Introduction
Hirschprung's disease is a congenital disease of
intestinal motility characterized by the the absence of ganglion
cells (aganglionosis) in the myenteric plexus of Auerbach and in
the submucosal plexus of Meissner. It extends a variable distance
in the colon and arises secondary to a failure in the migration of
ganglion cells from the neural crest during embryonic development
(1). Although Hirschsprung's disease
may have a polygenic influence, the gene most frequently involved
is the RET proto-oncogene (2,3).
Hirschsprung's disease can be classified according to aganglionic
extension into ultra-short segment, short segment, long segment and
total colonic aganglionosis (4). Its
estimated incidence is 1 in 5,000 newborns, and it is a common
cause of intestinal obstruction in newborns and children. Clinical
manifestations and diagnosis occur prior to 5 years of age in
>90% of cases. However, patients with mild forms of the disease
may reach adulthood before the diagnosis is established (5). In adults, the diagnosis of
Hirschsprung's disease can only be established after the age of 10
years. There are several case reports describing adults and as it
is often missed or misdiagnosed, there is no estimated incidence in
adults (4-6).
The usual age gap for diagnosis in adults is between 20 and 40
years, with a higher prevalence in males (4,6,7). The present study describes the case of
a 20-year-old male patient, with a history of chronic constipation
since childhood managed conservatively.
Case report
A 20-year-old male patient, without a prior medical
