Introduction
The COVID-19 pandemic had severe repercussions on
global health; currently, this infection is known for its ability
to harm any organ or system in the body (1). As with other viruses (2), the symptoms it causes can become
chronic (3). Indeed, due to the
success of vaccination efforts, it is estimated that 70% of
COVID-19 infections will have a greater long-term impact than
during the acute phase of the infection (4). The persistence of symptoms following a
COVID-19 infection is known as post-COVID-19 syndrome (5). This condition is characterized by the
presence of symptoms for at least 2 months following the initial
infection (6,7). The emergence of this syndrome does not
depend on the duration of the primary infection (8), but rather on factors, such as age and
the number of symptoms during the acute infection (9). The overall prevalence of post-COVID-19
syndrome has been calculated at 41.79%, although significant
variations exist across different populations (10). Due to the ability of the virus to
cross mucosal barriers (11),
post-COVID-19 syndrome can manifest in the cells and structures of
the skin (12). Potential lesions
associated with COVID-19 have been classified into six groups,
listed in order of prevalence: Acral (51%), vesicular (15%),
urticarial (9%), morbilliform (9%), petechial (3%), livedo
reticularis (1%) and other types (15%) (13). The mechanisms related to these
lesions include the excessive production of inflammatory cytokines
and stress hormones with subsequent damage to the production of
proteoglycans in the extracellular matrix (14), as well as dysregulations in the
humoral response of CD8+ T-lymphocytes (15) and residual effects of post-traumatic
stress (16). However, the
dermatological lesions observed in post-COVID-19 syndrome may
differ from those observed during the acute phase of infection.
Given that there is no specific treatment for dermatological
lesions caused by post-COVID-19 syndrome, the treatment of choice
depends on the symptomatology, thus rendering it essential to
describe the type and nature of the lesions presented (17). For this reason, in the present study,
a systematic review of the dermatological lesions and symptoms
presented during post-COVID-19 syndrome was conducted to detail the
clinical spectrum of this condition and guide the therapeutic needs
of those affected.
Data and methods
Using the PICO strategy, a systematic search was
conducted in the repositories of PubMed, Embase, Scopus and Google
Scholar, utilizing the following key words: ‘Long-Covid Syndrome
and skin manifestations’ OR ‘POST-COVID syndrome and cutaneous
manifestations’ OR ‘Post COVID and Skin’. Only original
multicentric articles, such as prospective cohort studies,
retrospective cohort studies, case series and case reports
published between January, 2020 and January, 2024, written in
English or Spanish, involving patients diagnosed with post-COVID-19
syndrome and documenting clinical skin manifestations or cutaneous
appendages, were included. Studies, such as systematic reviews,
meta-analyses, expert consensus, pre-experimental studies and in
vitro studies were excluded, as well as studies with
unavailable content or imprecise information about symptoms and
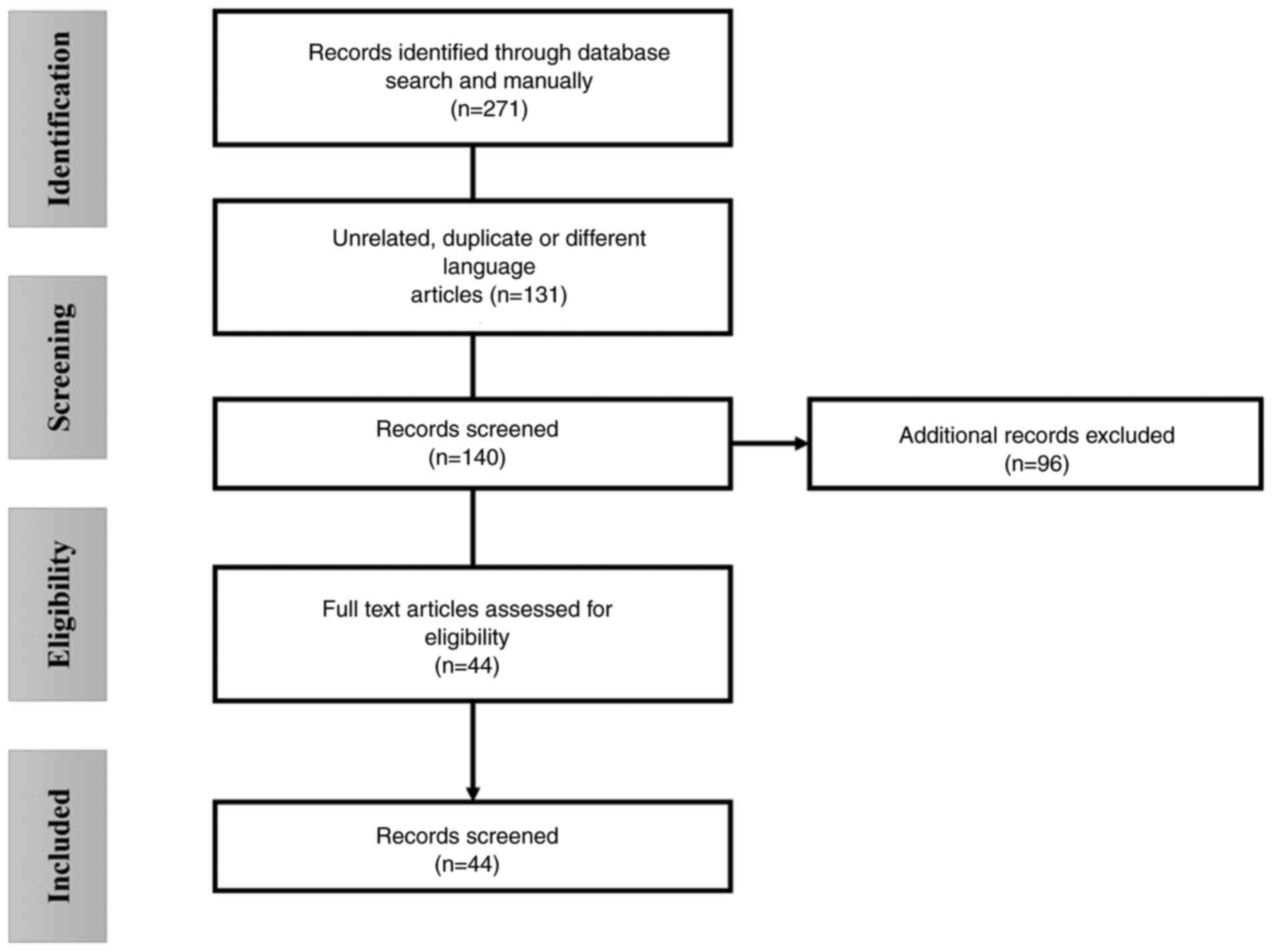
follow-up. Initially, a total of 271 candidate articles were found,
which were reviewed in parallel by two reviewers through the
reading of their abstracts and titles. Following the consensus of
the reviewers, the results of this analysis were organized in a
database, summarizing the characteristics of each record. A total
of 119 studies were discarded due to unrelated information to the
interests of the present systematic review, another 96 for
belonging to other types of studies, one article was excluded for
being in a language other than Spanish or English, and 12 studies
were excluded for duplications, resulting in 44 eligible articles
(Fig. 1).
