Introduction
Platinum and taxane-based chemotherapy following
cyto-reductive surgery are the predominant approaches for the
treatment of advanced ovarian cancer (1). Although the majority of patients
respond well to primary chemotherapy, 75% will experience a relapse
and acquire drug-resistance (1).
Novel therapeutic strategies are, therefore, required in order to
improve the prognosis for such patients (2). Dasatinib is one such therapy that
targets the breakpoint cluster region-Abelson (BCR-ABL) fusion
protein and the Src family tyrosine kinases (SFKs) (3). SFKs consist of nine non-receptor
tyrosine kinases that share a similar structure (4). Cellular-Src kinase (c-Src) is
expressed in a number of types of cells. It is involved in numerous
signaling pathways, and in the formation and development of tumors
(5). Overexpression and activation
of c-Src has been observed in the development of certain solid
tumors, such as breast, colon, prostate, ovarian, pancreatic and
non-small cell lung cancer, and squamous cell carcinoma of the head
and neck (6–10). Budde et al (11) detected Src expression in 60 human
tumor cell lines and demonstrated that ovarian cancer cell lines
exhibited a moderate level of Src expression, compared with healthy
cell lines. A further study demonstrated Src overexpression and
activation in advanced-stage ovarian tumor cells (12). Similarly, c-Src and
phospho-Src-Y416 (p-Src; Tyr416) were shown to be overexpressed in
human ovarian cancer cells (13).
A number of different Src inhibitors have been analyzed in certain
tumors. Dasatinib is a multi-targeted inhibitor of the receptor
tyrosine kinases, Src and the BCR-ABL fusion protein (14). In June 2006, the Food and Drug
Administration approved the use of dasatinib for the treatment of
imatinib-resistant or imatinib-intolerant patients with chronic
myeloid leukemia, and for the treatment of patients with
Philadelphia-chromosome-positive acute lymphoblastic leukemia, who
may be resistant or intolerant to first-line treatments (15). Dasatinib therapy has been
investigated in other types of malignancies and the results
observed for the treatment of solid tumors are encouraging. A
number of studies have confirmed the effectiveness of dasatinib
treatment for solid tumors (16–21),
although few studies have focused on ovarian cancer. Therefore, the
effects of dasatinib on ovarian cancer remain unclear. Konecny
et al (22) examined the
effects of dasatinib in 34 human ovarian cancer cell lines and
demonstrated that 24/34 (71%) of representative ovarian cancer cell
lines were highly sensitive to dasatinib. Furthermore, additive and
synergistic interactions were observed, following treatment with
dasatinib and carboplatin or paclitaxel. Similar results were
presented by Teoh et al (23). However, the precise mechanisms
underlying the antitumor effects of, and the interactions between,
dasatinib and paclitaxel, such as cell survival, proliferation,
autophagy, microtubule stability, motility and tumor angiogenesis
remain unknown. The aim of the present study was to evaluate the
antitumor properties of dasatinib alone and in combination with
paclitaxel in ovarian cancer in vitro and in vivo.
The mechanisms underlying the interactions between dasatinib and
paclitaxel were also investigated.
Materials and methods
Drugs and reagents
In order to conduct an in vitro study,
dasatinib (Selleck Chemicals, Houston, TX, USA) was dissolved in
dimethylsulfoxide (DMSO; DaMao Chemical Reagent Factory, Tiangjin,
China) at 10 mmol/l and stored at −20°C. Frequent freeze-thawing
was avoided. In order to conduct an in vivo study, dasatinib
was diluted in sterile distilled water at 1 mg/ml, and stored at
4°C for <7 days. Paclitaxel (Bristol-Myers Squibb, New York
City, NY, USA) was diluted in 3 mg/ml sterile distilled water. The
rabbit polyclonal anti-Src (cat. no. 2108S; 1:100) and rabbit
polyclonal anti-phosphorylated Src (cat. no. 2101S; 1:60)
antibodies were purchased from Cell Signaling Technology, Inc.
