tumor, which was
often accompanied by local hemorrhage, the patient underwent
surgical excision of the gingival tumor with concomitant removal of
the right maxillary second molar to decrease symptoms in December
2023. The procedure was performed while the patient was receiving
chemotherapy with FTD/TPI.
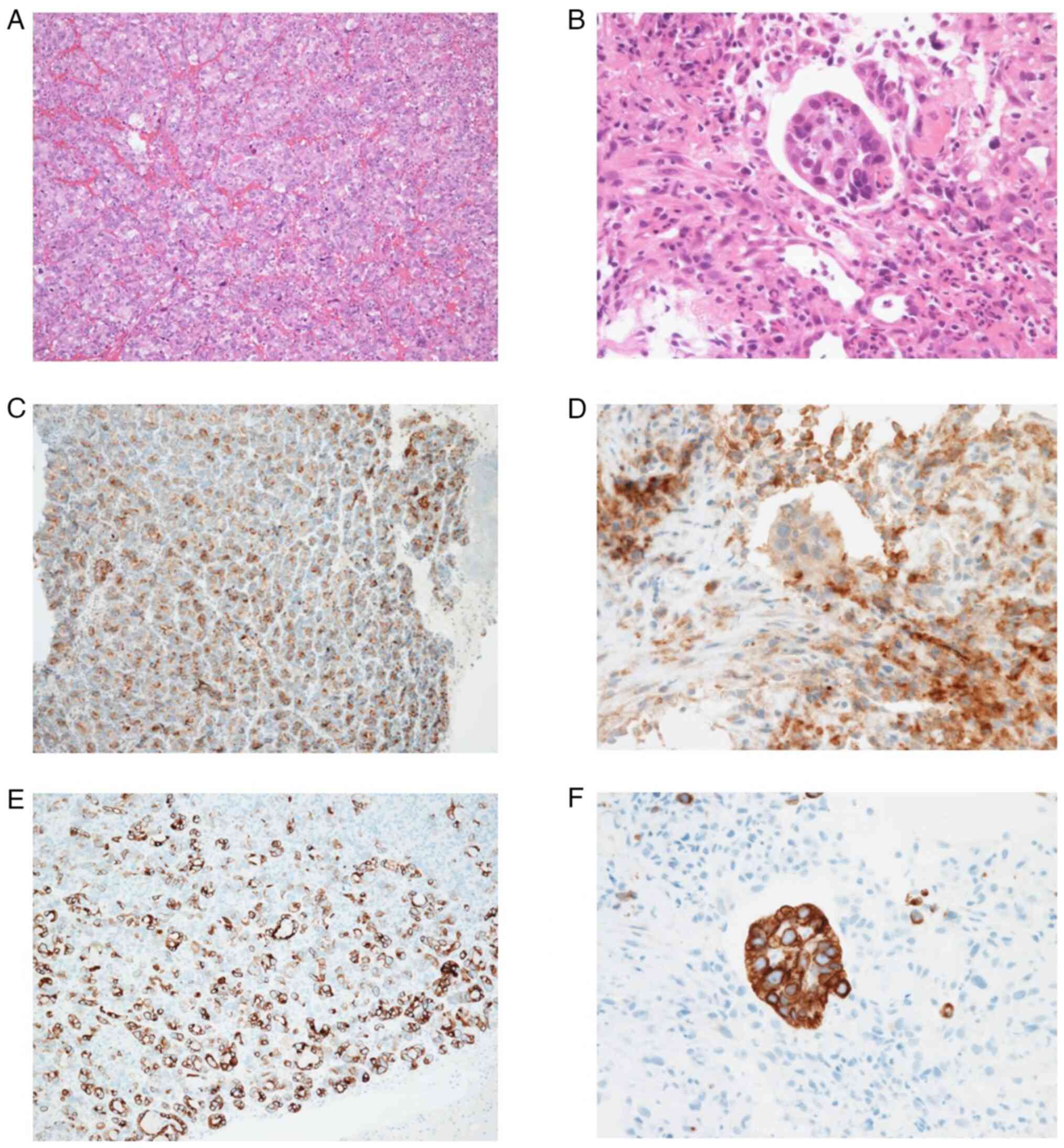
The tissue samples of the gastric cancer and the
gingival tumor were fixed in 10% formalin neutral buffer solution
and embedded in paraffin. Histological sections with a thickness of
4 µm were stained with hematoxylin and eosin (H&E) and
immunohistochemistry using Tissue-Tek Prisma Plus Automated Slide
Stainer (Sakura Finetek Japan Co., Ltd.) and VENTANA BenchMark
ULTRA system (Roche Diagnostics K.K), respectively. The sections
were incubated with rabbit antibody against CD10, CK7 and CK20 and
with mouse antibody against MUC (mucin) 2, MUC5AC and MUC6. H&E
staining of the specimens from gingival tumors (Fig. 4A) and gastric cancer (Fig. 4B) demonstrated poorly
differentiated adenocarcinoma. Immunohistochemical expression of
human epidermal growth factor receptor 2 in gastric cancer was
negative. Immunohistochemistry showed that both specimens were
positive for CD10 (Fig. 4C and
D) and CK7 (Fig. 4E and F) but negative for CK20, MUC2, MUC5AC and
MUC6. These pathological findings revealed metastatic
adenocarcinoma of maxillary gingiva that was consistent with a
gastric cancer origin.