In the 44 selected articles, data corresponding to
the research question were collected, along with information
regarding the number of participants, presented dermatological
symptoms and follow-up period, among other relevant findings. Of
the included articles, a total of 21 studies were prospective
cohort studies, while four studies were retrospective cohort
studies. Of note, one study was ambispective, and another was a
case-control type study. Additionally, nine studies were
cross-sectional, one study was a case series, and seven studies
were case reports. A list of the included studies is presented in
Table I.
 | Table ISummary of the included studies. |
Table I
Summary of the included studies.
| Authors | Type of study | No. of
patients | Features | Findings | (Refs.) |
|---|
| Menges et
al | P | 442 | 7-Month
follow-up | Non-specific
dermatological symptoms in 11% of patients | (18) |
| Peghin et
al | A | 231 | Healthy
population | 10% Non-specific
symptoms | (19) |
| Peter et
al | R | 11,710 | 12-Month
follow-up | 5.6% of patients
had non-specific rash reactions | (20) |
| Popa et
al | R | 80 | Healthy
population | Non-specific
dermatological symptoms | (21) |
| Munblit et
al | P | 2,649 | More severe effects
in women | 8% of the
population with nonspecific symptoms | (22) |
| Subramanian et
al | P | 48,6149 | Healthy
population | Unspecified
alterations in nails, hair and skin | (23) |
| Fischer et
al | P | 491 | 12 Months
follow-up | Non-specific
symptoms in 23%, worsening depending on the severity of the initial
condition | (24) |
| Leth et
al | P | 49 | Hospitalized
patients | Non-specific skin
manifestations | (25) |
| Ariza et
al | CS | 319 | Psychiatrics
comorbid | Unidentified skin
symptoms | (26) |
| Moreno-Pérez et
al | P | 277 | 14 Weeks
follow-up | 8.36% of patients
with non-specific skin manifestations | (27) |
| Dryden et
al | P | 2,410 | Healthy
population | Skin rash 3.9% per
month and 1.9% after 3 months | (28) |
| Šipetić et
al | CS | 51 | Women with more
severe manifestations | Alterations in
nails, skin and hair: 27.4% of patients in general | (29) |
| Raj et
al | CS | 691 | 9-Month
follow-up | Non-specific skin
symptoms in 1.2% of patients | (30) |
| Funk et
al | P | 8,642 | Pediatric
population | Skin rash 12.50%,
10.30% in non-hospitalized patients | (31) |
| Asakura et
al | CCS | 8,018 | Japanese
population | 1.5% alopecia,
rash, cutaneous chilblains | (32) |
| Alkeraye et
al | CS | 806 | Mostly women | 52.7% with
alopecia, persistence after 3 months | (33) |
|
Fernández-de-Las-Peñas et al | P | 1,969 | Healthy
population | Hair loss (23.9%)
and rash (12%), more affected in women | (34) |
| Jung et
al | R | 1,122 | 4-Month
follow-up | 8.9% skin rash,
9.4% with noticeable hair loss | (35) |
| Kayaaslan et
al | P | 1,092 | Healthy
population | 1% non-specific
symptoms, and hair loss | (36) |
| Hennig et
al | P | 15 | 45 days of
follow-up | Moderate and severe
alopecia in the entire population | (37) |
| Förster et
al | P | 1,459 | Several months of
follow-up | Skin lesions in
2.3%, alopecia in 9.2% of patients | (38) |
| Domènech-Montoliu
et al | P | 484 | More severe in
females and COVID-19 severe infection | Skin lesions in
5.1%, loss of hair density in 22.25% of subjects | (39) |
| Al-Aly et
al | P | 73,453 | Healthy
population | Hair loss and skin
lesions in 7% of subjects | (40) |
| Peter et
al | CS | 12,503 | 12 Months of
follow-up | Skin rash, hair
loss in 7% of subjects | (41) |
| Saberian et
al | CS | 7,226 | Iranian
population | 32% with hair loss,
8% with skin lesions | (42) |
| Rossi et
al | CSR | 14 | 3 Months of