(Danvers, MA, USA). The monoclonal mouse GAPDH antibody (cat. no
KC-5G5; 1:1,000) was purchased from Kangchen (Shanghai, China). The
goat-anti-rabbit secondary (cat. no. sc-2054; 1:1,000), and
goat-anti-mouse secondary (cat. no. sc-2005; 1:1,000) antibodies
were obtained from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA,
USA). A horseradish peroxidase (HRP) polymer-conjugated anti-rabbit
secondary antibody (cat. no. PV-6001; 1:1,000) was purchased from
ZSGB-BIO (Beijing, China), and Annexin V-fluorescein isothiocyanate
(FITC) was obtained from Merck Millipore (Darmstadt, Germany). An
Apoptosis Detection kit was purchased from EMD Millipore
(Billerica, MA, USA). DMSO, MTT, and polyvinylidene difluoride
(PVDF) membranes were purchased from Sigma-Aldrich (St. Louis, MO,
USA).
Cell lines and cell culture
The following six human ovarian cancer cell lines
were used for analysis: A2780, HO8910, OVCAR3, CAOV3 and COC1
(Collection Conservation Center of Wuhan University, Wuhan, China),
and SKOV3 (State Key Laboratory of Oncology in South China,
Guangzhou, China). All cell lines were cultured in Dulbecco's
modified Eagle's medium (DMEM; Thermo Fisher Scientific, Waltham,
MA, USA), supplemented with 5% heat-inactivated fetal bovine serum
(Guangzhou Ruite Bio-tec Co., Ltd., Guangzhou, China), penicillin
(50 U/ml), and streptomycin (50 µg/ml) (North China
Pharmaceutical Co., Ltd., Shijiazhuang, China). Cells were grown in
a humidified incubator with 5% CO2, at 37°C.
Western blot analysis
Cells were cultured in six-well plates for 24 h and
exposed to treatments when in the logarithmic growth phase. Cells
were harvested and total protein was isolated. Total protein (20–40
µg) was separated using electrophoresis, electrotransferred
to PVDF membranes and then probed with the primary antibodies in
Tris-buffered saline with Tween-20® (TBST; Bioeasy Co.,
Ltd., Shenzhen, China)-5% milk (1:1,000) overnight, at 4°C. The
membranes were incubated with a peroxidase-conjugated secondary
antibody in TBST-5% milk (1:3,000) for 1–2 h, at room temperature.
Protein detection was achieved using enhanced chemiluminescence
reagent and XAR film (Kodak, Rochester, NY, USA) according to the
manufacturer's instructions. Anti-GAPDH was used as a positive
control (24).
MTT assay
In order to measure cell viability and activity,
cells in the logarithmic growth phase were seeded in 96-well plates
(3,000 cells/well) and then treated with different drug
concentrations. Concentrations were selected according to
references (16,25,26)
and preliminary experiments, which demonstrated that dasatinib (10
mg/kg) and paclitaxel (15 mg/kg) had marked anti-ovarian cancer
effects. The following concentrations were used: Dasatinib (0.3125,
0.625, 1.25, 2.5, 5, 10 and 20 µmol/l), paclitaxel (1.25,
2.5, 5, 10 and 20 µmol/l) or a combination of dasatinib and
paclitaxel (250:1 or 500:1). Negative control cells were treated
with DMSO. Experiments were repeated three times. Following 72 h of
drug treatment, 10 µl of 5 mg⁄ml MTT was added to each well
for an additional 4 h of incubation at 37°C, in 5% CO2.
The medium was subsequently removed and 100 µl DMSO was
added to the cells. Plates were agitated gently for 10 min at 37°C
and absorbance at 570 nm was measured using a microplate reader
(Molecular Devices, West Berkshire, UK). Cytotoxicity was evaluated
by calculating the 50% inhibitory concentration (IC50),
and the additive or synergistic effects were assessed using
combination indices (CI). CI<1 indicated synergy, CI=1 indicated
additivity, and CI>1 indicated antagonism (24), calculated using Calcusyn 2.0
software (Biosoft, Cambridge, UK).
