Introduction
Neuroglobin (NGB) was identified and initially
described by Burmester et al in 2000 (1). This recently identified protein is
expressed in the tissues of the nervous system, including those of
the retina (2). It is a member of
the hemoglobin superfamily and is a significant ischemic-hypoxic
biomarker for brain injury (3–5). An
increase in the expression of NGB under hypoxic conditions exhibits
a neuroprotective function in vitro and in vivo
(6–8). The oxygen-binding properties of NGB
are comparable to those of typical vertebrate myoglobin, suggesting
a similar function for NGB in the brain (9–11).
Previously, NGB upregulation in the murine brain following
forebrain ischemia, has been demonstrated following carotid artery
occlusion (12). However, compared
with extensive brain ischemia, focal cerebral ischemia, such as
basal nucleus infarction, is more frequently observed in clinical
settings (13).
Consequently, the determination of whether NGB is
upregulated during focal ischemia, and whether such upregulation
exerts a neuroprotective effect near the ischemic penumbra, was
important. Furthermore, a primary objective of the present study
was to identify upstream proteins, which exhibit ischemia-induced
changes in expression. In addition, the variation in serum redox
index values in focal brain ischemic cases was of interest, such as
those for superoxide dismutase (SOD) and malondialdehyde (MDA), as
this may indicate oxygen radical-induced lipid peroxidation during
hypoxic-ischemic encephalopathy, thereby providing an index of
neuronal damage and recovery. The present study was designed to
characterize changes in the expression of NGB and other
ischemia-regulated proteins in brain tissue, as well as to profile
serum redox indices in a rat model of focal cerebral ischemia
following reperfusion for different time periods.
Materials and methods
Animals
The present study was approved by the ethics
committee of the General Hospital of the Chinese People’s
Liberation Army (Beijing, China). A total of 63 male Sprague-Dawley
rats (weight, 280–300 g; Vital River Laboratory Animal Technology
Co. Ltd., Beijing, China) were randomly divided into the following
seven groups (each containing nine rats): The sham group, in which
the common carotid artery (CCA) was exposed, without insertion of a
filament; the 0 h reperfusion group, in which middle cerebral
artery occlusion (MCAO) was performed but no reperfusion treatment
was administered; and five ischemic-reperfusion groups, in which
MCAO was performed and reperfusion treatment was administered for
4, 8, 16, 32 or 64 h, after MCAO treatment. All experimental
procedures and animal handling protocols were approved by the
Institutional Animal Care and Use Committee of the General Hospital
of the Chinese People’s Liberation Army (approval no. 2008-X1-71).
The animals were allowed ad libitum access to food and water
and housed in a climate-controlled environment (25°C).
Construction of rat MCAO model
The MCAO model was established according to the
following procedures. Rats were anesthetized with 1% sodium
pentobarbital (40 mg/kg; Sigma-Aldrich, St. Louis, MO, USA). A
midline neck incision was made in order to expose the right CCA and
to enable its separation from the adjacent nerves and tissues. The
internal carotid artery was isolated, following occlusion of the
external carotid artery, and a filament was inserted into the CCA
by scalp acupuncture and slowly advanced until resistance was felt,
while a portion of the filament remained exposed. The filament was
removed following 1.5 h of mechanical artery blockage. Sham surgery
was performed in an identical manner, but without filament
occlusion of the arteries. The animals in the six groups in which
MCAO was performed were sacrificed using 1% sodium pentobarbital
(80 kg/kg) following reperfusion, 0, 4, 8, 16, 32 or 64 h after
MCAO treatment.
Triphenyltetrazolium chloride (TTC)
staining
Rat brain tissues were frozen at −20°C for 20 min
and cut into 10-µm sections using a cryostat (LS-3000;
Shenyang Longshou Electronic Equipment Co., Ltd, Shenyang, China).
The sections were labeled P1, P2, P3, P4 and P5, and were stained
with 2% TTC (Sigma-Aldrich) at 37°C for 20 min in complete
darkness. The necrotic areas were analyzed using Image-Pro Plus 7.0
software (Media Cybernetics, Inc., Rockville, MD, USA).