follow-up | Hair loss, worse
results are associated depending on the intensity of COVID | (43) |
| Dumont et
al | P | 1,034 | 12 Weeks
follow-up | Skin lesions and
pruritus in the population | (44) |
| McMahon et
al | P | 330 | 20 to 70 days
follow-up | Presence of
erythematous papules | (45) |
| Weinstock et
al | CS | 136 | Several months of
follow-up | Development of skin
lesions, nodules and alopecia | (46) |
| Bouwensch et
al | P | 160 | Healthy
population | Pruritus in 25%,
blisters and nodules in 12%, Rash, edema in 9%, vesicles and
pigmentary alterations in 6% of patients | (47) |
| Morris et
al | CR | 1 | 1-Month
follow-up | Ecchymosis and
vasculitis | (48) |
| De Medeiros et
al | CR | 1 | Immunocompetent
patient | Case of pemphigus
vulgaris with autoimmune component | (49) |
| Bekaryssova et
al | CS | 193 | Healthy
population | 9.4% of the
population with dermatitis | (50) |
| Qureshi and
Bansal | CR | 1 | Patient with
previous autoimmunity disease | Reactivation of
psoriasis after COVID-19, associated hyperthyroidism | (51) |
| Shimizu et
al | CR | 1 | Healthy
patient | Case of
dermatomyositis and nonspecific rash | (52) |
| Gold et
al | P | 185 | Healthy
population | 7 subjects with
skin rash and cases of Epstein Barr virus reactivation | (53) |
| Gupta et
al | CR | 1 | Healthy
patient | Report of
mucormycosis | (54) |
| Saad and
Mobarak | CR | 1 | Immunocompetent
patient | Cutaneous
mucormycosis secondary to COVID-19 | (55) |
| Ahsan and Rani | CR | 1 | Healthy
patient | Skin rash,
anti-COVID antibodies detected | (56) |
| Richter et
al | P | 59 | 12-Month
follow-up | Anti-epidermis
antibodies were found (41%) | (57) |
|
Fernández-de-Las-Peñas et al | P | 614 | Different
population cohorts | Skin rash according
to variant: Wuhan 12.9%, Alpha 5.7%, Delta 5.0% | (58) |
| Kim et
al | P | 454 | 12-Month
follow-up | ‘COVID toes’ in
1.7% of the population | (59) |
Results
Taken together, the analyzed studies compiled
findings from 626,128 patients screened for dermatological symptoms
secondary to post-COVID-19 syndrome. In the majority of the
records, the findings occurred in a population that was previously
healthy. In five studies, the target population was notable for the
presence of chronical pathologies, psychiatric comorbidities, or a
history of autoimmunity. Furthermore, one study focused on
describing dermatological symptoms due to post-COVID-19 syndrome in
the pediatric population. The average follow-up period and the
onset of symptoms within the analyzed were ~7 months, with a
minimum follow-up of 6 weeks following the diagnosis of COVID-19
and up to a maximum of 12 months post-diagnosis. The most prevalent
dermatological symptoms in the population are detailed in specific
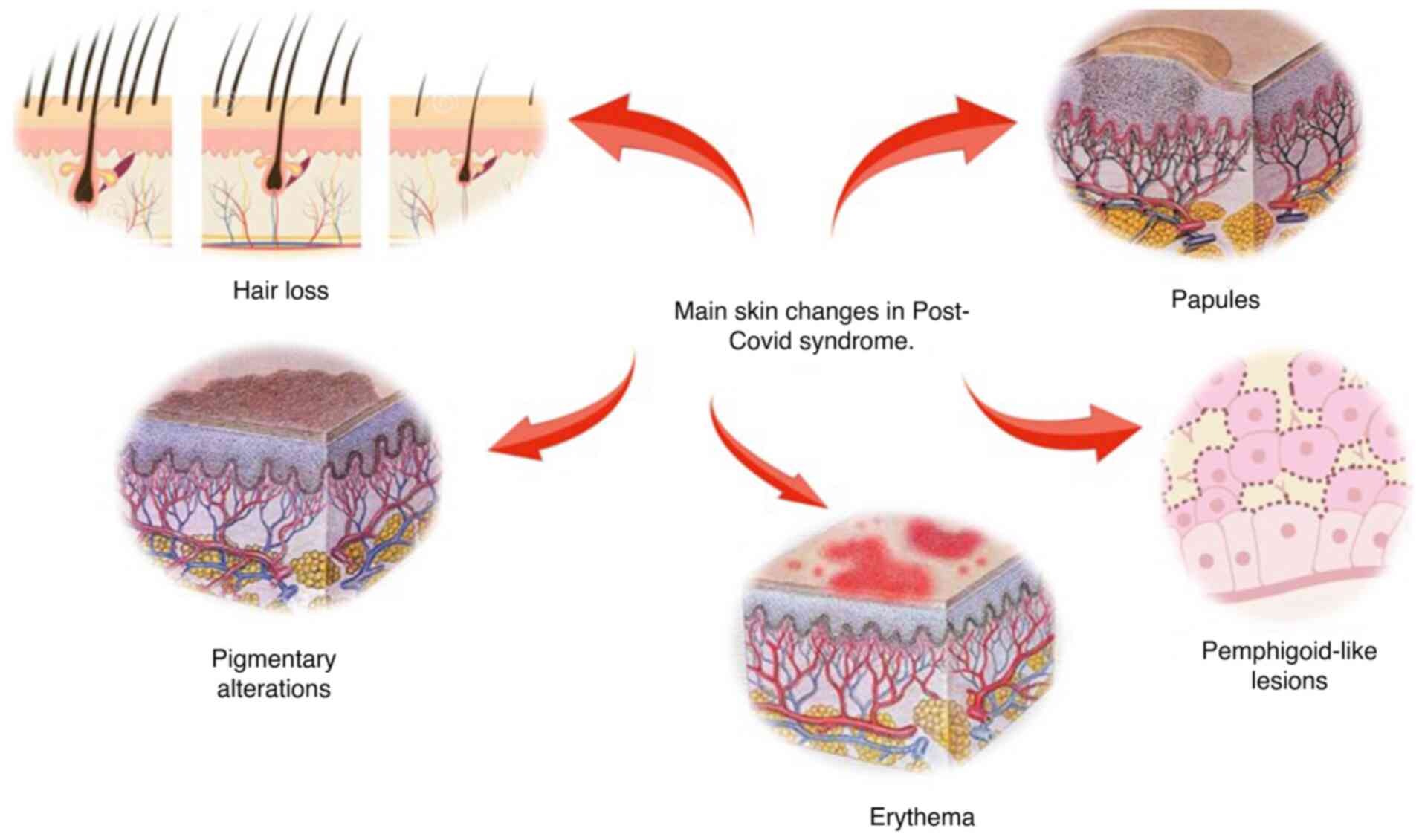
sections below. Additionally, Fig. 2
provides a graphical representation of examples of these
conditions.
Non-specific dermatological
manifestations
Among the studies analyzed, 14 articles described
non-specific cutaneous symptoms as the main finding. These symptoms
were described as ‘skin rash’, ‘dermatological alterations’ and
‘cutaneous symptoms’, without specifying the nature or
characteristics of these alterations (18-31).
The prevalence of this condition varied among the articles, with
the majority of studies indicating a percentage ranging from 5 to
11% of the population. Of note, one study reported a minimum of
1.2% (30), and another reported a
maximum prevalence of 27.4% (29) in
the population. Additionally, three studies highlighted the female
sex and hospitalization as risk factors for presenting these
symptoms with greater severity (22,29,31).
