Introduction
Uremia, the build-up of nitrogenous waste following
renal failure, commonly affects lung function (1). This condition leads to increased lung
vascular permeability, inflammation and dysregulated salt and water
channels, potentially through cytokine-mediated tissue crosstalk
(2,3). Several factors affect the extent of
changes in pulmonary function in uremic individuals, including salt
retention, an accumulation of toxic substances, anemia,
malnutrition and a microinflammatory state (4–7).
Notably, the management of these factors through blood purification
(hemodialysis, dialysis), the correction of anemia, nutritional
improvement and inflammation control improves lung function;
dialysis is the preferred treatment for improving lung function in
uremic patients (8).
Dialysis uses a porous membrane to transfer solutes
and water to the blood, creating a gradient that aids the removal
of urea and other waste products. The flow of particles across this
membrane is partially determined by the size of the pores, since
smaller pores result in lower flux and larger pores result in
higher flux. High-flux dialysis is a more recent treatment that is
increasingly being used in patient care due to the potential
benefits on cardiac outcomes (9).
However, to the best of our knowledge, no previous studies have
investigated whether high-flux dialysis results in improved lung
function in uremic patients.
In the present study, we assessed pulmonary function
in 21 uremic individuals prior to and after high-flux dialysis
treatment and compared their results with those of individuals
treated with low-flux (routine) dialysis. Our results may have
implications for the treatment of remote organ dysfunction in renal
failure.
Subjects and methods
Study subjects
Forty-two uremic patients who were admitted to the
Division of Nephrology, Department of Internal Medicine, The Third
Affiliated Hospital of Anhui Medical University (Hefei, China)
between January 2008 and August 2012 were enrolled in this study.
None of the patients had been previously treated with dialysis or
diagnosed with chronic bronchitis, bronchial asthma or other
chronic respiratory diseases. The patients were equally divided
into two treatment groups, the high-flux and routine groups,
according to their order of admission; the first 21 patients were
placed in the high-flux group and the second 21 in the routine
group. Patients in the high-flux group (13 males and 8 females,
aged 51.3±8.6 years) underwent high-flux dialysis, while those in
the routine group (14 males and 7 females, aged 50.8±7.9 years)
underwent routine dialysis. Additionally, 24 healthy individuals
who underwent physical examination in the Third Affiliated Hospital
of Anhui Medical University during the same period of time were
included in this study to determine the differences in lung
function between uremic patients and healthy individuals. The
control group included 16 males and 8 females, aged 51.9±9.1 years.
Individuals in this group were free from chronic cardiopulmonary
and renal disease, had normal cardiac and pulmonary function, as
confirmed by physical examination, and had a normal chest X-ray and
pulmonary function test. Age and gender were not significantly
different among the groups. This study was approved by the Ethics
Committee of the Third Affiliated Hospital of Anhui Medical
University, and the written informed consent was obtained from the
patients or their family members.
Treatment
Patients in the high-flux group were treated with an
FX60 high-flux dialyzer and a high-flux helixone polysulfone
membrane (membrane area, 1.4 m2; ultrafiltration
coefficient, 46.0 ml/h/mmHg/m2), produced by Fresenius
Medical Care (St. Wendel, Germany). Patients in the routine group
were treated with an F7 dialyzer and a polysulfone membrane
(membrane area, 1.6 m2; ultrafiltration coefficient,
16.0 ml/h/mmHg/m2). The 4008S dialysis machine with an
automatic volume control system (Fresenius), the ultrapure water
bicarbonate dialysate (dialysate flow rate, 500 ml/min; blood flow,
220–300 ml/min) and conventional heparin anticoagulation were used
in the two groups. Dialysis was performed 3 times per week for 4 h
each time, for 3 consecutive months. The dehydration amount
depended on the condition of the patient. Conventional treatment
with erythropoietin and active vitamin D and antihypertensive
treatment were administered to patients in the two groups; the
patients were monitored for 3 months. No treatments were
administered to the healthy individuals in the control group.
