Introduction
Pneumonia is a disease causing serious inflammation
and infection of the lungs and represents one of the leading causes
of mortality, accounting for >50,000 deaths annually (1). Individuals aged ≥65 years are
particularly vulnerable to developing the disease. Furthermore,
pneumonia is more serious in the elderly than in any other age
group (2). However, the diagnosis
of pneumonia in older populations can be difficult since the
elderly are less likely to report the symptoms associated with the
disease, such as fevers, chills and chest pains. Chest radiography
and physical examinations are necessary for a diagnosis to be
obtained, but the diagnosis often remains difficult due to the fact
that the accuracy of chest radiographs in the diagnosis of
pneumonia is low (3). Sputum
samples and antigen tests may be useful in the diagnosis; however,
these methods are time-consuming and lack sensitivity (4).
Biomarkers have the potential to aid health
practitioners in clinical practice. The information provided by
biomarkers should not duplicate that available by standard methods
and the use of the biomarker should enable certain definitive
actions to be taken. Prior to the acceptance of a specific
biomarker for clinical use, the biomarker should have been proven
to be successful in at least one of the following: (i) Showing
diagnostic or prognostic efficacy; (ii) reflecting disease
progression; (iii) aiding patient selection for specific
therapeutic regimens; (iv) exhibiting a wide variety of values; and
(v) being unaffected by the duration of the infection and
continuing to be show efficacy even during prolonged and successive
infections (5).
Aging is often associated with an increase in
inflammation and in the risk of community-acquired pneumonia
(6). Interleukin-1 receptor
antagonist (IL-1RA) is an anti-inflammatory protein that
counteracts the destructive effects of inflammatory proteins
(7). Taking this into account, it
was hypothesized in the present study that pneumonia in elderly
patients may be associated with reduced levels of IL-1RA. Tobacco
smoking has also been associated with impaired pulmonary function
and an increased incidence of infections (8,9),
including in elderly patients (10); however, the mechanism behind this
phenomenon has yet to be elucidated. Therefore, in the present
study, it was also investigated whether smoking affects the level
of IL-1RA and increases the risk of pneumonia.
Materials and methods
Experimental populations
Ethical approval was obtained from the General
Hospital of Shenyang Military Area Command (Shenyang, China) and
written informed consent was obtained from the patients (project
no. DQKY2011-2049B). Ninety young patients with pneumonia (52 males
and 38 females; 30 smokers and 60 non-smokers), aged ~22 years
(range, 18–24 years) and 90 elderly patients with pneumonia (50
males and 40 females; 40 smokers and 50 non-smokers), aged ~70
years (range, 65–73 years) were selected for this study. Patients
with collagen vascular diseases (CVDs) were excluded. For all
patients, the diagnosis was pathologically confirmed by open lung
biopsy or video-assisted thoracoscopic surgery. The mean ± standard
deviation (SD) percentage vital capacity (%VC) of the young
patients was 88±25% (range, 68–120%) and the mean ± SD arterial
oxygen tension (PaO2), measured while breathing room
air, was 11±1.9 kPa (range, 8–15 kPa). The mean ± SD %VC of the
elderly patients was 85±16% (range, 61–112%) and the mean ± SD
PaO2 while breathing room air was 11±1.3 kPa (range,
9–13 kPa). In all patients, crackles were present predominantly in
basal areas and inspiratory squeaks were not found. No positive
serological or other markers of CVD were observed. None of the
patients had taken medicine or immunosuppressant therapy at the
time of the clinical sample collection.
Blood sample collection and
bronchoalveolar lavage fluid (BALF) procedure
Serum samples were obtained from young and elderly
patients. Peripheral venous blood samples were taken and
immediately stored at −80°C. BAL was performed using a flexible
fiberoptic bronchoscope (Olympus 1T-200; Olympus, Tokyo, Japan)
following local anesthesia of the upper airways with 4% lidocaine.