history, apart from multiple childhood non-relevant and unspecific
episodes of constipation, which resolved spontaneously, was
admitted to Hospital Angeles Chihuahua (Chihuahua, Mexico). During
anamnesis, the patient reported an insidious onset of constipation
episodes during his pre-school years. He also reported previous
satisfactory resolution by intermittently treatment with
Plantago ovata (psyllium), laxatives and prokinetics.
Therefore, the patient proceeded to self-medicate with the same
treatment as necessary, delaying his diagnostic process. Currently,
the individual reported absent bowel movements for a duration of 1
week. He also complained that the use of laxatives and enemas had
been unsuccessful. At the time of his examination, the symptoms of
the patient included anorexia, nausea, biliary emesis and diffuse
intractable colicky abdominal pain. Upon a physical examination, a
distended abdomen with tenderness to palpation was noted.
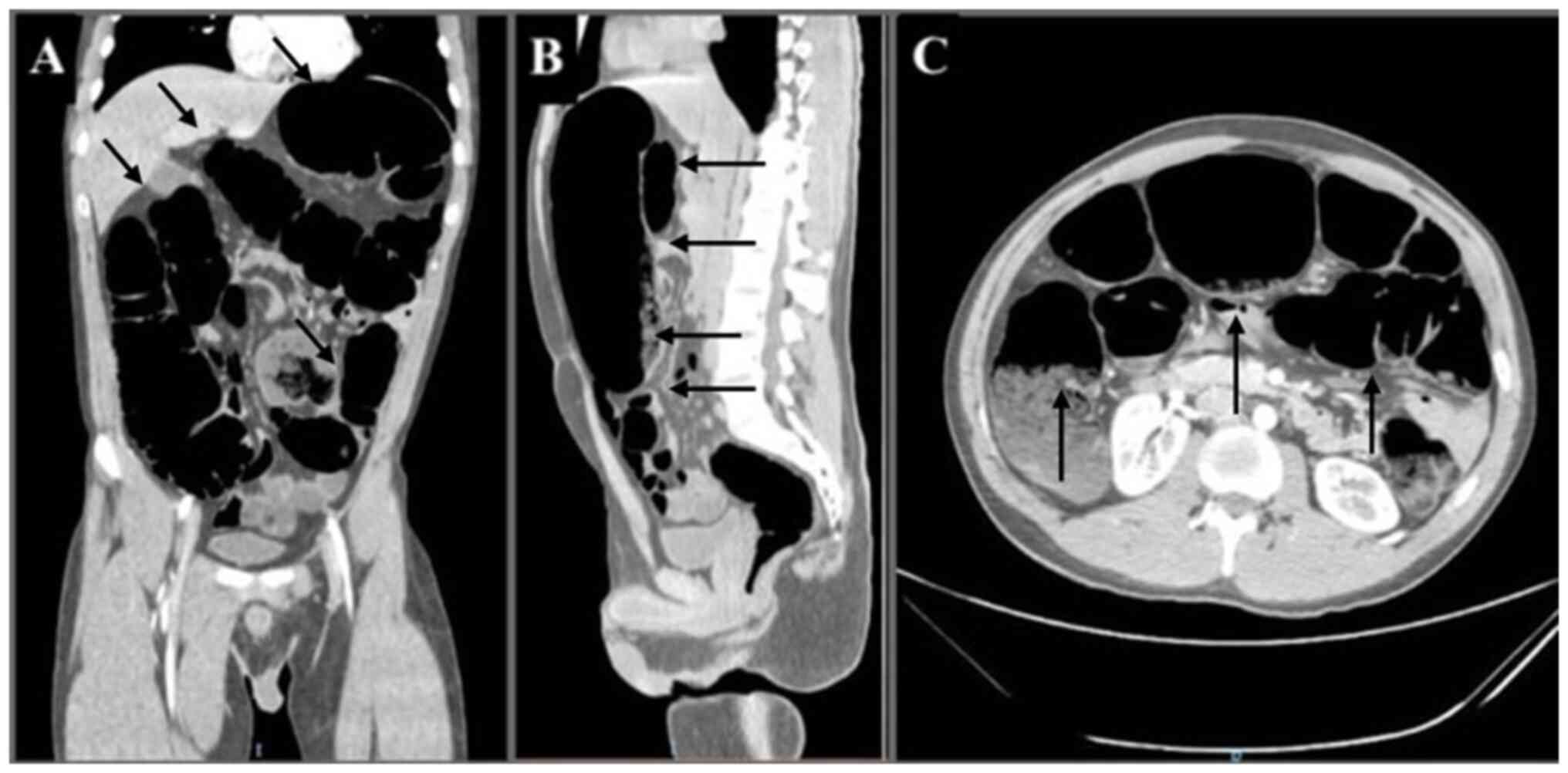
Therefore, volvulus was suspected and thus, an abdominal X-ray
(Fig. 1), and 1 h later an abdominal
computed tomography (CT) scan with intravenous contrast were
performed (Fig. 2). Following
imaging evaluation, emergency surgical intervention was performed
due to the risk of bowel perforation.
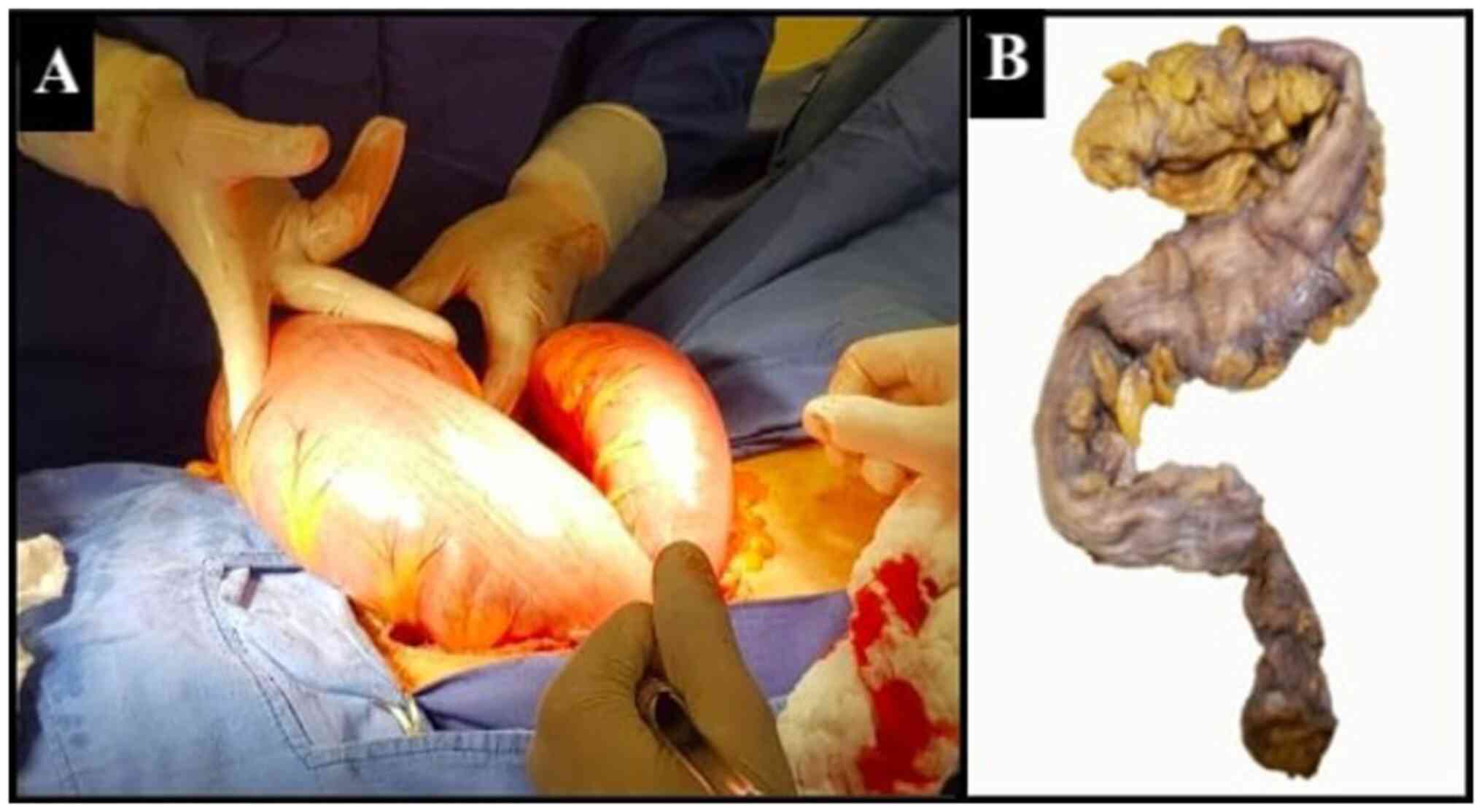
An exploratory laparotomy was performed, at which
time no volvulus was found, and a sigmoid colon distention of 11 cm
in diameter was noted (Fig. 3).
Seromuscular biopsies were obtained at the descending and sigmoid
colon junction, as well as at the sigmoid colon with fragments of