Hematoxylin and eosin (HE) staining
The rat brain tissues were prepared, fixed and
sliced prior to storage. HE staining was performed according to the
following procedure. Preserved slides were deparaffinized and
rehydrated prior to staining. Frozen or vibratome sections were
mounted on slides and rehydrated prior to staining. A slight
over-staining of the sections with HE (Sigma-Aldrich) was performed
for 3–5 min, depending on the section thickness and quantity of
fixative present. Excessive stain was then removed using tap water.
The differentiation was accomplished with four-five immersions in
acidic alcohol or until sections appeared red. Excess alcohol was
removed by rinsing with tap water. The nuclei were stained blue by
treating the HE-stained sections with bicarbonate for 2 min,
followed by an 8 min rinse with tap water. The HE-stained sections
were placed in 70% ethanol for 3 min and then stained with eosin
for 2 min in order to resolve the cellular details. Eosin-treated
sections were subjected to three consecutive treatments of 5-min
incubations with 95% ethanol followed by transfer to absolute
ethanol for clearing. Images of stained hippocampus and cortex
sections were captured through a microscope (80i; Nikon, Tokyo,
Japan) connected via a charge-coupled device camera (magnification,
x200; Nikon Corporation, Tokyo, Japan).
Immunohistochemistry
Sections were deparaffinized, rehydrated and washed
three times with 0.01 M phosphate-buffered saline (PBS). Endogenous
peroxidase activity was quenched by incubating the sections with 3%
H2O2 (Beijing Zhongshan Biotechnology Co.,
Ltd., Beijing, China) for 30 min. The sections were then subjected
to sequential incubations in 10% normal goat serum (Beijing
Zhongshan Biotechnology Co., Ltd.) in 0.01 M PBS for 30 min at room
temperature. The sections were incubated in polyclonal rabbit
anti-goat NGB antibody (1:100; cat. no. sc-22001; Santa Cruz
Biotechnology, Inc., Santa Cruz, CA, USA) in PBS, containing 0.3%
Triton X-100 at 4°C overnight. Following three washes for 5 min
each with PBS, the sections were incubated in peroxidase-conjugated
goat anti-rabbit IgG (cat. no. 111213-96-8; 1:200; Zymed, San
Francisco, CA, USA) for 1 h at room temperature. Finally, the
sections were developed with diaminobenzidine (Sigma-Aldrich) in
0.1 M Tris-buffered saline, containing 0.001%
H2O2 for 30–50 min. The number of
NGB-positive cells and total positive area in the assigned
sub-regions was measured using the Image-Pro Plus 7.0 software.
Reverse transcription quantitative
polymerase chain reaction (RT-qPCR) for hypoxia inducible factor
(HIF)-1α and NGB
The PCR primer pairs used, which were based on
HIF-1α, NGB, and β-actin sequences from rats, were as follows:
Forward: 5′-GATGCAGCACGATCTCGGCGAA-3′ and reverse:
5′-TGGGAGCTCACGTTGTGGGGAA-3′ for HIF-1α, forward:
5′-AAGGGCGGTTCTCTGGGAGCTT-3′ and reverse:
5′-AGAGGATGTGCAGGGCCAGCTT-3′ for NGB and forward:
5′-GATGCAGCACGATCTCGGCGAA-3′ and reverse:
5′-TGGGAGCTCACGTTGTGGGGAA-3′ for β-actin.
Rat brain tissues from each group were separated
into ischemic and non-ischemic regions. Total RNA was extracted
from tissues using TRIzol™ reagent (Invitrogen Life Technologies,
Carlsbad, CA, USA), and reverse transcribed using the Total RNA
transcription kit (cat. no. R6834-01; Omega Bio-Tek, Inc., Shiga,
Japan). For RT-qPCR, 100 ng total RNA was used as a template
quantity in order to determine HIF-1α and NGB mRNA expression
levels. The results were analyzed using SDS 1.4 software (Applied
Biosystems, Foster City, CA, USA), based on the 2(−ΔΔCt)
method (14).