The bronchoscope was inserted into one of the segmental bronchi of
the right middle lobe and 50 ml sterilized saline was then
instilled through the bronchoscope. The fluid was immediately
retrieved by suction using a sterile syringe and the procedure was
repeated three times. BALF was passed through two sheets of gauze
and then centrifuged at 500 × g for 10 min at 4°C. The cells were
washed twice with phosphate-buffered saline (PBS) and the remaining
cells were then suspended in PBS supplemented with 10%
heat-inactivated fetal calf serum and counted using a
hemocytometer. An aliquot was then diluted to a concentration of
2×105 cells/ml and a 0.2-ml cell suspension was spun
down onto a glass slide at 300 × g for 2 min. The remaining fluid
was centrifuged at 500 × g for 5 min and the supernatant was stored
at −80°C. The slides were dried, fixed and then stained using the
May-Giemsa method.
Western blot analysis of the relative
protein levels of IL-1RA
Antibodies against IL-1RA and GAPDH (loading
control) were purchased from Beijing Biotech Co., Ltd., (Beijing,
China). BALF and serum were dissolved in radioimmunoprecipitation
assay buffer [150 mM sodium chloride, 1% NP-40, 0.5% sodium
deoxycholate, 0.1% SDS and 50 mM Tris-HCl (pH 8.0)] and cOmplete
Mini protease inhibitor [Roche R&D Center (China) Ltd.,
Shanghai, China] was included. The debris was removed and the
supernatants were boiled and mixed with an equal volume of 20%
glycerol containing 0.02% bromophenol blue. Proteins were separated
using SDS-PAGE and transferred to a polyvinylidene difluoride
membrane (Millipore Corporation, Billerica, MA, USA). The membranes
were blocked with 5% skimmed milk in 10 mM Tris (pH 7.5), 100 mM
NaCl and 0.1% Tween-20 (TBST) and incubated with primary antibodies
in TBST with 0.5% skimmed milk overnight at 4°C. The membranes were
treated with primary antibodies and horseradish
peroxidase-conjugated goat secondary antibodies (Sangon Biotech
Co., Ltd., Shanghai, China).
Measurement of the immunological activity
of IL-1RA
The levels of IL-1RA were measured using commercial
kits in accordance with the manufacturer’s instructions. IL-1RA
concentrations in the serum and BALF were measured using an ELISA
kit (Sino Biological Inc., Beijing, China). To compare the levels
of IL-1RA with other biomarkers of pneumonia known to be useful for
clinical decisions, the serum levels of periostin, a matrix protein
used as a biomarker to assess histopathological types of pneumonia,
were additionally measured (11).
Periostin levels were measured using an ELISA kit (R&D Systems
China Co., Ltd., Beijing, China).
Statistical analysis
Differences between the two groups were compared
using one-way analysis of variance. Fisher’s protected least
significant difference test was used as a post hoc test. Spearman’s
rank correlation coefficient was used to identify the strength of
correlation between the levels of IL-1RA in the serum and BALF. The
correlation between tobacco smoking and the levels of IL-1RA was
also examined. All subjects had a personal history of smoking 0 to
12 cigarettes/day (the same brand of cigarettes) for the last 10
years. Online software (available at http://www.wessa.net/rwasp_spearman.wasp/) was used to
compute the Spearman’s Rank Correlation and the two-sided P-value,
as well as to create the ordinary scatterplot between the ranks of
X and Y. Data were analyzed using Statview 5.0 software (Abacus
systems, Berkeley, CA, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
Cell counts in BALF
Numerous types of cell are responsible for producing
cytokines in response to local or systemic injury. These cells can
be local resident cells within the lung, including alveolar
macrophages, lung epithelial cells and fibroblasts, or cells such
as neutrophils, lymphocytes, monocytes and platelets (12–14).
The number of inflammatory cells may reflect certain
characteristics of specific types of pneumonia. For young patients,
the total cell counts of macrophages, eosinophils and neutrophils
were significantly higher than those in elderly patients
(P<0.05). However, in the elderly patients, the absolute number
of lymphocytes was higher than those in the young patients
(P<0.05) (Table I). Thus,
pneumonia in elderly patients may be characterized by the high
levels of the predominant inflammatory cells, lymphocytes.
 | Table ICell counts in bronchoalveolar lavage
fluid among different groups. |
Table I
Cell counts in bronchoalveolar lavage
fluid among different groups.