the muscular layer. A colostomy was then performed at the
descending and sigmoid junction of the colon (8). The samples obtained were processed
using 10% buffered formalin, then embedded in paraffin and
sectioned into 50-µm-thick slices using a microtome. The sections
were placed on slides and stained with hematoxylin and eosin. These
procedures were performed at the Cytopathology and Oncological
Pathology laboratory, Histopath®, in accordance with
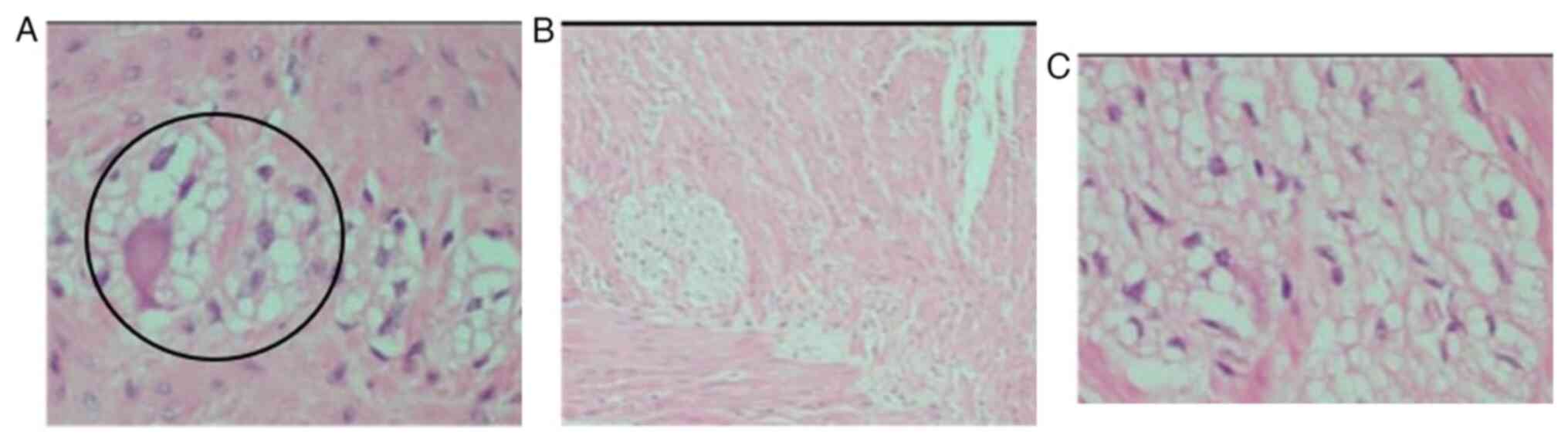
standard guidelines. The pathology report of the biopsies described
the absence of ganglion cells in the myenteric plexus in all the
biopsied segments, diagnosing adult Hirschsprung's disease. The
patient was subjected to surgery for a second time, at which time
Soave's procedure was utilized for colon descent with rectal
anastomosis and the resection of the dysfunctional sigmoid colon,
and a terminal ileostomy was performed (9). The subsequent histopathological
diagnosis confirms the aganglionosis and hypoganglionosis of the
sigmoid colon in its last 6 cm, confirming the diagnosis of
short-segment adult Hirschprung's disease (Fig. 4). At 2 months following Soave's
procedure, a follow-up with a colonoscopy was performed to assess
the integrity of the colo-anal anastomosis, where no openings,
ulcers, or signs of fistulization were evident. Finally, a third
surgery was performed for ileostomy closure (10). Following an uncomplicated
post-operative course, the patient was discharged from the
hospital. The patient remains uncomplicated at 40 months of
follow-up with no difficulty in achieving bowel movements.