Apoptosis assays
A2780 and HO8910 cell lines were cultured in
six-well plates and treated with paclitaxel with or without
dasatinib for 48–72 h in culture medium (37°C, 5% CO2).
The cells were stained using an Annexin V-FITC Apoptosis Detection
kit. Subsequently, cell cycle and apoptosis were measured at 488
nm, using flow cytometry (Beckman Coulter, Brea, CA, USA). Data
were recorded as the percentage of cells in each phase of the cell
cycle.
Tumor xenografts
A total of 87 female BALB/c nude mice age, 5–6 weeks
old, weight, 18–20 g, were obtained from Hunan SJA Lab Animal Co.
Inc. (Hunan, China) and were maintained in specific pathogen-free
conditions. Experiments were approved by the animal care committee
of Sun Yat-sen University (Guangzhou, China) and were performed
under sterile conditions. Mice were housed in Sun Yat-sen
University Medical Animal Center and maintained in a 12 h
light/dark cycle with access to food and water. A2780 or HO8910
cell lines (5×106 cells) were subcutaneously injected
into both side flanks, using a 23-gauge needle (each cell line was
administered to two mice; Sun Yat-sun University Cancer Center).
Once the tumors had reached a mean diameter of 8–10 mm, the mice
were sacrificed and the tumor tissue was cut into 1–2-mm fragments
in serum-free DMEM, at 4°C. The tumor fragments were subsequently
transplanted subcutaneously into the flanks of recipient mice (42
mice were injected with the A2780 tumor fragments; 43 mice were
injected with the HO8910 tumor fragments). The whole
transplantation procedure was completed within 30–40 min. Tumor
size and animal weight were monitored every 2–3 days. Once tumor
volumes had reached 50–80 mm3 (mean diameter 3–5 mm,
following 7 days of inoculation), mice were randomly divided into
four groups of six, and treated intraperitoneally with one of the
following: Dasatinib only (10 mg/kg, five times a week); paclitaxel
only (15 mg/kg, once a week); combined dasatinib (10 mg/kg) and
paclitaxel (15 mg/kg); or negative control (sterile distilled
water). All treatments were administered for 4 weeks; dosage was
derived from references (16,25,26)
and preliminary experiments, which demonstrated that dasatinib (10
mg/kg) and paclitaxel (15 mg/kg) had marked anti-ovarian cancer
effects. Tumor volumes were calculated using the formula: volume
(mm2) = 0.5 x tumor length x tumor width2.
Mice were sacrificed by cervical dislocation and tumor size, tumor
weight, and mouse body weight were measured. Tumor tissues were
excised and tissue samples were divided: One section was fixed in
formalin (Guangzhou Chemical Reagent Factory, Guangzhou, China) for
immunohistochemistry analysis and a second section was fixed in
liquid nitrogen for western blotting. Tumor growth inhibitory rate
(TIR) was calculated as follows: (average tumor weight in control
group − average tumor weight in treatment group)/aver average tumor
weight in control group × 100%.
Immunohistochemistry
The xenograft tumor tissues were fixed in formalin,
embedded in paraffin, sliced into 4-µm sections, and
rehydrated using a graded alcohol series. Endogenous peroxidase
activity was blocked using 3% hydrogen peroxide (Guangzhou Chemical
Reagent Factory) in methanol, for 10 min. For antigen retrieval,
slides were heated in a pressure cooker in 10 mM citrate buffer (pH
6.0; Guangzhou Chemical Reagent Factory), for 10 min. The slides
were incubated with anti-Src antibody (1:100) or anti-P-Src
antibody (1:60) overnight, at 4°C. Slides were then incubated with
an HRP polymer-conjugated anti-rabbit secondary antibody for 30
min, at 37°C and the color was developed using diaminobenzidine for
5 min. The nucleus was counter-stained using Meyer's hematoxylin
(Guangzhou Chemical Reagent Factory). The negative control was
obtained by replacing the primary antibody with normal rabbit
immunoglobulin G. Human epithelial ovarian cancer slides were used
as positive controls. Tumor tissue, fixed in liquid nitrogen, was
pulverized in cell lysis buffer (1,000 µl; Guangzhou
Chemical Reagent Factory), on ice. Immediately, 1 mmol/l
phenylmeth-anesulfonylfluoride (Guangzhou Chemical Reagent Factory)
was added and the lysate was clarified twice by centrifugation at
12,000 × g and 4°C for 15 min. Western blotting was performed as
described previously.