| Patient groups | Number | Total cellsa, ×105/ml | Macrophagesa | Neutrophilsa | Eosinophilsa | Lymphocytesa |
|---|
| Young | 40 | 5.7 (11.8) | 75.8 (36.3) | 6.4 (5.5) | 3.8 (6.1) | 13.7 (8.5) |
| Elderly | 50 | 4.4 (1.3) | 52.8 (21.1) | 3.1 (1.9) | 1.7 (1.8) | 42.0 (21.3) |
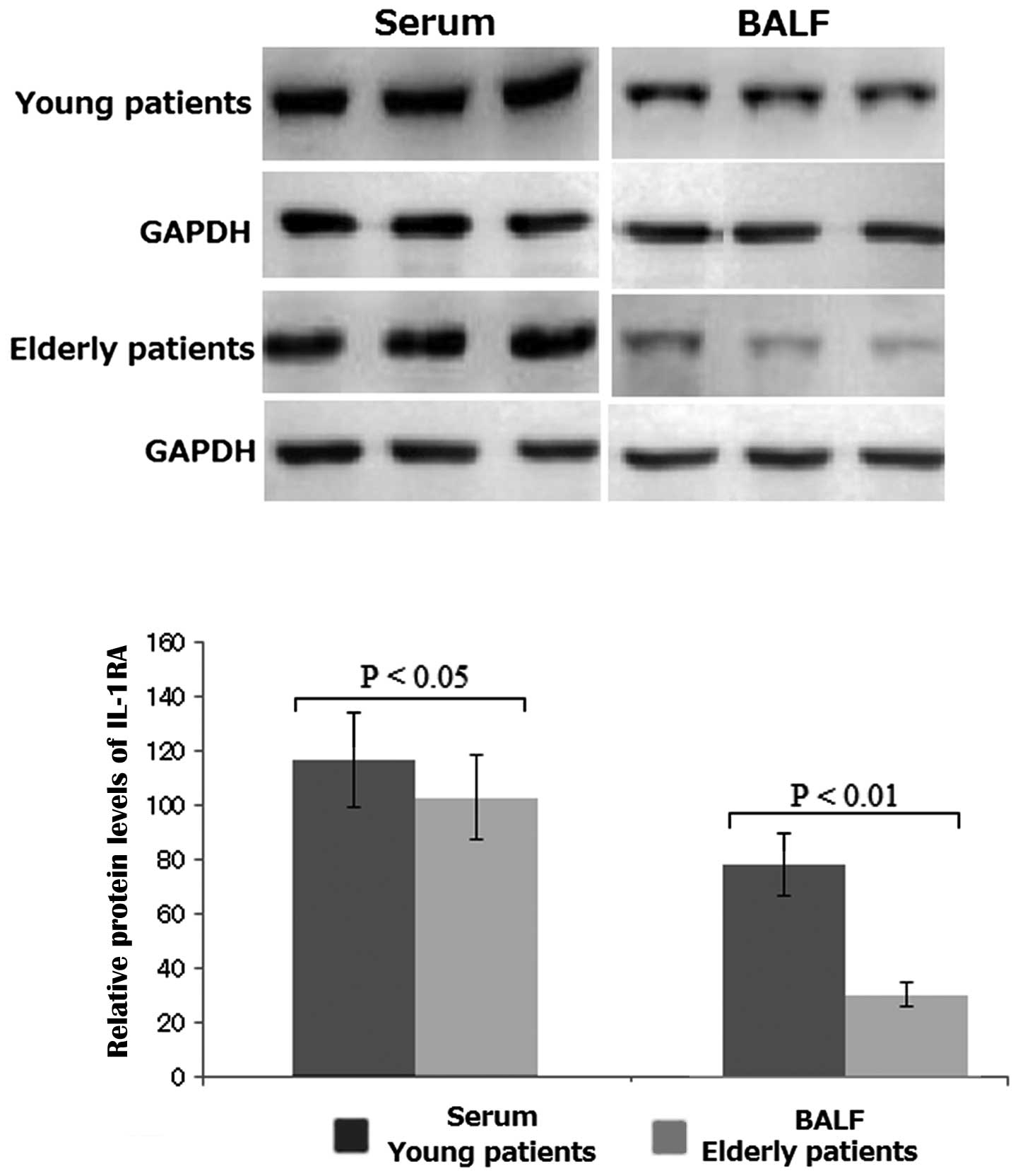
Relative protein levels of IL-1RA in the
serum and BALF
The relative protein levels of IL-1RA in the serum
differed between young and elderly patients: The relative protein
levels of IL-1RA in the serum were lower in elderly patients than
those in young patients (P<0.05; Fig. 1). Similarly, the relative protein
levels of IL-1RA in BALF differed significantly between young and
elderly patients: The relative protein levels of IL-1RA in the BALF
were lower in elderly patients than those in young patients
(P<0.01; Fig. 1). This
difference in protein levels between young and elderly patients was
greater in the BALF than that in serum. Therefore, reduced protein
levels of IL-1RA in BALF may act as an effective biomarker for the
diagnosis of elderly pneumonia.