Although no bleeding from the tumor was reported
since the procedure was completed, RT was planned to inhibit tumor
regrowth. At 2 weeks following the surgical excision, the gingival
tumor showed growth and the patient was treated with one cycle of
palliative QUAD shot RT immediately. A total of two daily fractions
of 3.5 Gy was delivered with an interval of ≥6 h for 2 consecutive
days, totaling 14 Gy over four fractions. After that, there was no
progression of maxillary gingival metastatic lesion and the patient
was capable of oral intake. However, the patient died of multiple
organ failure caused by systemic metastases 3 months following the
diagnosis of maxillary gingival metastasis originating from gastric
cancer.
Discussion
The incidence of gingival metastasis originating
from gastric cancer is rare. English literature in PubMed
(pubmed.ncbi.nlm.nih.gov/), Scopus
(https://www.scopus.com/) and Google
Scholar(scholar.google.com/) and Japanese
literature in J-Stage (jstage.jst.go.jp/) were searched without date limit.
The keywords ‘oral region’, ‘gastric cancer’ and ‘metastasis’ were
searched in the title/abstract of publications. Studies cited by
the review of Wu et al (32) and references of the included
articles were also searched (Table
I).
 | Table ICases with gingival metastasis
originated from gastric cancer. |
Table I
Cases with gingival metastasis
originated from gastric cancer.
| First author,
year | Age/sex | Gingival site | Duration between
primary gastric cancer and gingival meta | Other
metastasis | Treatment | Vital status,
time | (Refs.) |
|---|
| Lund et al,
1968 | 63/F | Mand | Synchronous | + | S | Died, 2 months | (13) |
| Astacio et
al, 1969 | 58/M | Mand | Synchronous | ND | C | Died, 4 months | (14) |
| Ohba et al,
1974 | 51/M | Mand | Synchronous | + | RT | Died, 7 months | (15) |
| Lopez et al,
1976 | 65/F | Maxi | Before primary, 3
weeks | + | - | Died, ND | (16) |
| Osaki et al,
1978 | 59/M | Maxi | ND | ND | S | ND | (17) |
| Tojo et al,
1989 | 69/M | Mand | ND | ND | C | Died, 5 months | (18) |
| Hamakawa et
al, 1993 | 56/M | Mand | ND | + | S | Died, 4 months | (19) |
| Florio et
al, 1995 | 66/M | Maxi | After primary, 3
months | - | RT | Died, ND | (20) |
| Makino et
al, 1997 | 60/M | Mand | ND | ND | C | Died, 4 months | (21) |
| Yajima et
al, 1999 | 65/M | Maxi | ND | - | S | ND | (22) |
| Shimoyama et
al, 2004 | 56/M | Mand | After primary, 15
months | + | - | Died, 3 months | (23) |
| Colombo et
al, 2005 | 61/F | Maxi | Before primary, 7
months | - | C, RT | Died, 15
months | (24) |
| Kwon et al,
2006 | 65/M | Mand | Synchronous | - | - | Died, 3 months | (25) |
| Nishide et
al, 2006 | 82/F | Mand | After primary, 4
years | + | S | ND | (26) |
| Hwang et al,
2007 | 58/M | Maxi | After primary, 4
years | + | C | ND | (27) |
| Uchiyama et
al, 2009 | 73/F | Mand | After primary, 10
months | + | C, RT | Died, 9 months | (28) |
| Suaerbom et
al, 2011 | 70/M | Mand | After primary, 3
months | + | S | Died, 3 months | (29) |
| Guo et al,
2012 | 62/F | Mand | After primary, 2
years | + | - | Died, 6 months | (30) |
| Kalaitsidou et
al, 2015 | 71/M | Mand | After primary, 2
years | ND | S | ND | (31) |
| Wu et al,
2017 | 75/M | Maxi | After primary, 2.5
years | + | C, RT | Alive, 9
months | (32) |
| Soares et
al, 2018 | 43/M | Mand | Before primary,
ND | ND | C, RT | Died, 3 months | (33) |
| Ayşegu et
al, 2018 | 54/M | Maxi | Before primary,
ND | + | S, C | Died, 5 months | (34) |
| Present case,
2023 | 55/M | Maxi | After primary, 2
years | + | C, S, RT | Died, 3 months | |
To the best of our knowledge, 23 cases including the
present case have been reported to date in English and Japanese
literature. Among these, ~43% (10/23 cases) were reported in Japan,
indicating that such cases are more common compared with in other
countries. This tendency may be due not only to advances in
multimodal therapies globally but also from the progression of the
Japanese super-aging society (5).