Symptoms associated with hair
health
In addition to the non-specific cutaneous symptoms,
a total of 13 studies described a certain degree of affliction in
hair health. These conditions ranged from a decrease in hair
density and thinning of the follicle to pronounced persistent
alopecia lasting for months, with these issues enduring for an
average period of 3 months following acute COVID-19 infection. The
prevalence of this hair loss demonstrated a high variability,
manifesting in as few as 2% of the population (32) to >50% of study subjects (33), with the majority of the studies
indicating a prevalence between 7 to 35% (34-43).
In two studies, the severity of alopecia was linked to both the
female sex (32) and to the severity
of the initial COVID-19 infection (43).
Skin lesions
On the other hand, six studies described
well-defined skin lesions with distinct characteristics. In two
studies, the presence of papular lesions with irregular borders and
erythematous features was described (44,45). In
two other studies, the presence of subcutaneous nodules was
documented (46,47), one of which also reported the
occurrence of pruritus in 25% of the population, as well as the
formation of blisters and subcutaneous nodules in 12% of subjects,
edema in 9%, pigmentary changes and vesicle formation in 6%
(47). Additionally, one study
mentioned ecchymosis associated with vasculitis (48), and another described pemphigus
vulgaris-like lesions (49).
Dermatitis/associated pathologies
In six studies, cases of dermatitis and pathologies
that appeared concomitantly in the subjects analyzed were
presented. In one study, ~9.4% of the population exhibited
dermatitis with a significant inflammatory component (50). Additionally, two studies mentioned
the worsening of pre-existing pathologies related to autoimmunity,
such as the clinical reactivation of psoriasis (51) and dermatomyositis (52), as well as the reactivation of the
Epstein-Barr virus with the development of characteristic herpetic
lesions (53). Furthermore, two
cases of mucormycosis in immunocompetent patients were reported
(54,55).
Additional dermatological
findings
A total of four studies focused on uncommon
alterations. In two studies, antibodies against the epidermis were
found in up to 41% of the affected subjects (56,57). On
the other hand, one study analyzed the prevalence of cutaneous
symptoms based on the viral variant detected during the primary
infection, with a prevalence of 12.9% for the Wuhan variant, 5.7%
for the Alpha variant and 5% for the Delta type (58). Finally, one study reported the
presence of ‘COVID toes’, a finding where the skin of one or more
toes exhibits edema and bright erythema that gradually turns
violet, potentially showing violaceous brown spots, in 1.7% of its
population (59).
Possible pathophysiological mechanisms
involved in dermatological symptoms in post-COVID-19 infection
Some of the studies reviewed described potential
pathophysiological mechanisms involved in the onset of
dermatological symptoms during the post-COVID-19 state. First, the
cytotoxic potential of the coronavirus was suggested as a possible
contributing factor through molecular interactions with
angiotensin-converting enzyme 2 (ACE2) receptors present on the
host cell surface, which are abundantly expressed in the skin
(60). The interaction between
SARS-CoV-2 and this receptor induces endothelial dysfunction
characterized by localized hyperinflammation, vasculitis,
deposition of complement proteins, and the subsequent development
of skin and appendage lesions (61).
Furthermore, the persistence of this inflammatory
state would increase the production of specific interleukins (IL),
such as IL-6 and IL-4. The former has been linked to the loss of
immune regulation that normally maintains hair follicles in an
immune-privileged state, thereby ensuring their normal growth
(62). Elevated levels of IL-4, on
the other hand, promote keratinocyte apoptosis (63). These alterations, combined with the
overexpression of matrix metalloproteinases 1 and 3, may represent
the underlying mechanism responsible for symptoms, such as hair
loss. This is due to the fact that they can modify the cellular
microenvironment at the base of the hair bulb, thereby promoting
the initiation of the catagen phase in the hair growth cycle
(43).
Additionally, the studies included in the present
systematic review describe mechanisms related to alterations in the
hypothalamic-pituitary axis, generation of anti-epidermal
antibodies and mitochondrial dysfunction in epidermal cells. These
mechanisms have been previously identified as contributors to
long-term dermatological symptoms, not only in COVID-19, but also
in other viral infections, suggesting they may represent a common
pathogenic pathway (64,65).
Clinical implications of the findings
for dermatological practice
According to the analyzed studies, dermatological
symptoms following COVID-19 infection constitute one of the five
major symptom clusters observed in recovered patients. Notably,
these symptoms tend to appear at a later stage (22). The average prevalence of
dermatological symptoms in affected individuals is 51.07%,
primarily concerning hair-related conditions, which have been
proven to be among the most challenging to treat due to their poor
response to treatment (with a resolution rate <50%).
Additionally, they are associated with a more prominent negative
effect on the quality of life of patients and emotional well-being
(19,29,36,37).
Moreover, the onset of these symptoms appears to
follow a variable pattern, with manifestation occurring as early as
3 months post-acute phase, up to a maximum of 18 months in studies
with longer follow-up periods. Notably, there is a possibility that
these dermatological lesions may become chronic, as suggested by a
study theorizing that dermatological manifestations following
COVID-19 may persist indefinitely if left untreated (32) or may reappear periodically with
increased severity (47).
The preceding statements hold significant
implications for dermatological clinical practice. Given that skin
lesions secondary to the post-COVID-19 condition tend to manifest
at a later stage, establishing a link between a prior COVID-19
infection and these conditions can be particularly challenging.
Furthermore, studies indicate a poor therapeutic response to these
lesions, particularly in cases of hair loss, which is often
perceived as a relatively minor issue by numerous healthcare
professionals. However, this complication has emerged as having the
greatest impact on the overall well-being of individuals, rendering
their management a priority in dermatological care.
Discussion
The present systematic review detailed the findings
from studies focusing on post-COVID-19 syndrome and the
dermatological conditions it causes. The literature review
indicated a relatively limited number of records of dermatological
alterations resulting from this syndrome. This scarcity may be due
to the fact that such dermatological manifestations are not as
apparent until the initial impact of the health emergency is
mitigated (66). On the one hand,
while the majority of studies reported only mild and non-specific
skin lesions, other studies revealed two main findings: Firstly, an
increase in cutaneous symptoms associated with hyperinflammation
and immune dysregulations, and secondly, a significant prevalence
of hair loss and alopecia in the affected population.
As regards the first finding, the included studies
reported multiple cases of subjects whose pathology was associated
with hyperinflammation and the development of autoimmunity,
including the reactivation of autoimmune and viral diseases in a
silent state, as well as infections by opportunistic pathogens in
previously healthy individuals. Post-COVID-19 syndrome is
characterized by the development of residual inflammation due to
direct viral toxicity, as well as alterations in the regulatory
function of T-lymphocytes (67).