Statistical analysis
Statistical analyses were performed using SPSS 17.0
(SPSS, Inc., Chicago, IL, USA). Student's t-test or Pearson's
chi-squared tests were performed as appropriate. Analysis of
variance (ANOVA) was used for repeated measurements (one-way ANOVA
or Kruskal-Wallis test). P<0.05 was considered to indicate a
statistically significant difference.
Results
Src and p-Src expression in ovarian
cancer cell lines
Src and p-Src expression levels were measured using
western blotting. The six ovarian cancer cell lines exhibited high
levels of Src and p-Src expression. A2780 and SKOV3 cells lines
demonstrated the highest Src expression levels, whilst the A2780
and HO8910 cell lines demonstrated the highest p-Src expression
levels (Fig. 1). Based on these
results, the A2780 and HO8910 cell lines were selected for further
analysis.
Paclitaxel activates the Src pathway in
ovarian cancer cells
p-Src expression was upregulated in a dose-dependent
manner. However, total Src protein expression was unaffected, in
A2780 and HO8910 cell lines, following treatment with paclitaxel.
For the A2780 cells, p-Src expression was greatest following 24 h
of treatment with 10 nmol/l paclitaxel. For HO8910 cells, p-Src
expression was greatest following 6 h of treatment with 5 nmol/l
(Fig. 2).
Dasatinib inhibits viability and enhances
paclitaxel cytotoxicity in ovarian cancer cells
The results of the present study demonstrated that
paclitaxel treatment activated Src expression in ovarian cancer
cells. Subsequently, the effect of dasatinib on the cytotoxicity of
paclitaxel was investigated in these cell lines. A2780 and HO8910
cell lines treated with increasing dasatinib concentrations
(0.3125-20 µM) demonstrated a dose-dependent reduction in
cell viability (Fig. 3A).
IC50 values were 7.30±0.64 µM in A2780 cells and
2.51±0.64 µM in HO8910 cells. Cell lines were sensitive to
paclitaxel treatment (IC50~20 nmol/l). Dasatinib
combined with paclitaxel demonstrated synergistic antitumor
activity with confidence interval (CI) values of 0.25–0.93 and
0.31–0.75 in A2780 and HO8910 cell lines, respectively (Table I). In addition, at concentrations
below the IC50, dasatinib suppressed Src and p-Src
protein expression (Fig. 3B). An
annexin V-FITC/propidium iodide apoptosis assay was conducted in
order to determine whether the cytotoxicity of dasatinib, with or
without paclitaxel treatment, is associated with changes in cell
apoptosis. Apoptosis rates in A2780 cells treated with 20 µM
and 40 µM dasatinib for 48 h, were 30.9±1.4 and 66.5±0.9%,
respectively. In HO8910 cells, these rates were 8.65±0.6 and
30.8±1.2% following 48 h of treatment, and 12.6±2.2 and 76.0±2.0%
following 72 h of treatment, respectively (P<0.05). A greater
percentage of apoptotic cells was observed following treatment with
dasatinib combined with paclitaxel, compared with cell treated with
dasatinib only. The apoptotic rates of A2780 cells following
treatment with 20 µM dasatinib, 0.02 µM paclitaxel,
and combined dasatinib and paclitaxel, for 48 h, were 34.7±3.4,
20.9±3.7 and 44.2±2.4%, respectively. Apoptotic rates were
17.3±2.1, 22.0±2.7 and 43.6±4.0% in HO8910 cells (all P<0.001
compared with control cells; Fig.