The present case exhibits features which align with
those from previous reports: MOR is primarily observed in elderly
patients, with a mean age of 57 years (5,6). The
patient in the present case was 55-years-old, consistent with this
age distribution. Secondly, the location of the MOR was the
maxillary molar gingiva, a common site for gingival metastasis
(4-6).
In soft tissue, the attached gingiva is the most affected site
because of chronic inflammation due to periodontitis (1,2,4,32).
Allon et al (38) reported
that in dentulous patients with gingival metastasis, metastatic
foci were adjacent to teeth and the presence of teeth was
significantly associated with gingival metastasis. When teeth are
present, chronic inflammation may provide a niche for metastases
(2,38,39).
Shimono et al (5) suggested
that chronic inflammation such as gingivitis causes MOR and
gingival metastasis is likely to occur in the attached gingiva of
remaining teeth. In the present case, the metastatic lesion was
attached to the gingiva of the right maxillary molar. Thirdly,
metastatic foci of the oral region sometimes show rapid growth
(7,32). Here, gingival tumor presented as a
nodule with local hemorrhage and enlarged rapidly within a month.
Fourthly, MOR is typically accompanied by metastases of other sites
(7,32,40).
In the present case, gastric cancer was already accompanied by
metastases of multiple lymph nodes and liver at first examination.
Finally, prognosis of patients with MOR is poor and ~70% of
patients die within 1 year of diagnosis of MOR (4). A review showed that the range of the
mean time between the diagnosis of MOR and death is 7.5-9.8 months
(5). In cases of gingival
metastasis from gastric cancer, ~60% of patients die within 6
months of diagnosis (32). In the
present case report, although the patient was treated with
combination therapy, he died 3 months following diagnosis of
maxillary gingival metastasis.
Chemotherapy alone, with palliative intent, is
utilized in ~40% of patients with MOR and ~30% of the cases are
treated with combination therapy (5). For the treatment of gingival
metastasis from gastric cancer, ~30% (7/23) of cases underwent
surgical excision only (13,17,19,21,26,29,31)
and 17% (4/23) of cases received chemotherapy alone (14,18,21,27).
On the other hand, 26% (6/23) of cases were treated with
combination therapy: 17% (4/23) received chemotherapy and RT
(24,28,32,33),
4% (1/23) underwent surgery and chemotherapy (34), and one patient (4%) case underwent
chemotherapy, tumor excision and RT. However, 12/23 (52%) of cases
resulted in patient death within 6 months (13-34).
Despite treatment modalities, there is currently no effective
treatment for patients with MOR. Treatment for MOR primarily
focuses on improving patient quality of life (QOL) or prognosis
through palliative care (2-5).
Before treating MOR, it is necessary to evaluate the following
factors: i) Patient prognosis; ii) patient condition, including
ECOG-PS score; iii) existence of oral dysfunction or symptom; iv)
whether the primary tumor is under control; v) progress of
metastatic foci of the oral region and vi) patient will and
intention in a multidisciplinary team approach.