Studies focusing on this aspect have determined that after
recovering from the acute phase of COVID-19, the virus can cause
T-lymphocytes to exhibit autologous epitopes on their antigen
identification cell receptors, thus creating an autoimmune
environment, particularly in the female body (68).
Moreover, the excessive secretion of IL-6, D-dimer
and lymphopenia produced during the primary COVID-19 infection
increases the likelihood of developing post-COVID-19 syndrome
(69). This is consistent with the
findings that have been reported in previous research (70) and in the present systematic review,
where females and subjects with severe COVID-19 infection presented
more intense dermatological symptoms compared to the remainder of
the population. In line with this finding, previous research has
confirmed that some patients develop autoantibodies following
COVID-19 infection, regardless of whether they have a history of
autoimmunity or not (71). A
proposed mechanism indicates the viral capacity to generate
molecular mimicry with normal body structures (71). Thus, it is possible that the
generation of antibodies against skin layers contributes to the
development of skin lesions as indicated by some studies analyzed
in this review (56,57).
As regards hair loss and alopecia, these conditions
were initially reported during the peak of the pandemic in Spain
(72), and described as expected
findings during the acute phase and convalescence of patients
infected with COVID-19(73). At that
time, these conditions were considered mild and reversible, as with
other viral and bacterial infections, resulting from the alteration
of hair growth cycles following exposure to persistent inflammation
affecting the metabolism of keratinocytes and the dermal papilla
(74).
However, in the case of post-COVID-19 syndrome, it
has been reported that the onset of alopecia occurs more rapidly
and lasts longer compared to other pathogens, suggesting direct
damage to the hair follicle. This is due to the fact that ACE2
receptors, used by COVID-19 for viral entry, are present in both
mesenchymal cells of the hair follicle and its basal layers
(75). Additionally, it has been
theorized that certain components of the hair follicle increase
immunological reactivity against COVID-19, consequently leading to
an increase in antigen-antibody interactions in this area,
resulting in the degradation of the follicle root structures
(76). Furthermore, it is considered
that this localized toxicity generates intense oxidative stress,
leading to the premature onset of the catagen phase of the hair
follicle and hair apoptosis, as well as a reduction in
anticoagulant proteins in the perifollicular vessels, which in turn
facilitates the formation of microthrombi that reduce blood flow to
the hair root, causing it to thin and become fragile (77).
Although hair loss is considered a benign symptom
without real systemic repercussions, its impact on body aesthetics
is crucial for the individual, particularly considering that,
compared with other dermatopathies, the availability of treatments
for this condition is limited (78).
This renders hair loss one of the most critical dermatological
effects of post-COVID-19 syndrome, given the high prevalence rate
of this condition. Thus, the timely approach to this condition in
subjects with risk factors, such as women and severe COVID-19
should be considered a priority in dermatological health
matters.
Although the findings from the present systematic
review are notable due to their clinical implications in
dermatological practice, it is important to highlight the inherent
limitations of the present study. Since the studies analyzed
predominantly rely on reports provided by affected patients, there
is a notable risk of human bias. The integration of technological
tools, such as neural networks for the analysis of dermatological
lesions in post-COVID-19 syndrome, may allow for more accurate data
on the impact of this condition on dermatological health, as has
been observed with other conditions (79,80).
Therefore, the associations generated through these analytical
tools could contribute to future studies identifying both the risk
factors for symptom onset and the pathogenic pathways responsible
for the lesions in post-COVID-19 syndrome.
In conclusion, the present systematic review found
that the dermatological manifestations of post-COVID-19 syndrome
are primarily hair loss and skin lesions associated with persistent
inflammation and the development of autoimmunity, with the severity
of the initial clinical presentation and female sex being risk
factors for severity. Additionally, given that dermatological
lesions in post-COVID-19 syndrome may present in a delayed manner,
their diagnosis should always be considered in patients
experiencing symptoms that cannot be explained by other
dermatological conditions. Furthermore, due to the limited
therapeutic success for some symptoms, such as hair loss, further
studies are required to focus on comparing specific therapeutic
interventions for these conditions.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BACF was a main contributor to the conception of the
study, as well as to the literature search for related studies.
BACF, WMR and DTJ were involved in the literature review, in the
writing of the manuscript, and in the analysis and interpretation
of the patient data obtained from the studies. BACF and DTJ confirm
the authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Garg S, Garg M, Prabhakar N, Malhotra P
and Agarwal R: Unraveling the mystery of Covid-19 cytokine storm:
From skin to organ systems. Dermatol Ther.
33(e13859)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Carod-Artal FJ and García-Moncó JC:
Epidemiology, pathophysiology, and classification of the
neurological symptoms of post-COVID-19 syndrome. Neurol Perspect.
1:S5–S15. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rocha KO, Zanuncio VV, de Freitas BAC and
Lima LM: ‘COVID toes’: A meta-analysis of case and observational
studies on clinical, histopathological, and laboratory findings.
Pediatr Dermatol. 38:1143–1149. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Goetzl EJ and Kapogiannis D: Long-COVID:
Phase 2 of the COVID-19 pandemic. Am J Med. 135:1277–1279.
2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sykes DL, Holdsworth L, Jawad N,
Gunasekera P, Morice AH and Crooks MG: Post-COVID-19 symptom
burden: What is long-COVID and how should we manage It? Lung.
199:113–119. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Castanares-Zapatero D, Chalon P, Kohn L,
Dauvrin M, Detollenaere J, Maertens de Noordhout C, Primus-de Jong
C, Cleemput I and Van den Heede K: Pathophysiology and mechanism of
long COVID: A comprehensive review. Ann Med. 54:1473–1487.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Raveendran AV, Jayadevan R and Sashidharan
S: Long COVID: An overview. Diabetes Metab Syndr. 15:869–875.
2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Fernández-de-Las-Peñas C, Palacios-Ceña D,
Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G and
Navarro-Santana M: Prevalence of post-COVID-19 symptoms in
hospitalized and non-hospitalized COVID-19 survivors: A systematic
review and meta-analysis. Eur J Intern Med. 92:55–70.