Discussion
Hirschsprung's disease can be classified according
to the length of the aganglionic colon from the internal anal
sphincter. It is divided into an ultra-short segment when it
affects only the internal anal sphincter and <5 cm of the distal
rectum, a short segment when the aganglionosis extends to the
sigmoid colon (75-80% of cases) (as in the case in the present
study), a long segment when the absence of ganglion cells extends
beyond the rectosigmoid junction to the splenic flexure or
transverse colon (15-20%) and total colonic aganglionosis,
affecting the entire colon and less than 50 cm of the ileum (2-13%)
(4,11,12).
Of note, >90% of cases are diagnosed in the
neonatal period, with suspicion beginning following a delay in
meconium elimination for >24 h (13). However, patients with mild forms of
the disease may reach adulthood prior to diagnosis, as it is
commonly overlooked during medical evaluations and can be masked by
effective management of constipation (6,14). The
diagnosis of Hirschsprung's disease in adults is relatively
difficult compared with that in children, largely due to its
infrequency, and the fact that it usually involves short or
ultra-short aganglionic segments, which produce mild symptoms that
can be managed effortlessly (11).
It is estimated that ~2% of cases of chronic constipation in adults
could be secondary to Hirschsprung's disease (5). As the causes of chronic constipation
can be multifactorial, it is critical to make differential
diagnoses and exclude other causes of chronic constipation and
megacolon in adults, such as: Colorectal cancer, volvulus,
iatrogenic causes, enteric neuropathies, stenosis, colonic motility
slowing, Chagas disease, anatomical or functional (endocrine or
metabolic disorders) obstruction to defecation or idiopathic
megacolon (11,15).
In addition, since the most important
etiopathogenetic factor in the development of Hirschsprung's
disease is a neuronal disorder, this pathology can be classified as
an intestinal neuropathy (16). The
clinical presentation of intestinal neuropathies varies
significantly according to the degree of biochemical disruption,
neuronal connectivity and cell density present in the enteric
ganglia (17). Sometimes, in
Hirschsprung's disease, the distinction between innervated and
aganglionic segments is not well-defined. As a result, transitional
zones can exist where the cellular density and characteristics of
the ganglia exhibit considerable variability. These incomplete
enteric ganglia contribute to the formation of hybrid structures,
leading to greater heterogeneity in the clinical manifestations of
Hirschsprung's disease. This variability in ganglion cell density
may further complicate the histopathological diagnosis of the
condition (18). Indeed, apart from
cases of complete aganglionosis in Hirschsprung's disease, the
degree of neuronal dysfunction or the phenotype of the pathology
directly depends on the genetic and epigenetic interactions of the
patient. In a number of instances, there are groups of immature or
inactive neurons in the colonic plexuses, which may either activate
or deactivate, thereby exacerbating or alleviating the symptoms of
the disease depending on various environmental factors (19).
As there is a wide array of differential diagnoses
in adults, and the onset of symptoms can also occur at a late stage
and be minimal, a high index of suspicion and a detailed history of
constipation characteristics since childhood are required. The most
common initial presentation of Hirschsprung's disease in adults
consists of insidious and intermittent episodes of constipation of
variable duration, bloating and abdominal pain (4,6,7). Adults mostly seek medical consultation
for chronic refractory constipation from childhood onwards,
complaints of abdominal pain and distension, and regular use of
laxatives or enemas. This disease is frequently misdiagnosed in
adults as chronic constipation without conclusive analyses, as
constipation is the most common symptom in this population with a
prevalence of 10 to 15%. Late diagnoses are particularly associated
with short segments (<10 cm in length) or when symptoms are
attenuated by the chronic use of laxatives, a low-residue diet,
antispasmodics and other treatments (13). Evidence of this has been previously
reported in the literature. There is a documented case of a
9-year-old patient with Hirschsprung's disease, who was diagnosed
only at that age due to having bowel movements approximately every
3 to 4 days. At the same time, the patient exhibited a favorable
response to the use of laxatives and prokinetics (20). Similarly, a 19-year-old Caucasian
woman with a chronic history of constipation, managed daily with
enemas and laxatives, was diagnosed with Hirschsprung's disease at
a later stage. The diagnosis was confirmed through a biopsy of the
colonic tissue, which revealed residual neuronal tissue (5).