Western blot analysis of NGB and HIF-1α
expression
The total brain tissue protein for each group was
extracted and quantified. Approximately 35 mg total protein was
separated by 12.5% SDS-PAGE and transferred onto a polyvinylidene
difluoride membrane for overnight hybridization with polyclonal
rabbit anti-rat NGB antibody (1:500; sc-22001; Santa Cruz
Biotechnology, Inc.), polyclonal rabbit anti-mouse β-actin
(1:1,000; sc-81178; Santa Cruz Biotechnology, Inc.) and monoclonal
rabbit anti-rat HIF-1α antibody (1:500; ab51608; Abcam, Cambridge,
MA, USA). The blotted membranes were incubated for 2.5 h with
horseradish peroxidase-labeled goat anti-rabbit secondary antibody
(1:1,000; cat. no. sc-2004; Santa Cruz Biotechnology, Inc.). The
protein bands were read with an electronic scanner and analyzed
using the Image-Pro Plus 7.0 software.
Quantification of serum SOD activity and
MDA concentration
The SOD enzyme activity and MDA concentration were
measured according to the manufacturer’s instructions using SOD and
MDA assay kits (Dojindo Laboratories, Beijing, China).
Statistical analysis
All data are expressed as the mean ± standard
deviation. The statistical analysis for the morphometric
quantification of the NGB-positive cells was performed using a
one-way analysis of variance. Scheffé’s test for group mean