2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lippi G, Sanchis-Gomar F and Henry BM:
COVID-19 and its long-term sequelae: What do we know in 2023? Pol
Arch Intern Med. 133(16402)2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sk Abd Razak R, Ismail A, Abdul Aziz AF,
Suddin LS, Azzeri A and Sha'ari NI: Post-COVID syndrome prevalence:
A systematic review and meta-analysis. BMC Public Health.
24(1785)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kabeerdass N, Thangaswamy S,
Mohanasrinivasan V, Rajasekaran C, Sundaram S, Nooruddin T and
Mathanmohun M: Green synthesis-mediated nanoparticles and their
curative character against post COVID-19 skin diseases. Curr
Pharmacol Rep. 8:409–417. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yuen S: Dermatology services: The new
normal post COVID-19. Skin Health Dis. 1(e30)2021.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
de Masson A, Bouaziz JD, Sulimovic L,
Cassius C, Jachiet M, Ionescu MA, Rybojad M, Bagot M and Duong TA:
SNDV (French National Union of Dermatologists-Venereologists).
Chilblains is a common cutaneous finding during the COVID-19
pandemic: A retrospective nationwide study from France. J Am Acad
Dermatol. 83:667–670. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Aldahish A, Vasudevan R, Salem H,
Alqahtani A, AlQasim S, Alqhatani A, Al Shahrani M, Al Mohsen L,
Hajla M, Calina D and Sharifi-Rad J: Telogen effluvium and
COVID-19: A cross-sectional study. Eur Rev Med Pharmacol Sci.
27:7823–7830. 2023.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zou H and Daveluy S: Toxic epidermal
necrolysis and Stevens-Johnson syndrome after COVID-19 infection
and vaccination. Australas J Dermatol. 64:e1–e10. 2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tay MZ, Poh CM, Rénia L, MacAry PA and Ng
LFP: The trinity of COVID-19: Immunity, inflammation and
intervention. Nat Rev Immunol. 20:363–374. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Greenhalgh T, Knight M, A'Court C, Buxton
M and Husain L: Management of post-acute covid-19 in primary care.
BMJ. 370(m3026)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Menges D, Ballouz T, Anagnostopoulos A,
Aschmann HE, Domenghino A, Fehr JS and Puhan MA: Burden of
post-COVID-19 syndrome and implications for healthcare service
planning: A population-based cohort study. PLoS One.
16(e0254523)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Peghin M, Palese A, Venturini M, De
Martino M, Gerussi V, Graziano E, Bontempo G, Marrella F, Tommasini
A, Fabris M, et al: Post-COVID-19 symptoms 6 months after acute
infection among hospitalized and non-hospitalized patients. Clin
Microbiol Infect. 27:1507–1513. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Peter RS, Nieters A, Kräusslich HG,
Brockmann SO, Göpel S, Kindle G, Merle U, Steinacker JM,
Rothenbacher D and Kern WV: EPILOC Phase 1 Study Group. Post-acute
sequelae of covid-19 six to 12 months after infection: population
based study. BMJ. 379(e071050)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Popa MV, Bogdan Goroftei ER, Gutu C,
Duceac M, Marcu C, Popescu R, Popescu R, Druguș D and Duceac LD:
Observational study of post-COVID-19 syndrome in healthcare workers
infected with sars-COV-2 virus: General and oral cavity
complications. Rom J Oral Rehabil. 15:198–207. 2023.
|
|
22
|
Munblit D, Bobkova P, Spiridonova E,
Shikhaleva A, Gamirova A, Blyuss O, Nekliudov N, Bugaeva P,
Andreeva M, DunnGalvin A, et al: Incidence and risk factors for
persistent symptoms in adults previously hospitalized for COVID-19.
Clin Exp Allergy. 51:1107–1120. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Subramanian A, Nirantharakumar K, Hughes
S, Myles P, Wiliams T, Gokhale K, Taverner T, Chandan J, Brown K,
Simms-Williams N, et al: Assessment of 115 symptoms for long COVID
(post-COVID-19 condition) and their risk factors in
non-hospitalised individuals: a retrospective matched cohort study
in UK primary care. Res Sq, 2022.
|
|
24
|
Fischer A, Badier N, Zhang L, Elbéji A,
Wilmes P, Oustric P, Benoy C, Ollert M and Fagherazzi G: Long COVID
classification: Findings from a clustering analysis in the
predi-COVID cohort study. Int J Environ Res Public Health.
19(16018)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Leth S, Gunst JD, Mathiasen V, Hansen K,
Søgaard O, Østergaard L, Jensen-Fangel S, Storgaard M and Agergaard
J: Persistent symptoms in patients recovering from COVID-19 in
Denmark. Open Forum Infect Dis. 8(ofab042)2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ariza M, Cano N, Segura B, Adan A,
Bargalló N, Caldú X, Campabadal A, Jurado MA, Mataró M, Pueyo R, et
al: COVID-19 severity is related to poor executive function in
people with post-COVID conditions. J Neurol. 270:2392–2408.
2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Moreno-Pérez O, Merino E, Leon-Ramirez JM,
Andres M, Ramos JM, Arenas-Jiménez J, Asensio S, Sanchez R,
Ruiz-Torregrosa P, Galan I, et al: Post-acute COVID-19 syndrome.
Incidence and risk factors: A Mediterranean cohort study. J Infect.
82:378–383. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Dryden M, Mudara C, Vika C, Blumberg L,
Mayet N, Cohen C, Tempia S, Parker A, Nel J, Perumal R, et al:
Post-COVID-19 condition 3 months after hospitalisation with
SARS-CoV-2 in South Africa: A prospective cohort study. Lancet Glob
Health. 10:e1247–e1256. 2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Šipetić T, Rajković D, Bogavac Stanojević
N, Marinković V, Meštrović A and Rouse MJ: SMART pharmacists
serving the new needs of the post-COVID patients, leaving no-one
behind. Pharmacy (Basel). 11(61)2023.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Raj SVA, Jacob A, Ambu V, Wilson T and
Renuka R: Post COVID-19 clinical manifestations and its risk
factors among patients in a northern district in Kerala, India. J
Family Med Prim Care. 11:5312–5319. 2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Funk AL, Kuppermann N, Florin TA, Tancredi
DJ, Xie J, Kim K, Finkelstein Y, Neuman MI, Salvadori MI,
Yock-Corrales A, et al: Post-COVID-19 conditions among children 90
days after SARS-CoV-2 infection. JAMA Netw Open.