3C).
 | Table IEffects of dasatinib combined with
paclitaxel. |
Table I
Effects of dasatinib combined with
paclitaxel.
| A, A2780 ovarian
cancer cell line |
|---|
|
|---|
| Dasatinib
(µM) | Paclitaxel
(µM) | Fa | CI |
|---|
| 0.3125 | 0.0013 | 0.4089 | 0.330 |
| 0.6250 | 0.0025 | 0.4247 | 0.575 |
| 1.2500 | 0.0050 | 0.4650 | 0.817 |
| 2.5000 | 0.0100 | 0.5277 | 0.973 |
| 5.0000 | 0.0200 | 0.6903 | 0.483 |
| 10.000 | 0.0400 | 0.8178 | 0.245 |
| B, HO8910 ovarian
cancer cell line |
|---|
|
|---|
| Dasatinib
(µM) | Paclitaxel
(µM) | Fa | CI |
|---|
| 0.3125 | 0.0006 | 0.4713 | 0.402 |
| 0.625 | 0.0013 | 0.5130 | 0.526 |
| 1.25 | 0.0025 | 0.5500 | 0.746 |
| 2.5 | 0.0050 | 0.7395 | 0.308 |
| 5.0 | 0.0100 | 0.8294 | 0.257 |
| 10.0 | 0.0200 | 0.8229 | 0.553 |
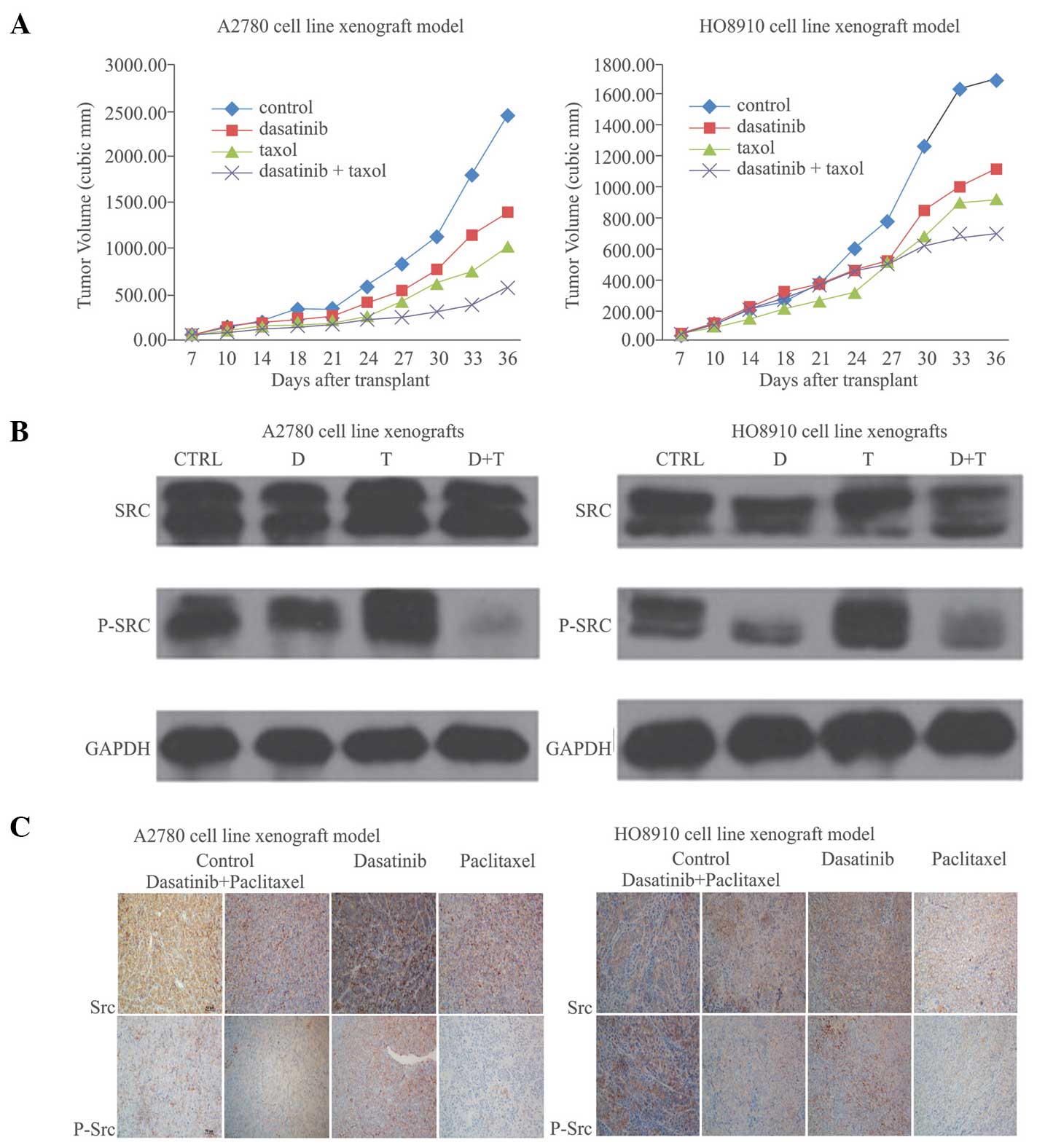
Antitumor activity of combined dasatinib
and paclitaxel in a human ovarian cancer xenograft model
A2780 and HO8910 xenografts were established in nude
mice in order to assess the potential antitumor effect of treatment
with dasatinib alone or with dasatinib in combination with
paclitaxel. In A2780 and HO8910 xenografts, dasatinib treatment led
to tumor growth inhibition by 43.2% (A2780) and 34.0% (HO8910;