Pulmonary function assessment
The pulmonary function of subjects in each of the
three groups was assessed using the 6200 pulmonary function
detector from Sensor Medics (Homestead, FL, USA). For the two
treatment groups, lung function was assessed prior to and after 3
months of dialysis. Pulmonary function indicators included forced
vital capacity (FVC), maximal breathing capacity (MBC), forced
expiratory volume in 1 sec (FEV1), peak expiratory flow
(PEF), maximum middle expiratory flow (MMEF), peak expiratory flow
at 25% vital capacity (V25) and the diffusion capacity
of the lungs for carbon monoxide (DLco). Measured values are
expressed as percentages (%) of normal expected values; pulmonary
function was determined by the first author of this study.
Statistical analysis
SPSS 17.0 was used for statistical analysis.
Measurement data are expressed as the mean ± standard deviation
(SD). The χ2 test and one-way ANOVA were used to compare
gender, age and pulmonary function prior to dialysis among the
three groups. Variance analysis using repeated data measurements
was used to compare pulmonary function prior to and after dialysis
in the high-flux and routine groups, separately, and to compare
pulmonary function between the two groups. Tests were two-sided
with α=0.05 and P<0.05 was considered to indicate a
statistically significant difference.
Results
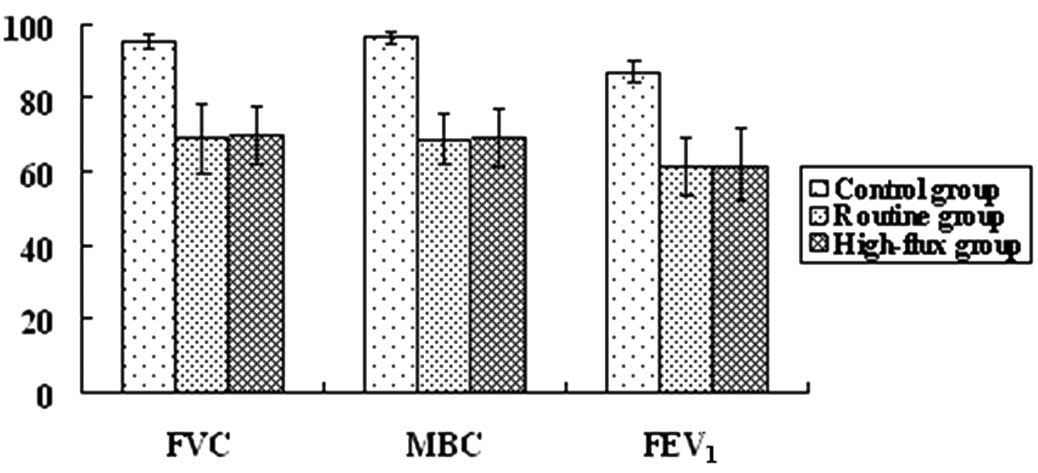
Baseline pulmonary function differs
between uremic patients and healthy individuals
Prior to uremia treatment, pulmonary function was
assessed to determine the baseline lung function of patients in the
two treatment groups compared with that of healthy individuals. For
each parameter (FVC, MBC, FEV1, PEF, MMEF,
V25 and DLco), uremic patients in the high-flux and
routine groups exhibited significantly lower values compared with
the healthy population (P<0.05; Figs. 1 and 2).