5(e2223253)2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Asakura T, Kimura T, Kurotori I, Kenichi
K, Hori M, Hosogawa M, Saijo M, Nakanishi K, Iso H and Tamakoshi A:
Case-control study of long COVID, Sapporo, Japan. Emerg Infect Dis.
29:956–966. 2023.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Alkeraye S, Alrashidi A, Alotaibi NS,
Almajli N, Alkhalifah B, Bajunaid N, Alharthi R, AlKaff T and
Alharbi K: The association between hair loss and COVID-19: The
impact of hair loss after COVID-19 infection on the quality of life
among residents in Saudi Arabia. Cureus. 14(e30266)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Fernández-de-Las-Peñas C, Martín-Guerrero
JD, Pellicer-Valero ÓJ, Navarro-Pardo E, Gómez-Mayordomo V,
Cuadrado ML, Arias-Navalón JA, Cigarán-Méndez M, Hernández-Barrera
V and Arendt-Nielsen L: Female sex is a risk factor associated with
long-term post-COVID related-symptoms but not with COVID-19
symptoms: The LONG-COVID-EXP-CM multicenter study. J Clin Med.
11:413–423. 2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Jung YH, Ha EH, Choe KW, Lee S, Jo DH and
Lee WJ: Persistent symptoms after acute COVID-19 infection in
omicron era. J Korean Med Sci. 37(e213)2022.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Kayaaslan B, Eser F, Kalem AK, Kaya G,
Kaplan B, Kacar D, Hasanoglu I, Coskun B and Guner R: Post-COVID
syndrome: A single-center questionnaire study on 1007 participants
recovered from COVID-19. J Med Virol. 93:6566–6574. 2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Hennig V, Schuh W, Neubert A, Mielenz D,
Jäck HM and Schneider H: Increased risk of chronic fatigue and hair
loss following COVID-19 in individuals with hypohidrotic ectodermal
dysplasia. Orphanet J Rare Dis. 16(373)2021.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Förster C, Colombo MG, Wetzel AJ, Martus P
and Joos S: Persisting symptoms after COVID-19. Dtsch Arztebl Int.
119:167–174. 2022.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Domènech-Montoliu S, Puig-Barberà J,
Pac-Sa MR, Vidal-Utrillas P, Latorre-Poveda M, Del Rio-González A,
Ferrando-Rubert S, Ferrer-Abad G, Sánchez-Urbano M, Aparisi-Esteve
L, et al: Complications post-COVID-19 and risk factors among
patients after six months of a SARS-CoV-2 infection: A
population-based prospective cohort study. Epidemiologia (Basel).
3:49–67. 2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Al-Aly Z, Xie Y and Bowe B:
High-dimensional characterization of post-acute sequelae of
COVID-19. Nature. 594:259–264. 2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Peter RS, Nieters A, Kräusslich HG,
Brockmann SO, Göpel S, Kindle G, Merle U, Steinacker JM,
Rothenbacher D and Kern WV: EPILOC Phase 1 Study Group. Post-acute
sequelae of covid-19 six to 12 months after infection: Population
based study. BMJ. 379(e071050)2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Saberian P, Pazooki B, Hasani-Sharamin P,
Garjani K, Ahmadi Hatam Z, Dadashi F and Baratloo A:
Persistent/late-onset complications of COVID-19 in general
population: A cross-sectional study in Tehran, Iran. Int J
Community Based Nurs Midwifery. 10:234–245. 2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Rossi A, Magri F, Sernicola A, Michelini
S, Caro G, Muscianese M, Di Fraia M, Chello C, Fortuna MC and
Grieco T: Telogen effluvium after SARS-CoV-2 infection: A series of
cases and possible pathogenetic mechanisms. Skin Appendage Disord.
21:1–5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Dumont R, Richard V, Lorthe E, Loizeau A,
Pennacchio F, Zaballa ME, Baysson H, Nehme M, Perrin A, L'Huillier
AG, et al: A population-based serological study of post-COVID
syndrome prevalence and risk factors in children and adolescents.
Nat Commun. 13(7086)2022.PubMed/NCBI View Article : Google Scholar
|
|
45
|
McMahon DE, Gallman AE, Hruza GJ,
Rosenbach M, Lipoff JB, Desai SR, French LE, Lim H, Cyster JG, Fox
LP, et al: Long COVID in the skin: A registry analysis of COVID-19
dermatological duration. Lancet Infect Dis. 21:313–314.
2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Weinstock LB, Brook JB, Walters AS, Goris
A, Afrin LB and Molderings GJ: Mast cell activation symptoms are
prevalent in long-COVID. Int J Infect Dis. 112:217–226.
2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Bouwensch C, Hahn V and Boulmé F: Analysis
of 160 nonhospitalized COVID-19 patients with mild to moderate
symptoms from an Austrian general medical practice: From typical
disease pattern to unexpected clinical features. Wien Med
Wochenschr. 172:198–210. 2022.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Morris D, Patel K, Rahimi O, Sanyurah O,
Iardino A and Khan N: ANCA vasculitis: A manifestation of
post-Covid-19 syndrome. Respir Med Case Rep.
34(101549)2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
De Medeiros VLS, Monteiro-Neto AU, França
DDT, Castelo Branco R, de Miranda Coelho ÉO and Takano DM:
Pemphigus vulgaris after COVID-19: A case of induced autoimmunity.
SN Compr Clin Med. 3:1768–1772. 2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Bekaryssova D, Joshi M, Gupta L,
Yessirkepov M, Gupta P, Zimba O, Gasparyan AY, Ahmed S, Kitas GD
and Agarwal V: Knowledge and perceptions of reactive arthritis
diagnosis and management among healthcare workers during the
COVID-19 pandemic: Online survey. J Korean Med Sci.
37(e355)2022.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Qureshi NK and Bansal SK: Autoimmune
thyroid disease and psoriasis vulgaris after COVID-19 in a male
teenager. Case Rep Pediat. 2021(7584729)2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Shimizu H, Matsumoto H, Sasajima T, Suzuki
T, Okubo Y, Fujita Y, Temmoku J, Yoshida S, Asano T, Ohira H, et
al: New-onset dermatomyositis following COVID-19: A case report.