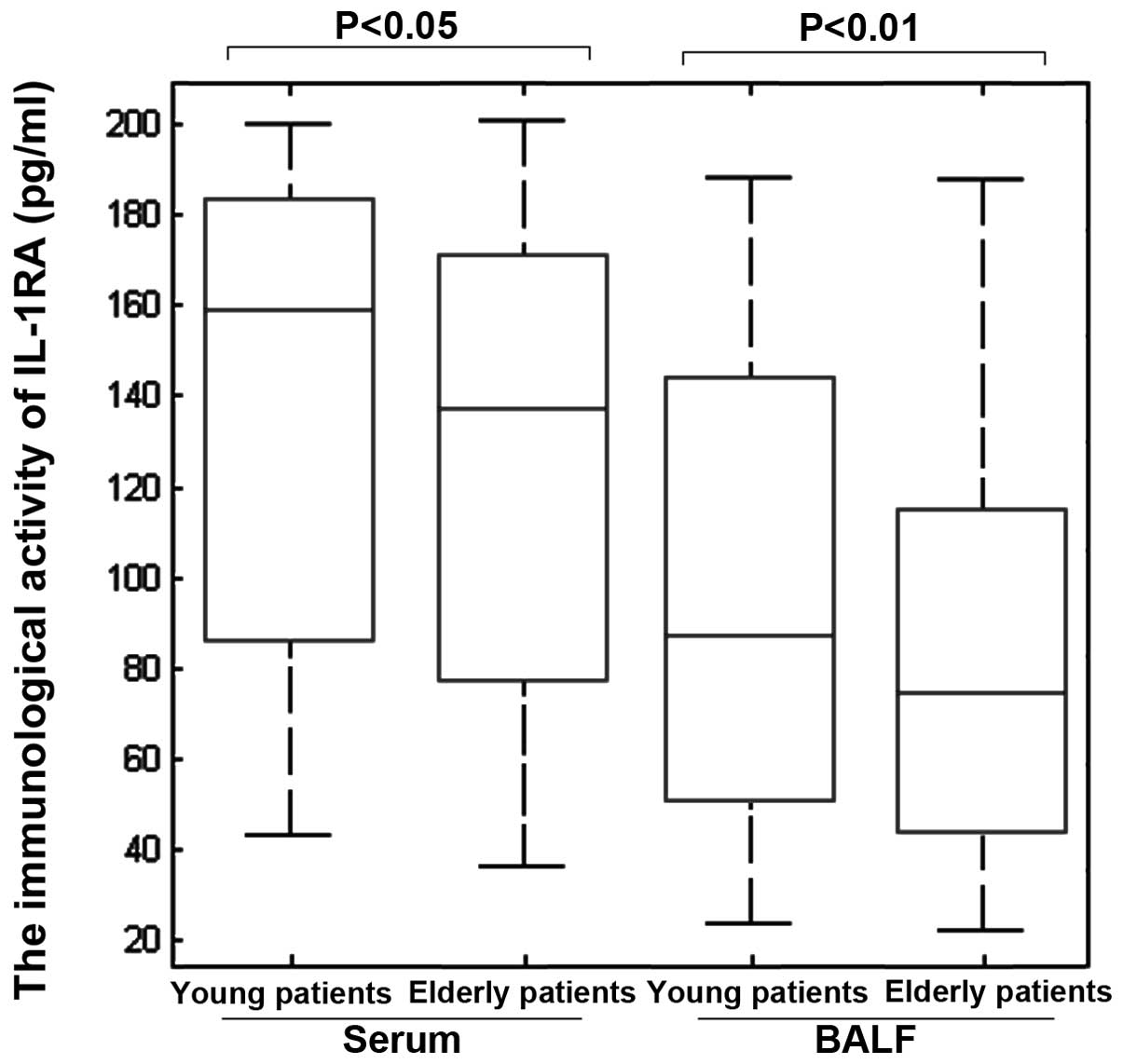
Immunological activities of IL-1RA in the
serum and BALF
The average concentrations of IL-1RA were 160 pg/ml
(range, 84–185 pg/ml) and 138 pg/ml (range, 78–170 pg/ml) in the
serum of the young and elderly patients, respectively. The average
concentrations of IL-1RA were 85 pg/ml (range, 50–143 pg/ml) and 70
pg/ml (range, 40–105 pg/ml) in the BALF of young and elderly
patients, respectively. IL-1RA levels in the serum differed
(P<0.05) between young and elderly patients. The levels of
IL-1RA in the serum were higher in young patients than those in
elderly patients (Fig. 2). IL-1RA
levels in the BALF also differed significantly (P<0.05) between
young and elderly patients: IL-1RA levels in the BALF were higher
in young patients than those in elderly patients (Fig. 2). All the results were in
accordance with the results obtained from the western blot
analysis.