However, as in the case described herein, the
presentation of Hirschsprung's disease in some adults can be acute,
requiring laparotomy and rapid surgical management due to overlying
intestinal occlusive syndrome (4,7,6,21).
Although there are well-established tests for the diagnosis of
Hirschsprung's disease, due to the rarity of its occurrence in
adults, these are rarely performed. Nevertheless, when
Hirschsprung's disease is suspected in an adult, the same tests
performed in pediatric patients can also be performed in adults.
Some of these tests include plain abdominal radiographs, contrast
enema, anal manometry and full-thickness rectal biopsies (5,9,22). An initial assessment can be performed
with simple abdominal radiography, where a grossly distended colon,
the abnormal distribution of intestinal gas and the absence of
stool in the rectum could be observed (9,23).
The most effective imaging method to assess
Hirschsprung's disease is contrasted enema (sensitivity, 70%;
specificity, 83%), in which an observable transition sign (the
narrow zone proximal to the anus, funnel-shaped transition zone and
dilated zone correspond to the aganglionic, hypoganglionosis and
normal ganglionic zones, respectively) is the most important
criterion to help confirm a suspicion for Hirschsprung's disease
(24). Anorectal manometry is
another study modality with high sensitivity (91%) and specificity
(93%) that can be used to evaluate suspected cases. It consists of
rectal distension using a pressure-controlled balloon with the
subsequent measurement of contraction/relaxation of the interior
and exterior anal sphincters. An abnormal test consistent with
Hirschsprung's disease is a failure of the internal anal sphincter
to relax after rectal distension (23,25).
However, despite all the tests available, the gold standard for a
definitive diagnosis is a histopathological analysis. The diagnosis
of Hirschsprung's diseases is made when the absence of ganglion
cells and submucosal nerve hypertrophy are found (4,5,23,25).
Definitive treatment is surgical and is focused on
elimination of the aganglionic segment of the colon with subsequent
anastomosis distal to the affected area (1,22). There
are different surgical techniques to treat Hirschsprung's disease
in adults; however, when selecting one, the decision should be
individualized based on the clinical status of the patient and the
classification according to the length of the affected segment
(26). Fecal diversion procedures
(e.g., colostomy) tend to be applied to older patients and with an
American Society of Anesthesiologists (ASA) score of ≥3, which
probably explains a higher incidence of post-operative
complications, pre-operative gastrointestinal organic lesion and
the duration of obstruction. On the other hand, patients who
underwent an intestinal continuity restoration technique were more
likely to be younger and with a better ASA score of 1-2, which
translated into a shorter length of hospitalization and fewer
complications (26,27).
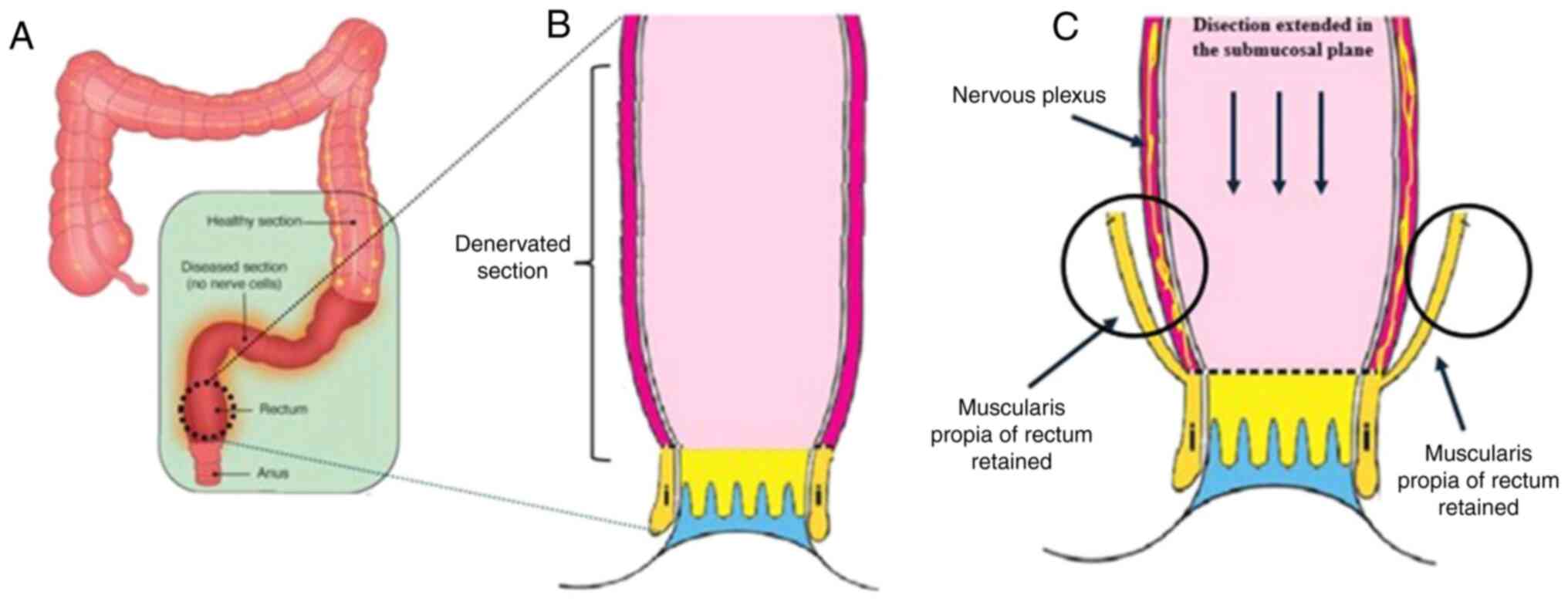