comparisons was used for post-hoc comparisons. Statistical analyses
were performed using SPSS version 21.0 software (IBM Corp., Armonk,
NY, USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
Necrotic zone areas increase with
increasing reperfusion time and different brain slices exhibit
different necrotic zones
Different brain sections exhibited different
necrotic zones, as indicated by TTC staining. The
ischemic-reperfusion group exhibited larger necrotic zones than
that of the 0 h reperfusion and sham groups in each brain section
(P<0.01; Fig. 1A). The
reperfusion treatment groups exhibited significant damage in
different brain sections, as compared with the sham and 0 h
reperfusion groups (P<0.01; Fig.
1B).
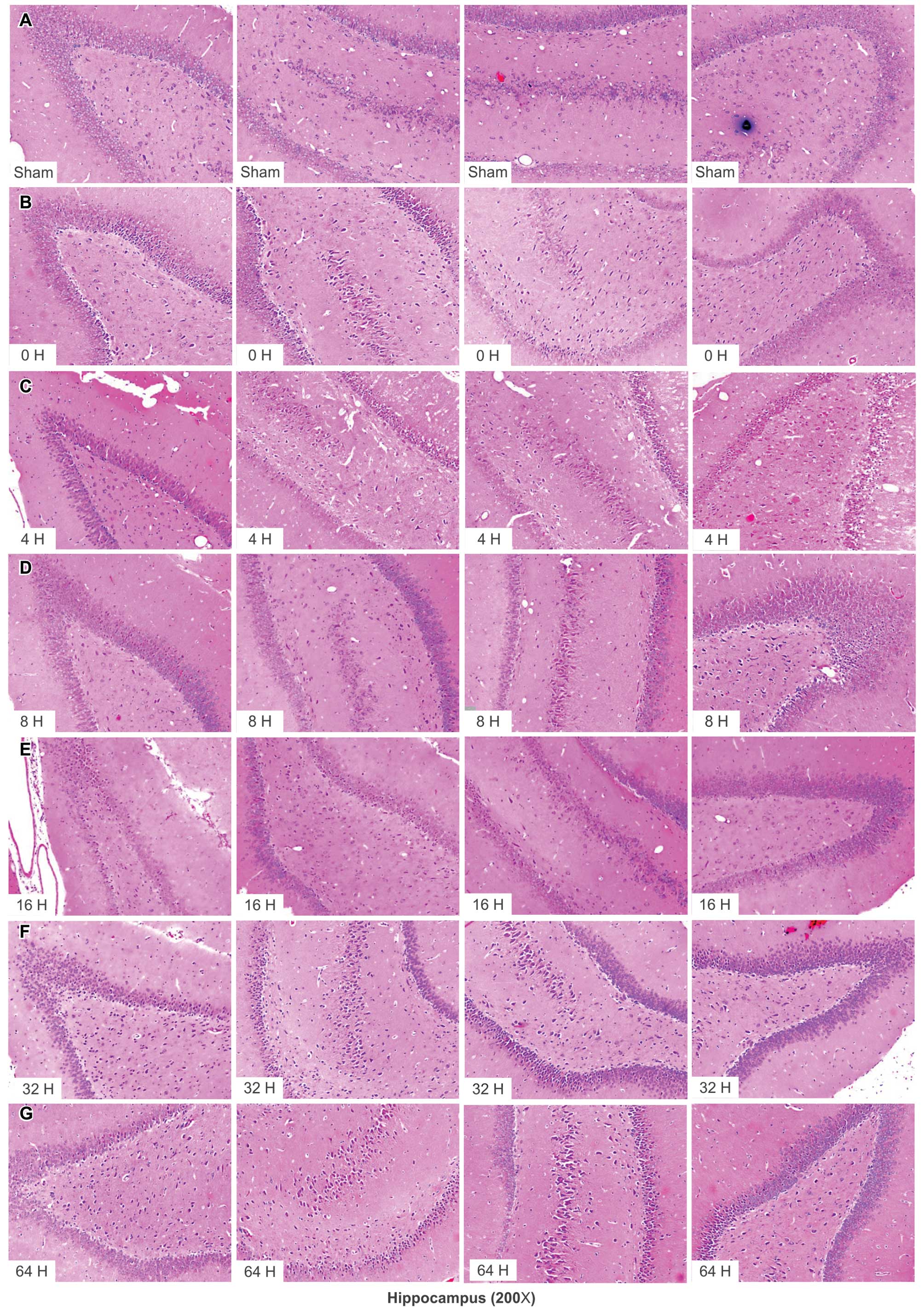
Quantity of hyperchromatic cells in
different hippocampal and cortical regions increases with
increasing reperfusion time
The number of hyperchromatic cells in different
hippocampal regions detected by HE staining, increased with
reperfusion time and peaked in the group that received reperfusion
at 32 h after MCAO (Fig. 2). A
similar trend was observed for cortical regions (Fig. 3).
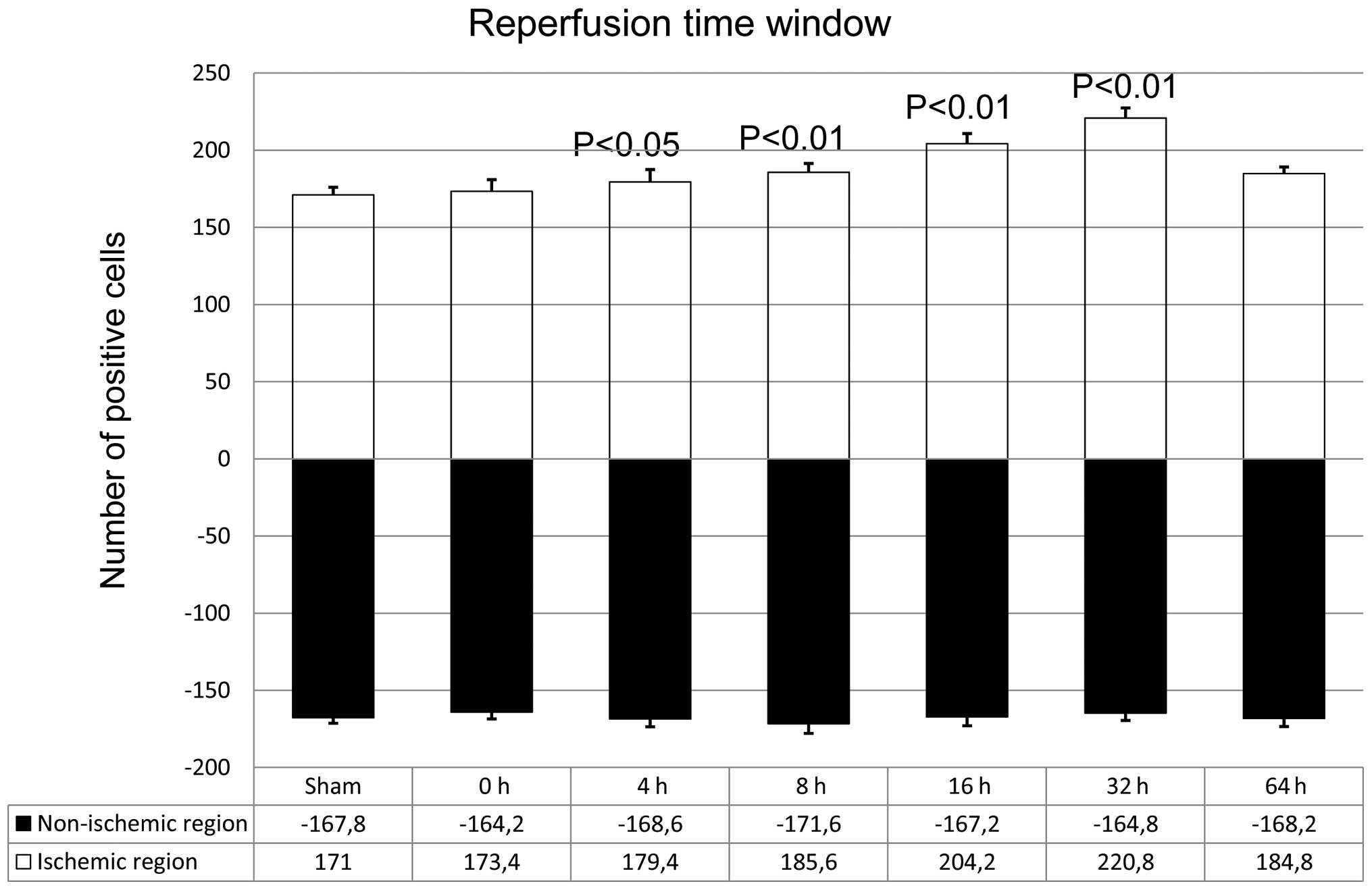
Quantity of NGB-positive cells in
different cortical regions increases with increasing reperfusion
time