Correlation between the percentage of
lymphocytes and concentration of IL-1RA
The levels of IL-1RA in the serum and the BALF were
inversely correlated with the percentage of lymphocytes in all
individuals (Fig. 3A and B). No
significant correlations were observed between the levels of IL-1RA
and the percentages of neutrophils or eosinophils in the BALF. The
mean serum concentrations of periostin in young patients were
significantly higher than those in elderly patients [young
patients, 49 ng/ml (range, 35.8–77.1 ng/ml) versus elderly
patients, 18.7 ng/ml (range, 11.3–30.1 ng/ml); P<0.005] (data
not shown). In addition, the clinical utility of reduced serum and
BALF IL-1RA levels as markers of pneumonia in the elderly was
investigated. No significant differences were identified in the
mean %VC or PaO2 between young and elderly patients. The
serum and BALF levels of IL-1RA also did not significantly
correlate with any of the pulmonary function test results or
PaO2 (data not shown) in the patients with
pneumonia.
Association between smoking and the
levels of IL-1RA
Smoking damages the natural defenses of the body
against bacteria and viruses that increase the risk of
hospitalization for pneumonia (15,16).
In the present study it was hypothesized that pneumonia in elderly
patients may be due to reduced levels of IL-1RA; therefore, it was
also investigated whether smoking affected the expression levels of
IL-1RA. In young patients, the average concentrations of IL-1RA in
serum and BALF were not correlated with the degree of tobacco
smoking (P>0.05; Fig. 4A and
B). By contrast, the concentration of IL-1RA in the BALF, but
not serum, was closely correlated with the degree of tobacco
smoking in elderly patients (P<0.01; Fig. 4C and D). These results suggested
that smoking may cause a decrease in the expression levels of
IL-1RA in the BALF of elderly patients. The association between the
degree of tobacco smoking and the levels of IL-1RA in the BALF
indirectly provides support for the hypothesis that smoking may
contribute to the pathogenesis of pneumonia in elderly patients by
reducing IL-1RA levels in the BALF but not the serum.
Discussion
This study demonstrated that reduced levels of
IL-1RA may lead to an increased number of lymphocytes in the BALF
of elderly patients compared with the number of lymphocytes in the
BALF of young patients. The levels of IL-1RA were observed to be
inversely correlated with the number of lymphocytes in the BALF.
These findings suggest that the reduced levels of IL-1RA at local
inflammatory sites may lead to the pathogenesis of pneumonia in
elderly patients and an increase in the number of lymphocytes in
the BALF. Surgical lung biopsy remains an important method for the
pathological diagnosis and clinical selection of therapeutic
management for pneumonia. Clinicians often speculate on the
presence of such pathological changes based on non-invasive imaging
studies, for example high-resolution computed tomography (HRCT)
scans (17–19). However, the discrimination between
pneumonias in young and elderly patients, which appear to have
different pathogeneses, may not always be accurately predicted by
HRCT. BAL has been demonstrated to be a useful method to permit
sampling of cells from alveolar areas. In the present study it was
found that reduced levels of IL-1RA were associated with an
increased risk of pneumonia in elderly patients; this may provide
more information for promoting the prognostic significance of young
patients and healthy subjects. The effect of IL-1RA on lymphocyte
infiltration remains unknown. In the presents study it was
indicated that IL-1RA acts as a functional inhibitor of lymphocyte
accumulation in lung lesions and that elderly patients exhibit
reduced levels of IL-1RA. It was also demonstrated that there was a
significant inverse correlation between the levels of IL-1RA in
BALF and the serum levels of periostin in young patients and
healthy individuals, with serum levels of periostin being
significantly higher in elderly patients.