There are three main surgical techniques described:
Swenson (rectosigmoidectomy), Duhamel (retrorectal transanal
pull-through), Lynn and Soave (endorectal pull-through) (1,7). The
Soave technique was first described in 1960 and consists of a
colo-anal anastomosis above the dentate line with rectal
mucosectomy. Its technical advantage over the other techniques
consists of the greater preservation of the internal sphincter,
vessels and pelvic nerves (4,7).
Currently, both Soave's original procedure and the modified one by
Jarry and Faucheron (28) can be
performed minimally invasively via laparoscopy, with excellent
long-term results.
Regardless of the surgical treatment employed,
patients with Hirschsprung's disease who undergo colonic resection
may develop chronic colitis as a chronic adverse effect, rendering
the choice of treatment complex (29). Factors, such as continence and the
maintenance of intestinal physiology are key parameters for
evaluating therapeutic efficacy. The Soave, Duhamel and transanal
endorectal pull-through procedures do not exhibit differences
concerning the post-operative nutritional status of patients with
Hirschsprung's disease (30). On the
other hand, the Soave procedure is preferred for preserving the
integrity of pelvic structures to a greater extent, although it has
also been shown to be associated with an increased incidence of
enterocolitis (31). Furthermore,
the Soave procedure is superior to the Duhamel procedure in
preventing both fecal incontinence and symptoms related to the
post-operative period (32). As
regards intestinal physiology, the Soave procedure does not exhibit
differences compared to other treatments (33). Therefore, the Soave technique appears
to be an ideal treatment within the context of limited resources
for managing adult Hirschsprung's disease, as is the case in the
present study (Fig. 5) (14,34).
According to the European Reference Network for rare
Inherited and Congenital Anomalies (ERNICA) guidelines (29), a recommended pre-operative
preparation for elective surgery includes a combination of saline
rectal irrigations one to three times a day (effective in 75% of
cases) and a single dose of antibiotics to reduce the risk of wound
infections (27). Even though
surgical treatment remains the first and most effective treatment
option, and techniques have greatly improved over time, there are
still a number of post-operative complications that could greatly
decrease quality of life of patients. Possible therapies focusing
on genetic engineering, stem cell research and tissue engineering
could be readily available in the future (3).
Finally, concerning long-term outcomes, the patient
described in the present study demonstrated favorable fecal
continence, with a bowel pattern of approximately one evacuation
daily or every other day, as reported by the patient. However, the
authors consider that a thorough evaluation of the effects of
surgery on intestinal physiology over an extended period of time is
necessary to accurately assess the long-term efficacy of the
intervention.