High-flux dialysis improves pulmonary
function
The pulmonary function of uremic patients was
reassessed following 3 months of dialysis treatment. After either
high-flux or routine dialysis, several parameters of pulmonary
function were significantly increased compared with their
respective baseline values (FEV1, PEF, MMEF,
V25 in the high-flux and routine groups; all P<0.05;
Table I). Additionally, these
parameters were significantly improved in uremic patients treated
with high-flux dialysis compared with those who underwent routine
dialysis (all P<0.05). No changes were observed in FVC, MBC or
DLco.
 | Table IComparison of pulmonary function
between the high-flux and routine dialysis groups at baseline and
post-treatment. |
Table I
Comparison of pulmonary function
between the high-flux and routine dialysis groups at baseline and
post-treatment.
| Dialysis type | FVC | MBC | FEV1 | PEF | MMEF | V25 | DLco |
|---|
| Routine |
| Baseline (%;
n=21) | 69.1±9.7 | 68.9±6.5 | 61.2±8.0 | 61.4±7.7 | 52.0±6.2 | 54.5±8.1 | 66.9±7.4 |
| Post-treatment (%;
n=21) | 73.0±4.7 | 72.3±7.3 | 67.3±9.7 | 78.9±6.1 | 71.5±6.4 | 74.3±7.2 | 68.9±7.0 |
| F-value | 2.572 | 3.524 | 6.157 | 101.878 | 119.585 | 90.945 | 1.331 |
| P-value | 0.124 | 0.075 | 0.022 | 0.001 | 0.001 | 0.001 | 0.262 |
| High-flux |
| Baseline (%;
n=21) | 69.7±7.7 | 69.0±7.9 | 61.9±9.7 | 60.1±7.8 | 51.5±6.0 | 53.1±9.3 | 67.0±7.7 |
| Post-treatment (%;
n=21) | 73.9±7.4 | 74.1±7.7 | 76.1±9.1 | 87.7±6.5 | 78.3±6.1 | 83.8±7.6 | 70.1±9.4 |
| F-value | 2.879 | 3.714 | 22.282 | 143.016 | 258.185 | 155.198 | 1.669 |
| P-value | 0.105 | 0.068 | 0.001 | 0.001 | 0.001 | 0.001 | 0.211 |
| F-value | 0.220 | 0.335 | 5.398 | 5.457 | 4.565 | 4.543 | 0.106 |
| P-value | 0.642 | 0.566 | 0.025 | 0.025 | 0.039 | 0.039 | 0.746 |
Discussion
The incidence of lung injury in uremic patients has
been reported to be >46.6% (10). Previous studies on the effects of
uremia on pulmonary function have demonstrated decreased pulmonary
diffusion, while results for pulmonary ventilation function are
inconsistent (11,12). In the present study, uremic
patients exhibited significantly lower pulmonary function indices
compared with the healthy population prior to dialysis; the
pulmonary ventilation (FVC, MBC), large- and medium-sized airway
function (FEV1, PEF) and small airway function indices
(MMEF, V25) were all indicative of impaired lung
function. Additionally, the pulmonary diffusion capacity index
(DLco) was significantly impaired. These results indicate that
uremic patients experience pulmonary ventilation and diffusion
dysfunction and airway obstruction, particularly in small airways.
These results may be explained by the accumulation of water and
toxic substances in the body under uremic conditions, which
increases the permeability of alveolar capillaries. This allows the
superabundant liquid to transfer from the pulmonary blood vessels
to the pulmonary interstitium, causing interstitial edema, the
increased osmotic pressure of alveolar capillaries, the hydrostatic
pressure of pulmonary vessels and the ventilation dysfunction of
large and small airways, which manifests as restrictive ventilation
dysfunction. Diffusion function has also been shown to decrease due
to pulmonary interstitial and alveolar edema (11,13).
To assess the effects of dialysis and, more
specifically, to compare the effects of high-flux and routine
dialysis on uremia-induced lung injury, the lung function of uremic
patients was reassessed following high-flux or routine dialysis. Of
the 7 lung function parameters assessed, four (FEV1,
PEF, MMEF and V25) were significantly increased in the
two treatment groups compared with their respective baseline
(pre-treatment) values. However, FVC, MBC and DLco were not
altered. These results indicate that dialysis expels excessive
toxins and water, restores electrolyte and acid-base balance,
reduces the permeability of pulmonary capillaries and relieves
pulmonary edema, thereby improving pulmonary ventilation in uremic
patients (14).