Table II; Fig. 4A). Combined treatment led to a
greater growth inhibitory effect: TIRA2780 = 76.7% (P<0.001) and
TIRHO8910 = 58.5% (P<0.001) in comparison with single drug
treatments. The comparison of tumor-growth curves, using group and
time as variables, with a two-sided ANOVA, demonstrated that the
group-by-time interaction for tumor growth (F) was statistically
significant (FA2780 = 8.054, PA2780<0.001;
FHO8910 = 7.681, PHO8910 < 0.001). As shown in Table II, mouse weight was not
significantly different between groups (one-way ANOVA: FA2780 =
5.619, PA2780 = 0.162; FHO8910 = 0.6, PHO8910 = 0.794). Overall,
treatments appeared to be relatively well tolerated by the mice,
with no mortalities or weight loss, and no signs of acute or
delayed toxicity. Western blotting (Fig. 4B) and immunohistochemistry
(Fig. 4C) suggested that
paclitaxel activated and upregulated the Src pathway (p-Src
expression) in cancer cells, compared with that in the control
cells. Dasatinib combined with paclitaxel treatment downregulated
p-Src expression in cancer cells (23.3 vs. 31.0% in A2780 cells and
21.3 vs. 48.7% in HO8910 cells), as compared with dasatinib
treatment alone (Figs. 4B and C).
This is consistent with the results of the in vitro
study.