In conclusion, Hirschsprung's disease is a rare
cause of chronic constipation in adults. In the majority of cases,
it causes subtle and sporadic episodes of constipation, bloating
and abdominal pain; however, an acute presentation of intestinal
obstruction that requires urgent surgical management can be
observed in a minority of patients. As differential diagnoses are
very varied and may be multifactorial, a high index of suspicion is
required. Special emphasis should be placed on past episodes of
constipation, including those in childhood. Hirschsprung's disease
may be the underlying cause of an acute episode of intestinal
occlusive syndrome; hence, taking multiple intraoperative biopsies
of the colorectum for further analyses in those who undergo urgent
laparotomy without an apparent cause identified appears to be a
feasible option. This should be specially considered in patients
with prior episodes of constipation, since an early age without a
definite diagnosis established. The patient required urgent
laparotomy and colostomy due to overlying intestinal occlusive
syndrome with risk of bowel perforation. Multiple seromuscular
biopsy samples were obtained, as there was no evident cause of
intestinal obstruction identified, aiding in the diagnosis of
Hirschsprung's disease. Definitive resolution with excellent
long-term results was later achieved using Soave's procedure.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GGC was a main contributor to the conception of the
study, as well as to the literature search for related studies.
RAMC, ILZL, AART and ERM were involved in the literature review, in
the writing of the manuscript, and in the analysis and
interpretation of the patient's data. GGC and RAMC confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent for
participation
The present study was performed in accordance with
the ethical standards of the Declaration of Helsinki, 1964.
Informed consent was obtained from the patient for inclusion in the
study. Ethics approval was waived by the local committee as no
personal data were used.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chhabra S and Kenny SE: Hirschsprung's
disease. Surgery (Oxford):. 34:628–632. 2016.
|
|
2
|
Lorente-Ros M, Andrés AM, Sánchez-Galán A,
Amiñoso C, García S, Lapunzina P and Solera García J: New mutations
associated with Hirschsprung disease. An Pediatr (Engl Ed).
93:222–227. 2020.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
3
|
Klein M and Varga I: Hirschsprung's
disease-recent understanding of embryonic aspects, etiopathogenesis
and future treatment avenues. Medicina (Kaunas).
56(611)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Vrints I, Costache M, Dobos S, Sondji SH,
Fiasse M and Landen S: Hirschsprung's disease in patients of
advanced age. Int J Gerontol. 6:54–57. 2012.
|
|
5
|
Reategui CO, Spears CA and Allred GA:
Adults Hirschsprung's disease, a call for awareness. A Case Report
and review of the literature. Int J Surg Case Rep. 79:496–502.
2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Qiu JF, Shi YJ, Hu L, Fang L, Wang HF and
Zhang MC: Adult Hirschsprung's disease: Report of four cases. Int J
Clin Exp Pathol. 6:1624–1630. 2013.PubMed/NCBI
|
|
7
|
Soussan H, Jabi R, Ouryemchi M, Haddadi Z
and Bouziane M: Hirschsprung's disease in adults revealed by an
occlusive syndrome. Cureus. 13(e18484)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Devlin HB: Colostomy. Indications,
management and complications. Ann R Coll Surg Engl. 52:392–408.
1973.PubMed/NCBI
|
|
9
|
Lefèvre JH and Parc Y: Soave procedure. J
Visc Surg. 148:e262–e266. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Nessar G and Wu JS: Evolution of continent
ileostomy. World J Gastroenterol. 18:3479–3482. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Rahardjo TM, Nurzaman YA, Natalia J,
Hapdijaya I, Devina L, Andrianto H and Mahardhika JC: Adult
Hirschsprung's disease presenting as chronic constipation: a case
report. J Med Case Rep. 17(308)2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kaji T, Yamada W, Baba T and Machigashira
S: Classification. In: Taguchi T, Matsufuji H and Ieiri S (eds).
Hirschsprung's Disease and the Allied Disorders. Springer,
Singapore, pp47-49, 2019.
|
|
13
|
Páez MB, Vargas Hernández MP and Solís LM:
Hirschsprung´s disease: Update on diagnosis and treatment. Rev Méd
Sinerg. 5(e406)2020.
|
|
14
|
Adamou H, Amadou Magagi I, Habou O, Adakal
O, Aboulaye MB, Rodnodji A, James Didier L, Sani R and Abarchi H:
Diagnosis and surgical approach of adult Hirschsprung's disease:
About two observations and review of the literature. Case series.
Ann Med Surg (Lond). 48:59–64. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chen F, Winston JH III, Jain SK and
Frankel WL: Hirschsprung's disease in a young adult: Report of a
case and review of the literature. Ann Diagn Pathol. 10:347–351.