IL-1RA has been found to have a role in the host
immune defense in pneumonia. For example, IL-1RA polymorphism is
associated with the risk of multidrug-resistant Acinetobacter
baumannii-related pneumonia (20). In a study by Patwari et al
(21), the presence or absence of
the A1 allele in the IL-1RA intron 2 polymorphic site was
associated with a decreased or increased risk, respectively, of
severe lung injury in community-acquired pneumonia. Severe lung
injury was indicated by the requirement for positive pressure
ventilation or the development of acute lung injury or acute
respiratory distress syndrome (21). IL-1RA levels have been reported to
be low in elderly patients. For example, in patients with
colorectal cancer undergoing surgery, low preoperative IL-1RA
levels were revealed to be associated with postoperative infection.
Furthermore, lower IL-1RA levels were commonly observed in elderly
patients with low body mass index. These findings suggest that
postoperative infection, which is common among elderly individuals
who are nutritionally deficient, may be a consequence of a
defective immunoinflammatory adaptation system (22). However, levels of IL-1RA have not
been considered for the diagnosis of elderly pneumonia. In the
present study it was found that the levels of IL-1RA in elderly
patients were significantly lower than those in young patients,
resulting in high levels of inflammation in elderly patients and
making them vulnerable to the disease. The low levels of IL-1RA
were also found to be correlated with the disease activity of
pneumonia. These results indicate that low levels of IL-1RA in BALF
may be used as a sensitive parameter for the diagnosis of pneumonia
in the elderly.
Smoking increases the risk of hospitalization for
pneumonia, yet the mechanism behind the phenomenon is unknown. In a
previous study, gingival crevicular fluid (GCF) levels of the
cytokine IL-1RA were analyzed with respect to smoking in patients
with moderate to severe periodontal disease. The clinical
characteristics, in terms of probing depth and frequency of
diseased sites and supragingival plaque, did not differ between
smokers and non-smokers, so the observations did not reveal any
influence of smoking on the levels of IL-1RA in GCF (23). However, the present study revealed
that changes in IL-1RA levels could be detected in BALF, rather
than in serum; BAL has been demonstrated to be useful for analyzing
cells from the alveolar areas.
In the present study it was demonstrated that IL-1RA
levels in the BALF of elderly patients are reduced compared with
those in young patients. In addition, IL-1RA levels were shown to
significantly correlate with the number of lymphocytes in the BALF.
These results suggest that the lymphocytosis in the BALF of elderly
patients is associated with the reduced levels of IL-1RA, which may
be caused by smoking. From these results, it is concluded that
reduced levels of IL-1RA may act as a novel biomarker for elderly
pneumonia. Smoking may increase the risk of pneumonia in the
elderly by further reducing IL-1RA levels in the BALF.
References
|
1
|
Wilson BZ, Anzueto A, Restrepo MI, Pugh MJ
and Mortensen EM: Comparison of two guideline-concordant
antimicrobial combinations in elderly patients hospitalized with
severe community-acquired pneumonia. Crit Care Med. 40:2310–2314.
2012. View Article : Google Scholar
|
|
2
|
Cabre M: Pneumonia in the elderly. Curr
Opin Pulm Med. 15:223–229. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Esayag Y, Nikitin I, Bar-Ziv J, et al:
Diagnostic value of chest radiographs in bedridden patients
suspected of having pneumonia. Am J Med. 123:88.e1–88.e5. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Murdoch DR: Nucleic acid amplification
tests for the diagnosis of pneumonia. Clin Infect Dis.