Following induction of acute focal cerebral
ischemia, NGB expression levels in the ischemic region increased
with increasing reperfusion time, as indicated by
immunohistochemical analysis. The maximal level of NGB expression
was observed in the group that received reperfusion at 32 h after
MCAO (P<0.01; Fig. 4). However,
NGB expression levels in the non-ischemic regions did not vary with
reperfusion time (P<0.01; Fig.
4).
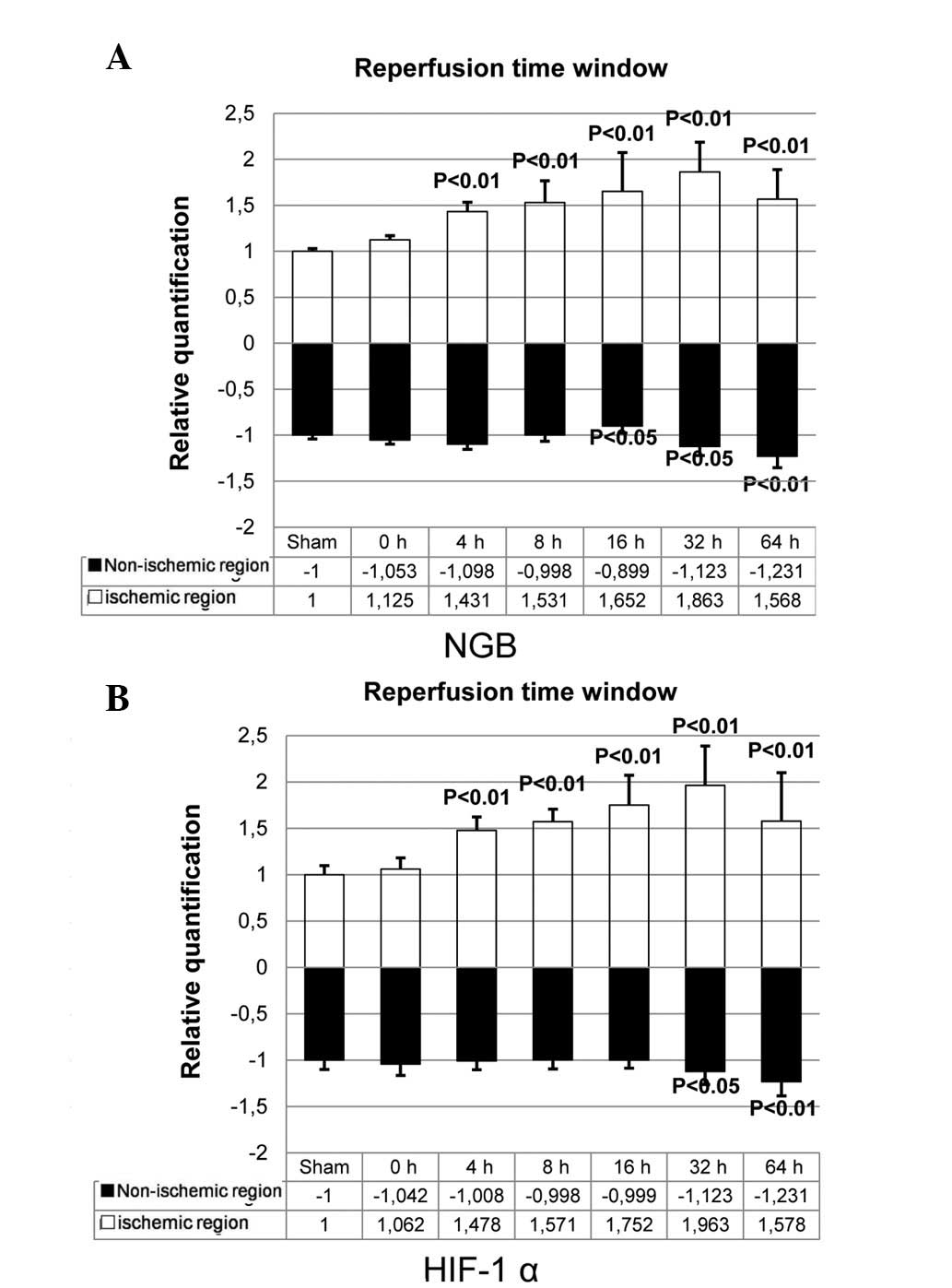
NGB and HIF-1α mRNA and protein
expression levels increase following ischemic reperfusion
NGB expression levels in the ischemic region
increased with increasing reperfusion time; the levels for all five
ischemic-reperfusion groups were significantly higher than that of
the sham group, and levels peaked in the group that received
reperfusion at 32 h after MCAO (P<0.01; Fig. 5A). For the non-ischemic regions,
NGB expression levels in the 16 h and 32 h reperfusion groups were
reduced, compared with those in the sham group (Fig. 5A), and the decrease was significant
in the group that received reperfusion at 64 h after MCAO
(P<0.01; Fig. 5A). It was also
observed that the HIF-1α expression level increased in the ischemic
region with increasing reperfusion time, and was significantly
higher in all five ischemic-reperfusion groups than that in the
sham group. The HIF-1α expression levels peaked in the group that
received reperfusion at 32 h after MCAO (P<0.01; Fig. 5B). By contrast, in the non-ischemic
regions, the mRNA transcription level of HIF-1α was unchanged at 16
h of reperfusion, although it increased in the group that received
reperfusion at 32 h and 64 h after MCAO (P<0.05, P<0.01;
Fig. 5B).
NGB protein levels in the ischemic
regions markedly increase with increasing reperfusion time and are
significantly higher for all ischemic-reperfusion groups compared
with the sham group
The protein levels of NGB peaked in the group that
received reperfusion at 32 h after MCAO (Fig. 6A). The NGB protein level in the
non-ischemic region also increased with increasing reperfusion time
and was significantly higher for all ischemic-reperfusion groups
compared with the sham group, while it was lower than that in the
ischemic region (Fig. 6A).
Regarding HIF-1α protein level in the ischemic regions, low levels
of expression were observed after 4 h reperfusion, and the
expression level markedly increased from 8 h of reperfusion until
64 h reperfusion, with maximal levels observed in the group that
received reperfusion at 32 h after MCAO (Fig. 6B). However, HIF-1α protein
expression was markedly lower in the non-ischemic regions (Fig. 6B).