2006.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Torroglosa A, Alves MM, Fernández RM,
Antiñolo G, Hofstra RM and Borrego S: Epigenetics in ENS
development and Hirschsprung disease. Dev Biol. 417:209–216.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tam PKH: Hirschsprung's disease: A bridge
for science and surgery. J Pediatr Surg. 51:18–22. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Smith M, Chhabra S, Shukla R, Kenny S,
Almond S, Edgar D and Wilm B: The transition zone in Hirschsprung's
bowel contains abnormal hybrid ganglia with characteristics of
extrinsic nerves. J Cell Mol Med. 27:287–298. 2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ibiza S, García-Cassani B, Ribeiro H,
Carvalho T, Almeida L, Marques R, Misic AM, Bartow-McKenney C,
Larson DM, Pavan WJ, et al: Glial-cell-derived neuroregulators
control type 3 innate lymphoid cells and gut defence. Nature.
535:440–443. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bhargava A and Khedkar K: Chronic
constipation unmasking as Hirschsprung disease in a preadolescent:
Delayed presentation or delayed diagnosis? Cureus.
16(e60315)2024.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Yüksel I, Ataseven H, Ertuğrul I, Başar O
and Saşmaz N: Adult segmental Hirschsprung disease. South Med J.
102:184–185. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Srinivas MVN, Satyam G, Hota PK, Suhas M
and Jadhav V: Adult Zonal Hirschsprung's Disease: A Diagnostic
Challenge. ACS Case Rev Surg. 1:38–41. 2017.
|
|
23
|
Arriagada MP, Alfaro G and Rostion CG:
Review: Hirschsprung´s disease. Rev Pediatr Elec. 5:1–9. 2008.In
Spanish.
|
|
24
|
de Lorijn F, Kremer LCM, Reitsma JB and
Benninga MA: Diagnostic tests in Hirschsprung disease: A systematic
review. J Pediatr Gastroenterol Nutr. 42:496–505. 2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ambartsumyan L, Smith C and Kapur RP:
Diagnosis of Hirschsprung disease. Pediatr Dev Pathol. 23:8–22.
2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ma S, Yu Y, Pan A, Gong H, Lou Z, Liu L,
Hao L, Meng R, Sui J and Zhang W: The classification and surgical
treatments in adult Hirschsprung's disease: A retrospective study.
Front Med (Lausanne). 9(870342)2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Schlund D, Jochum SB, Favuzza J, Hayden
DM, Pillai SB, Saclarides TJ and Bhama AR: A national analysis of
operative treatment of adult patients with Hirschsprung's disease.
Int J Colorectal Dis. 35:169–172. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Jarry J and Faucheron JL: Laparoscopic
rectosigmoid resection with transanal colonic pull-through and
delayed coloanal anastomosis: A new approach to adult Hirschsprung
disease. Dis Colon Rectum. 54:1313–1319. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kyrklund K, Sloots CEJ, De Blaauw I,
Bjørnland K, Rolle U, Cavalieri D, Francalanci P, Fusaro F, Lemli
A, Schwarzer N, et al: ERNICA guidelines for the management of
rectosigmoid Hirschsprung's disease. Orphanet J Rare Dis.
15(164)2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ji H, Lai D and Tou J: Neuroimmune
regulation in Hirschsprung's disease associated enterocolitis.
Front Immunol. 14(1127375)2023.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gunadi Juwitasari T, Damayanti NNR,
Kaniashari DS, Kencana SMS and Hastuti J: Growth outcomes in
Hirschsprung disease patients following pull-through. Med J
Malaysia. 75 (Suppl 1):S28–S31. 2020.PubMed/NCBI
|
|
32
|
Zhang Z, Li Q, Li B, Alganabi M and Li L:
Long-term Bowel function and pediatric health-related quality of
life after transanal rectal mucosectomy and partial internal anal
sphincterectomy pull-through for Hirschsprung disease. Front
Pediatr. 11(1099606)2023.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Gunadi Monica Carissa T, Stevie Daulay EF,
Yulianda D, Iskandar K and Dwihantoro A: Long-term functional
outcomes of patients with Hirschsprung disease following
pull-through. BMC Pediatr. 22(246)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Munnangi P, Sayed Mushir Ali A, Deva S,
Kushwaha V, Srivastava S, Boini A, Agarwal RS, Dinkar PK and
Chaudhary E: Post-surgical outcomes of different surgical
techniques in Hirschsprung's disease: A literature review. Cureus.
15(e47012)2023.PubMed/NCBI View Article : Google Scholar
|