36:1162–1170. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Christ-Crain M and Opal SM: Clinical
review: the role of biomarkers in the diagnosis and management of
community-acquired pneumonia. Crit Care. 14:2032010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hinojosa E, Boyd AR and Orihuela CJ:
Age-associated inflammation and toll-like receptor dysfunction
prime the lungs for pneumococcal pneumonia. J Infect Dis.
200:546–554. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Berezin V and Bock E: Antagonists of the
interleukin-1 receptor. WO Patent App. PCT/DK2012/000,022. Filed
March 14, 2012; issued September 20, 2012.
|
|
8
|
Mani D, Guinee DG Jr and Aboulafia DM:
Vanishing lung syndrome and HIV infection: an uncommon yet
potentially fatal sequela of cigarette smoking. J Int Assoc
Physicians AIDS Care (Chic). 11:230–233. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Clifford GM, Lise M, Franceschi S, et al:
Swiss HIV Cohort Study: Lung cancer in the Swiss HIV Cohort Study:
role of smoking, immunodeficiency and pulmonary infection. Br J
Cancer. 106:447–452. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kikuchi R, Watabe N, Konno T, Mishina N,
Sekizawa K and Sasaki H: High incidence of silent aspiration in
elderly patients with community-acquired pneumonia. Am J Respir
Crit Care Med. 150:251–253. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Okamoto M, Hoshino T, Kitasato Y, et al:
Periostin, a matrix protein, is a novel biomarker for idiopathic
interstitial pneumonias. Eur Respir J. 37:1119–1127. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dolinay T, Kim YS, Howrylak J, et al:
Inflammasome-regulated cytokines are critical mediators of acute
lung injury. Am J Respir Crit Care Med. 185:1225–1234. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sisson TH, Mendez M, Choi K, et al:
Targeted injury of type II alveolar epithelial cells induces
pulmonary fibrosis. Am J Respir Crit Care Med. 181:254–263. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Grommes J and Soehnlein O: Contribution of
neutrophils to acute lung injury. Mol Med. 17:293–307. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cecere LM, Williams EC, Sun H, et al:
Smoking cessation and the risk of hospitalization for pneumonia.
Respir Med. 106:1055–1062. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Katzenstein AL: Smoking-related
interstitial fibrosis (SRIF), pathogenesis and treatment of usual
interstitial pneumonia (UIP), and transbronchial biopsy in UIP. Mod
Pathol. 25(Suppl 1): S68–S78. 2012. View Article : Google Scholar
|
|
17
|
Jeong YJ, Lee KS, Chung MP, Han J, Johkoh
T and Ichikado K: Chronic hypersensitivity pneumonitis and
pulmonary sarcoidosis: differentiation from usual interstitial
pneumonia using high-resolution computed tomography. Semin
Ultrasound CT MR. 35:47–58. 2014. View Article : Google Scholar
|
|
18
|
Lynch DA and Huckleberry JM: Usual
interstitial pneumonia: typical and atypical high-resolution
computed tomography features. Semin Ultrasound CT MR. 35:12–23.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Eisman Hidalgo M, Nuñez-Delgado Y and
García Espona MÁ: Idiopathic lipoid pneumonia findings in chest
high resolution computed tomography. A case report. Arch
Bronconeumol. 50:83–84. 2014.(In English and Spanish).
|
|
20
|
Hsu MJ, Lu YC, Hsu YC, Liu WS and Wu WT:
Interleukin-1 receptor antagonist gene polymorphism in patients
with multidrug-resistant Acinetobacter baumannii-associated
pneumonia. Ann Thorac Med. 7:74–77. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Patwari PP, O‘Cain P, Goodman DM, et al:
Interleukin-1 receptor antagonist intron 2 variable number of
tandem repeats polymorphism and respiratory failure in children
with community-acquired pneumonia. Pediatr Crit Care Med.
9:553–559. 2008. View Article : Google Scholar
|
|
22
|
Miki C, Inoue Y, Toiyama Y, et al:
Deficiency in systemic interleukin-1 receptor antagonist production
as an operative risk factor in malnourished elderly patients with
colorectal carcinoma. Crit Care Med. 33:177–180. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Boström L, Linder LE and Bergström J:
Smoking and GCF levels of IL-1beta and IL-1ra in periodontal
disease. J Clin Periodontol. 27:250–255. 2000.PubMed/NCBI
|