High-flux dialysis has an extremely high diffusion
performance and hydraulic permeability, and is able to eliminate β2
microglobulin from the body of uremic patients, reduce blood
phosphorus, blood fat and parathyroid hormone and relieve
inflammation, oxidative stress and vascular endothelial changes.
This approach is superior to conventional dialysis in eliminating
urea nitrogen, creatinine and other small molecules (15). In the present study, high-flux
dialysis was also superior in the extent of improvement of
pulmonary function in uremic patients. This result provides
additional evidence to support the implementation of high-flux
dialysis in clinics, as it provides a greater benefit in treating
uremia-induced lung injury. Notably, dialysis is a replacement
therapy that is unable to be performed in a persistent state, and
hemodynamic and biological compatibility changes may occur during
the course of this type of treatment. These factors may also affect
the pulmonary function of patients; thus, it is difficult to fully
restore pulmonary function through dialysis.
In conclusion, high-flux dialysis improves the
function of large and small airways and pulmonary ventilation, and
offers a more marked improvement compared with routine dialysis.
Therefore, high-flux dialysis should be considered for clinical use
as it may significantly benefit patients by offering an improved
quality of life.
References
|
1
|
Turcios NL: Pulmonary complications of
renal disorders. Paediatr Respir Rev. 13:44–49. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Scheel PJ, Liu M and Rabb H: Uremic lung:
new insights into a forgotten condition. Kidney Int. 74:849–851.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Doi K, Ishizu T, Fujita T and Noiri E:
Lung injury following acute kidney injury: kidney-lung crosstalk.
Clin Exp Nephrol. 15:464–470. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jean G: How to manage mineral metabolism
disorders in renal failure. Presse Med. 40:1043–1052. 2011.(In
French).
|
|
5
|
Artunc F and Risler T: Serum
erythropoietin concentrations and responses to anaemia in patients
with or without chronic kidney disease. Nephrol Dial Transplant.
22:2900–2908. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nascimento MM, Qureshi AR, Stenvinkel P,
et al: Malnutrition and inflammation are associated with impaired
pulmonary function in patients with chronic kidney disease. Nephrol
Dial Transplant. 19:1823–1828. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Razeghi E, Pazoki M, Ahmadi F, et al:
Relation between pulmonary function and inflammatory biomarkers in
hemodialysis patients. Ren Fail. 34:24–27. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Karacan O, Tutal E, Uyar M, et al:
Pulmonary function in uremic patients on long-term hemodialysis.
Ren Fail. 26:273–278. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eknoyan G, Beck GJ, Cheung AK, et al:
Effect of dialysis dose and membrane flux in maintenance
hemodialysis. N Engl J Med. 347:2010–2019. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wanner C and Ketteler M: Chronic renal
failure. Dtsch Med Wochenschr. 136:1591–1593. 2011.(In German).
|
|
11
|
Kovelis D, Pitta F, Probst VS, et al:
Pulmonary function and respiratory muscle strength in chronic renal
failure patients on hemodialysis. J Bras Pneumol. 34:907–912.
2008.PubMed/NCBI
|
|
12
|
Bush A and Gabriel R: Pulmonary function
in chronic renal failure: effects of dialysis and transplantation.
Thorax. 46:424–428. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dujić Z, Eterović D and Tocilj J:
Pulmonary function in chronic renal failure: effects of dialysis
and transplantation. Thorax. 47:7631992.
|
|
14
|
Prezant DJ: Effect of uremia and its
treatment on pulmonary function. Lung. 168:1–14. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Palmer SC, Rabindranath KS, Craig JC, et
al: High-flux versus low-flux membranes for end-stage kidney
disease. Cochrane Database Syst Rev. 9:CD0050162012.PubMed/NCBI
|