Radiation Therapy Oncology Group 8502 ‘QUAD shot’,
which is a hypofractionated RT technique for palliative treatment,
involves 2 days of twice-daily fractionation with a fraction size
of 3.0-3.7 Gy (14.0-14.8 Gy/cycle). If possible, this regimen is
repeated at 3-6-week intervals for a total of three cycles with an
RT dose of 44.4 Gy (41,42). QUAD shot has been widely adopted
for palliative treatment in patients with head and neck cancer
(HNC) due to superior response rate, palliation, mild adverse
effects and minimizing physical and social burdens (41-43).
The National Comprehensive Cancer Network guidelines recommend the
QUAD shot regimen as a palliative RT care for HNC (44).
Due to rapid growth of the gingival tumor and
associated local hemorrhage in the present case, tumor excision was
performed in addition to chemotherapy. This approach was used to
alleviate these symptoms rather than completely cure the gingival
metastatic lesion. The patient received one cycle of palliative
QUAD shot. After that, there was no tumor progression or local
hemorrhage and the patient was capable of oral intake. However, the
patient died of systemic metastasis after 3 months following
diagnosis of maxillary gingival metastasis originating from gastric
cancer.
The lesions of MOR are treatment-resistant and often
demonstrate rapid progression. Moreover, lesions frequently lead to
various symptoms and dysfunctions such as local hemorrhage, pain,
hypoesthesia, difficulty in oral intake, dysphagia and airway
compromise (5,8,45).
Most lesions of MOR are reported as nodules, with ~64% of cases
being symptomatic (5). For these
reasons, MOR should be managed to alleviate symptoms and improve or
maintain patient QOL.
In the future, the number of patients with MOR is
expected to increase (4,6). The presence of MOR is rarely found
while treating the primary tumor and clinical symptoms appear in
advanced stages. Physicians should check the symptoms of the oral
region and perform screening during cancer therapy. The present
study reported a case of maxillary gingival metastasis originating
from gastric cancer and summarized relevant literature. The
prognosis of MOR is usually unfavorable. It is important to detect
MOR as early as possible to facilitate appropriate treatment. If
there are opportunities to improve patient QOL or prognosis,
physicians should develop treatment strategies with
interdisciplinary teams. Combination therapy, including
chemotherapy, immunotherapy, surgery and RT, such as QUAD shot,
should be considered.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by Japan Society for
the Promotion of Science KAKENHI Grant-in-Aid for Scientific
Research (grant no. 23K09389).
Availability of data and materials
The data generated in the present study are not
publicly available due to patient confidentiality but may be
requested from the corresponding author.
Authors' contributions
HM designed the study, wrote the manuscript and
performed the literature review. HM, MS, and FS collected and
analyzed the data and prepared figures and tables. HS, CK, MN, YI,
ST and KM supervised the study, analyzed data and edited the
manuscript. HM, HS, CK, MN, YI and ST confirm the authenticity of
all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
This case report was approved by Ethics Committee of
Tohoku Medical and Pharmaceutical University Hospital (approval no.
2023-4-074).
Patient consent for publication
The patient provided written informed consent for
publication of the case report and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hirshberg A and Buchner A: Metastatic
tumours to the oral region. An overview. Eur J Cancer Part B Oral
Oncol. 31B:355–360. 1995.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hirshberg A, Shnaiderman-Shapiro A, Kaplan
I and Berger R: Metastatic tumours to the oral cavity-pathogenesis
and analysis of 673 cases. Oral Oncol. 44:743–752. 2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hirshberg A, Berger R, Allon I and Kaplan
I: Metastatic tumors to the jaws and mouth. Head Neck Pathol.
8:463–474. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kirschnick LB, Schuch LF, Cademartori MG
and Vasconcelos ACU: Metastasis to the oral and maxillofacial
region: A systematic review. Oral Dis. 28:23–32. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Shimono H, Hirai H, Oikawa Y, Mochizuki Y,
Kuroshima T, Tomioka H, Kayamori K, Ikeda T and Harada H:
Metastatic tumors in the oral region: A retrospective chart review
of clinical characteristics and prognosis. Oral Surg Oral Med Oral
Pathol Oral Radiol. 132:648–652. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kirschnick LB, Schuch LF, Gondak R, Rivero
ERC, Gomes APN, Etges A, Tarquinio SBC, Mesquita RA, Caldeira PC,
da Costa AAS, et al: Clinicopathological features of metastasis to
the oral and maxillofacial region-multicenter study. Head Neck
Pathol. 17:910–920. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kajita T, Miyashita H, Kitamura J,
Kouketsu A, Kumamoto H and Takahashi T: Pulmonary pleomorphic
carcinoma metastasizing to the anterior mandibular gingiva: A case
report and literature review. Int J Surg Case Rep.