Changes in SOD activity and MDA levels in
the serum following focal cerebral ischemia
SOD activity decreased with increasing reperfusion
time and rapidly increased in the group that received reperfusion
at 64 h after MCAO. (P<0.05, P<0.01; Table I). By contrast, serum MDA
concentrations increased with increasing reperfusion time and
decreased after 64 h reperfusion (P<0.05, P<0.01; Table I).
 | Table ISOD activity and MDA concentration in
the serum following different periods of ischemia reperfusion. |
Table I
SOD activity and MDA concentration in
the serum following different periods of ischemia reperfusion.
| Reperfusion time
(h) | Group
|
|---|
| SOD (U/ml) | MDA (nmol/ml) |
|---|
| Sham | 114.157±0.967 | 5.177±0.123 |
| 0 | 97.317±1.366a | 5.403±0.047 |
| 4 | 85.100±2.011b | 5.910±0.061a |
| 8 | 80.547±0.359b | 6.443±0.146b |
| 16 | 73.767±1.842b | 6.840±0.098b |
| 32 | 70.667±0.358b | 7.533±0.061b |
| 64 | 88.860±1.363b | 6.910±0.070b |
Discussion
In the present study, the necrotic zone produced by
cerebral ischemia was characterized, demonstrating an increase in
the number of hyperchromatic cells and NGB-positive cells in
cortical tissues. It was observed that NGB and HIF-1α mRNA and
protein expression levels increased with increasing reperfusion
time, with peak expression levels in the group that received
reperfusion at 32 h after MCAO. The expression levels of the two
proteins in the ischemic-reperfusion groups were significantly
different from those in the sham group. The measurements of serum
redox indices revealed that the SOD enzyme activity decreased with
increased reperfusion time, although it rapidly increased in the
group that received reperfusion at 32 h after MCAO. The MDA level,
by contrast, increased with increasing reperfusion time and
decreased in the group that received reperfusion at 32 h after
MCAO.
The present results indicated that mRNA and protein
levels of NGB increased in rat brain tissues between 4 h and 64 h
following focal cerebral ischemia, with significant transcriptional
and translational upregulation in the ischemic regions, although
not in the non-ischemic regions. These findings suggested that NGB
may be important in sensing and responding to focal cerebral
ischemia. In order to address whether proteins other than NGB were
upregulated in the MCAO model, HIF-1α levels were examined, and
changes in its mRNA and protein levels were observed. These results
demonstrated that HIF-1α expression patterns were similar to that
of NGB. Therefore, it was hypothesized that NGB is involved in the
hypoxic response to MCAO via upregulation of HIF-1α. Future studies
are required to examine the regulatory interactions between NGB and
HIF-1α, and more closely examine the signaling pathway governing
NGB expression in the MCAO model.
Redox index assays for SOD activity and MDA
concentration, revealed significant changes from 4 h of reperfusion
following focal cerebral ischemia. The direction of change in SOD
activity was opposite to that of MDA levels and similar to that of
changes in NGB expression. Therefore, the serum SOD and MDA changes
may be useful biomarkers for brain focal cerebral ischemia, as
these can be easily measured (15–17).
For patients with focal cerebral ischemia, the most effective way
to reduce further nerve damage is to administer reperfusion
treatment as soon as possible. However, even with advanced imaging
techniques, such as computed tomography (18) and magnetic resonance imaging
(19,20), early detection of focal cerebral
ischemia is difficult. According to the present experimental
results, the measurement of serum SOD activity may be a novel,
accurate and convenient diagnostic approach for identifying focal
cerebral ischemic pathology at an early stage.
In conclusion, NGB levels were upregulated following
focal cerebral ischemia, and were shown to increase with increasing
reperfusion time. The present findings provide preliminary evidence
that serum SOD activity and MDA concentrations may be used as
biomarkers of early focal cerebral ischemia, due to the simplicity
and accuracy of their assay methods.
Acknowledgments
The present study was supported by the National
Natural Science Foundation (grant nos. 81071055 and 30801249), the
Open Project of the Medical Neurobiology of State Key Laboratory
(grant no. 09-08) and the Military Medicine and Public Health
Research Project (grant no. 10BJZ04). The authors would like to
thank Sysbiomics Bioinformatics Co., Ltd. (Beijing, China) for
assistance with data analysis.
References
|
1
|
Burmester T, Weich B, Reinhardt S and
Hankeln T: A vertebrate globin expressed in the brain. Nature.