Front Immunol. 13(1002329)2022.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Gold JE, Okyay RA, Licht WE and Hurley DJ:
Investigation of long COVID prevalence and its relationship to
epstein-barr virus reactivation. Pathogens. 10(763)2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Gupta A and Singh V: Mucormycosis: ‘The
black fungus’ trampling post-COVID-19 patients. Natl J Maxillofac
Surg. 12:131–132. 2021.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Saad RH and Mobarak FA: The diversity and
outcome of post-covid mucormycosis: A case report. Int J Surg Case
Rep. 88(106522)2021.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Ahsan T and Rani B: A case of multisystem
inflammatory syndrome post-COVID-19 infection in an adult. Cureus.
12(e11961)2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Richter AG, Shields AM, Karim A, Birch D,
Faustini SE, Steadman L, Ward K, Plant T, Reynolds G, Veenith T, et
al: Establishing the prevalence of common tissue-specific
autoantibodies following severe acute respiratory syndrome
coronavirus 2 infection. Clin Exp Immunol. 205:99–105.
2021.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Fernández-de-Las-Peñas C,
Cancela-Cilleruelo I, Rodríguez-Jiménez J, Gómez-Mayordomo V,
Pellicer-Valero OJ, Martín-Guerrero JD, Hernández-Barrera V,
Arendt-Nielsen L and Torres-Macho J: Associated-onset symptoms and
post-COVID-19 symptoms in hospitalized COVID-19 survivors infected
with wuhan, alpha or delta SARS-CoV-2 variant. Pathogens.
11(725)2022.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Kim Y, Bitna-Ha Kim SW, Chang HH, Kwon KT,
Bae S and Hwang S: Post-acute COVID-19 syndrome in patients after
12 months from COVID-19 infection in Korea. BMC Infect Dis.
22(93)2022.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Cazzato G, Cascardi E, Colagrande A, Foti
C, Stellacci A, Marrone M, Ingravallo G, Arezzo F, Loizzi V,
Solimando AG, et al: SARS-CoV-2 and skin: New insights and
perspectives. Biomolecules. 12(1212)2022.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Gawaz A and Guenova E: Microvascular skin
manifestations caused by COVID-19. Hamostaseologie. 41:387–396.
2021.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Pondeljak N and Lugović-Mihić L:
Stress-induced interaction of skin immune cells, hormones, and
neurotransmitters. Clin Ther. 42:757–770. 2020.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Mandt N, Geilen CC, Wrobel A, Gelber A,
Kamp H, Orfanos CE and Blume-Peytavi U: Interleukin-4 induces
apoptosis in cultured human follicular keratinocytes, but not in
dermal papilla cells. Eur J Dermatol. 12:432–438. 2002.PubMed/NCBI
|
|
64
|
Genovese G, Moltrasio C, Berti E and
Marzano AV: Skin manifestations associated with COVID-19: Current
knowledge and future perspectives. Dermatology. 237:1–12.
2021.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Mui UN, Haley CT, Vangipuram R and Tyring
SK: Human oncoviruses: Mucocutaneous manifestations, pathogenesis,
therapeutics, and prevention: Hepatitis viruses, human T-cell
leukemia viruses, herpesviruses, and Epstein-Barr virus. J Am Acad
Dermatol. 81:23–41. 2019.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Deshmukh V, Motwani R, Kumar A, Kumari C
and Raza K: Histopathological observations in COVID-19: A
systematic review. J Clin Pathol. 74:76–83. 2021.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Najafi MB and Javanmard SH: Post-COVID-19
syndrome mechanisms, prevention and management. Int J Prev Med.
14(59)2023.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Yong SJ: Long COVID or post-COVID-19
syndrome: Putative pathophysiology, risk factors, and treatments.
Infect Dis (Lond). 53:737–754. 2021.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Batiha GE, Al-Kuraishy HM, Al-Gareeb AI
and Welson NN: Pathophysiology of post-COVID syndromes: A new
perspective. Virol J. 19(158)2022.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Jimeno-Almazán A, Pallarés JG,
Buendía-Romero Á, Martínez-Cava A, Franco-López F, Sánchez-Alcaraz
Martínez BJ, Bernal-Morel E and Courel-Ibáñez J: Post-COVID-19
syndrome and the potential benefits of exercise. Int J Environ Res
Public Health. 18(5329)2021.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Stoian M, Procopiescu B, Șeitan S and
Scarlat G: Post-COVID-19 syndrome: Insights into a novel
post-infectious systemic disorder. J Med Life. 16:195–202.
2023.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Goren A, Vaño-Galván S, Wambier CG, McCoy
J, Gomez-Zubiaur A, Moreno-Arrones OM, Shapiro J, Sinclair RD, Gold
MH, Kovacevic M, et al: A preliminary observation: Male pattern
hair loss among hospitalized COVID-19 patients in Spain-A potential
clue to the role of androgens in COVID-19 severity. J Cosmet
Dermatol. 19:1545–1547. 2020.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Nguyen B and Tosti A: Alopecia in patients
with COVID-19: A systematic review and meta-analysis. JAAD Int.
7:67–77. 2022.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Czech T, Sugihara S and Nishimura Y:
Characteristics of hair loss after COVID-19: A systematic scoping
review. J Cosmet Dermatol. 21:3655–3662. 2022.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Sattur SS and Sattur IS: COVID-19
infection: Impact on hair. Indian J Plast Surg. 54:521–526.
2021.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Wei KC, Huang MS and Tsung-Hsien C: Dengue
VIPHHFDPC. Front Cell Infect Microbiol. 8(268)2018.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Gentile P: Hair loss and telogen effluvium
related to COVID-19: The potential implication of adipose-derived
mesenchymal stem cells and platelet-rich plasma as regenerative
strategies. Int J Mol Sci. 23(9116)2022.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Kinoshita-Ise M, Fukuyama M and Ohyama M:
Recent advances in understanding of the etiopathogenesis,
diagnosis, and management of hair loss diseases. J Clin Med.
12(3259)2023.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Hu R, Mo Q, Xie Y, Xu Y, Chen J, Yang Y,
Zhou H, Tang ZR and Wu WQ: AVMSN: An audio-visual two stream crowd
counting framework under low-quality conditions. IEEE Access.
9(1)2021.
|
|
80
|
Hu R, Tang ZR, Wu EQ, Yang R and Li J:
RDC-SAL: Refine distance compensating with quantum scale-aware
learning for crowd counting and localization. Appl Intell.
52:14336–14348. 2022.
|