98(107499)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zachariades N: Neoplasms metastatic to the
mouth, jaws and surrounding tissues. J Craniomaxillofac Surg.
17:283–290. 1989.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Maschino F, Guillet J, Curien R, Dolivet G
and Bravetti P: Oral metastasis: A report of 23 cases. Int J Oral
Maxillofac Surg. 42:164–168. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jham BC, Salama AR, McClure SA and Ord RA:
Metastatic tumors to the oral cavity: A clinical study of 18 cases.
Head Neck Pathol. 5:355–358. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Owosho AA, Xu B, Kadempour A, Yom SK,
Randazzo J, Ghossein RA, Huryn JM and Estilo CL: Metastatic solid
tumors to the jaw and oral soft tissue: a retrospective clinical
analysis of 44 patients from a single institution. J
Craniomaxillofac Surg. 44:1047–1053. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Thrift AP, Wenker TN and El-Serag HB:
Global burden of gastric cancer: Epidemiological trends, risk
factors, screening and prevention. Nat Rev Clin Oncol. 20:338–349.
2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lund BA, Moertel CG and Gibilisco JA:
Metastasis of gastric adenocarcinoma to oral mucosa. Oral Surg Oral
Med Oral Pathol. 25:805–809. 1968.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Astacio JN and Alfaro C: Oral mucosa
metastasis from gastric adenocarcinoma. Oral Surg Oral Med Oral
Pathol. 28:859–861. 1969.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ohba T, Nakagawa E and Nakata H:
Metastatic tumor of the gum. Jpn J Cancer Clin. 20:692–696.
1974.
|
|
16
|
Lopez N and Lobos N: Metastatic
adenocarcinoma of gingiva. Report of a case. J Periodontol.
47:358–360. 1976.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Osaki T, Ryoke K and Hamada T: Metastatic
adenocarcinoma to the oral cavity: report of two cases and review
of literature. Jpn J Stomatol Soc. 27:173–185. 1978.
|
|
18
|
Tojyo Y, Saito K, Aihara H, Tuda Y and
Nisimaru Y: The metastasis of gastric adenocarcinoma to the gingiva
of the mandible-review of the Japanese literature. Gan No Rinsho.
35:1165–1170. 1989.PubMed/NCBI(In Japanese).
|
|
19
|
Hamakawa H, Takarada M and Tanioka H: Two
metastatic tumors of the oral cavity: A histopathologic
investigation. J Oral Surg Society Jpn. 39:823–828. 1993.
|
|
20
|
Florio SJ and Hurd TC: Gastric carcinoma
metastatic to the mucosa of the hard palate. J Oral Maxillofac
Surg. 53:1097–1098. 1995.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Makino S, Omura K and Kitada H: Metastatic
mandibular tumor: Report of 7 cases. Jpn J Oral Maxillofac Surg.
43:465–472. 1997.
|
|
22
|
Yajima M and Miyazaki T: Metastasis of
gastric adenocarcinoma to the maxillary gingiva: Report of a case.
Jpn J Oral Maxillofac Surg. 45:497–499. 1999.
|
|
23
|
Shimoyama S, Seto Y, Aoki F, Ogawa T, Toma
T, Endo H, Itouji T and Kaminishi M: Gastric cancer with metastasis
to the gingiva. J Gastroenterol Hepatol. 19:831–835.
2004.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Colombo P, Tondulli L, Masci G, Muzza A,
Rimassa L, Petrella D and Santoro A: Oral ulcer as an exclusive
sign of gastric cancer: Report of a rare case. BMC Cancer.
5(117)2005.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kwon MS, Ko SO, Cho NP, Kim OH, Shin HK,
Baek JA and Leem DH: Gastric signet-ring cell adenocarcinoma
metastatic to the gingiva: A case report. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 102:62–66. 2006.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Nishide N and Kanamura N: The value of
carcinoembryonic antigen staining to determine the primary
malignancy in metastatic carcinoma to the gingiva. Am J Clin Oncol.
29:316–317. 2006.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hwang KG, Park CJ, Paik SS and Shim KS:
Gingival metastasis from gastric adenocarcinoma. Otolaryngol Head
Neck Surg. 137:169–170. 2007.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Uchiyama Y, Murakami S, Kakimoto N,
Nakatani A, Kishino M, Hamab Y and Furukawa S: Diagnostic imaging
findings for mandibular metastasis from gastric adenocarcinoma.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 107:e49–e53.