407:520–523. 2000. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schmidt M, Giessl A, Laufs T, Hankeln T,
Wolfrum U and Burmester T: How does the eye breathe? Evidence for
neuroglobin-mediated oxygen supply in the mammalian retina. J Biol
Chem. 278:1932–1935. 2003. View Article : Google Scholar
|
|
3
|
Zhang L, Li LH, Qu Y and Mu DZ:
Neuroglobin and hypoxic-ischemic brain damage. Zhongguo Dang Dai Er
Ke Za Zhi. 10:265–268. 2008.In Chinese. PubMed/NCBI
|
|
4
|
Zhang C, Wang C, Deng M, et al:
Full-length cDNA cloning of human neuroglobin and tissue expression
of rat neuroglobin. Biochem Biophys Res Commun. 290:1411–1419.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang CG, Li L, Deng MY and Xie F: Coding
region cDNA sequence cloning of rat neuroglobin gene, its
polymorphism feature and tissue expression profile analysis. Yi
Chuan Xue Bao. 28:997–1001. 2001.In Chinese. PubMed/NCBI
|
|
6
|
Dewilde S, Kiger L, Burmester T, et al:
Biochemical characterization and ligand binding properties of
neuroglobin, a novel member of the globin family. J Biol Chem.
276:38949–38955. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sun Y, Jin K, Peel A, Mao XO, Xie L and
Greenberg DA: Neuroglobin protects the brain from experimental
stroke in vivo. Proc Natl Acad Sci USA. 100:3497–3500. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Venis S: Neuroglobin might protect brain
cells during stroke. Lancet. 358:20552001. View Article : Google Scholar
|
|
9
|
Kriegl JM, Bhattacharyya AJ, Nienhaus K,
Deng P, Minkow O and Nienhaus GU: Ligand binding and protein
dynamics in neuroglobin. Proc Natl Acad Sci USA. 99:7992–7997.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pesce A, De Sanctis D, Nardini M, et al:
Reversible hexa- to penta-coordination of the heme Fe atom
modulates ligand binding properties of neuroglobin and cytoglobin.
IUBMB Life. 56:657–664. 2004. View Article : Google Scholar
|
|
11
|
Shang A, Feng X, Wang H, et al:
Neuroglobin upregulation offers neuroprotection in traumatic brain
injury. Neurol Res. 34:588–594. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shang A, Zhou D, Wang L, et al: Increased
neuroglobin levels in the cerebral cortex and serum after
ischemia-reperfusion insults. Brain Res. 1078:219–226. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Benazzouz A, Tai CH, Meissner W, Bioulac
B, Bezard E and Gross C: High-frequency stimulation of both zona
incerta and subthalamic nucleus induces a similar normalization of
basal ganglia metabolic activity in experimental parkinsonism.
FASEB J. 18:528–530. 2004.PubMed/NCBI
|
|
14
|
Zhu H and Yu JJ: Gene expression patterns
in the histopathological classification of epithelial ovarian
cancer. Exp Ther Med. 1:187–192. 2010.PubMed/NCBI
|
|
15
|
Hua JS, Li LP and Zhu XM: Effects of
moxibustion pretreating on SOD and MDA in the rat of global brain
ischemia. J Tradit Chin Med. 28:289–292. 2008. View Article : Google Scholar
|
|
16
|
Wang S, Zhou W, Wei M and Zhang G: Effects
of lead on NO, NOS, SOD, MDA in rat cerebral cortex. Wei Sheng Yan
Jiu. 31:226–228. 2002.In Chinese.
|
|
17
|
Wang Y, Fu X and Ma N: Relationship
between wound healing and TNF, MDA and SOD contents in granulation
tissues of rats in the first week. Zhonghua Zheng Xing Shao Shang
Wai Ke Za Zhi. 12:45–47. 1996.In Chinese. PubMed/NCBI
|
|
18
|
Tomizawa N, Maeda E, Akahane M, Torigoe R,
Kiryu S and Ohtomo K: Coronary CT angiography using the
second-generation 320-detector row CT: Assessment of image quality
and radiation dose in various heart rates compared with the
first-generation scanner. Int J Cardiovasc Imaging. 29:1613–1618.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Swenson DW, Nickel BJ, Boxerman JL, Klinge
PM and Rogg JM: Prenatal MRI characterization of brainstem glioma.
Pediatr Radiol. 43:1404–1407. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cheng DT, Meintjes EM, Stanton ME, et al:
Functional MRI of cerebellar activity during eyeblink classical
conditioning in children and adults. Hum Brain Mapp. 35:1390–1403.
2014. View Article : Google Scholar
|