2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sauerborn D, Vidakovic B, Baranovic M,
Mahovne I, Danic P and Danic D: Gastric adenocarcinoma metastases
to the alveolar mucosa of the mandible: A case report and review of
the literature. J Craniomaxillofac Surg. 39:645–648.
2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Guo Y, Chen DF, Li P and CH L: Gingival
metastasis from gastric cancer: 1 case report. Chin J Gastmenterol.
17(384)2012.
|
|
31
|
Kalaitsidou IG, Astreidis IT, Kontos KI,
Lazaridou MN, Bourlidou ET, Gerasimidou DK, Vladika NP and Mangoudi
DL: Metastatic tumours to the oral cavity: Report of three cases. J
Oral Maxillofac Res. 6(e5)2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Wu Z, Tang J, Li Y, Lu H, Xu J and Lv D:
Successful management of rare gingival metastasis from gastric
adenocarcinoma: A case report and literature review. World J Surg
Oncol. 15(141)2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Soares CD, Rocha BA, Paranaiba LMR, de
Melo-Filho MR, Jorge J, de Carvalho MGF and de Almeida OP: A
challenging diagnosis: Case report of oral metastasis from gastric
adenocarcinoma mimicking pyogenic granuloma. Medicine (Baltimore).
97(e9934)2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Ayşegul A, Ahmet K, Abdullah Y, Merva ST
and Sidar B: Gastric carcinoma metastases to the anterior maxilla:
A rare case report. Int J Oral Med Sci. 17:129–132. 2018.
|
|
35
|
Sohrabi C, Mathew G, Maria N, Kerwan A,
Franchi T and Agha RA: Collaborators. The SCARE 2023 guideline:
Updating consensus Surgical CAse REport (SCARE) guidelines. Int J
Surg. 109:1136–1140. 2023.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Japanese Gastric Cancer Association.
Japanese Classification of Gastric Carcinoma 2017. 15th edition.
Kanehara Shuppan, Tokyo, 2017.
|
|
37
|
Japanese Gastric Cancer Association:
Japanese gastric cancer treatment guidelines 2021. 6th edition.
Gastric Cancer. 26:1–25. 2023.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Allon I, Pessing A, Kaplan I, Allon DM and
Hirshberg A: Metastatic tumors to the gingiva and the presence of
teeth as a contributing factor: A literature analysis. J
Periodontol. 85:132–139. 2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Irani S: Metastasis to the oral soft
tissues: A review of 412 cases. J Int Soc Prev Community Dent.
6:393–401. 2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ellis GL, Jensen JL, Reingold IM and Barr
RJ: Malignant neoplasms metastatic to gingivae. Oral Surg Oral Med
Oral Pathol. 44:238–245. 1977.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Lok BH, Jiang G, Gutiontov S, Lanning RM,
Sridhara S, Sherman EJ, Tsai CJ, McBride SM, Riaz N and Lee NY:
Palliative head and neck radiotherapy with the RTOG 8502 regimen
for incurable primary or metastatic cancers. Oral Oncol.
51:957–962. 2015.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Toya R, Saito T, Yamaguchi K, Matsuyama T,
Watakabe T, Matsumoto T, Yoshida R, Hirosue A, Murakami D, Orita Y,
et al: Hypofractionated palliative volumetric modulated arc
radiotherapy with the radiation oncology study group 8502 ‘QUAD
shot’ regimen for incurable head and neck cancer. Radiat Oncol.
15(123)2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Takahashi S, Endo M, Nagatomo T, Onaga R,
Yamaguchi H, Yamamoto R, Fukuda Y, Ogawa K, Nakamura M, Okada K, et
al: Successful preoperative QUAD SHOT for bulky parotid carcinoma:
Potential preoperative ultra-hypofractionated radiotherapy for
conversion surgery. Case Rep Oncol. 16:218–226. 2023.PubMed/NCBI View Article : Google Scholar
|
|
44
|
National Comprehensive Cancer Network:
NCCN Clinical Practice Guidelines in Oncology, Head and Neck
Cancers (version 1). 2020.
|
|
45
|
Lee YH and Lee JI: Metastatic carcinoma of
the oral region: An analysis of 21 cases. Med Oral Patol Oral Cir
Bucal. 22:e359–e365. 2017.PubMed/NCBI View Article : Google Scholar
|