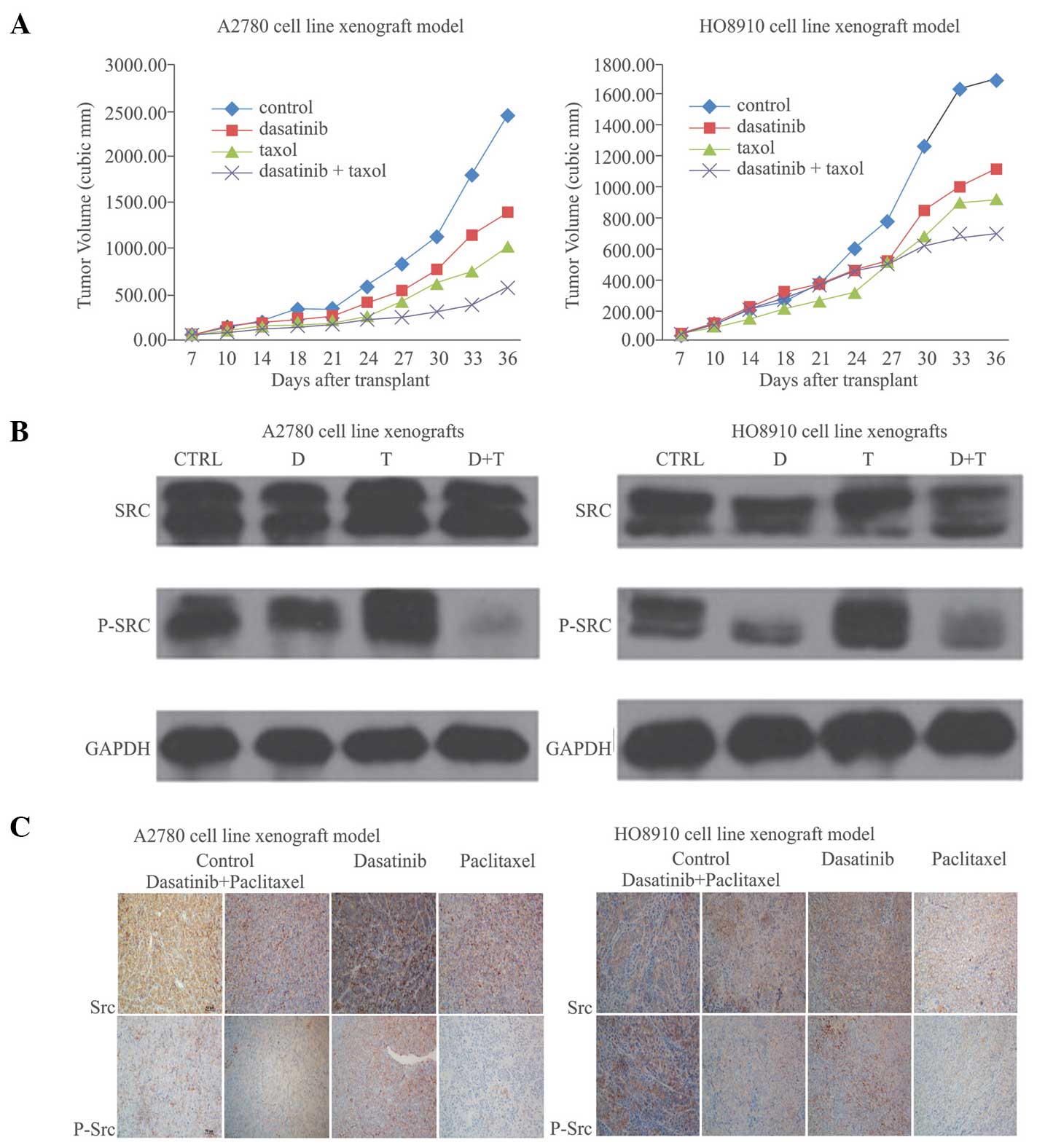 | Figure 4Antitumor activity of combined
dasatinib and paclitaxel in a human ovarian cancer xenograft model.
(A) Ovarian cancer xenograft growth curve. Mice bearing ovarian
cancer xenografts were treated as follows: Dasatinib alone (10
mg/kg five times a week); paclitaxel alone (15 mg/kg once a week);
combination of dasatinib (10 mg/kg per week); and paclitaxel (15
mg/kg per week); vehicle control (the same quantity of sterile
distilled water). P=0.003, dasatinib vs. control in A2780 cells;
P=0.004, combined treatment vs. dasatinib alone in A2780 cells;
P=0.087, combined treatment vs. paclitaxel in A2780 cells; P=0.024,
dasatinib vs. control in HO8910 cells; P=0.075, combined treatment
vs. dasatinib alone in HO8910 cells; P=0.281, combined treatment
vs. paclitaxel in HO8910 cells. Group-by-time interaction for tumor
growth was statistically significant (A2780, F=8.054 and
P<0.001; HO8910, F=7.681 and P<0.001). (B) Western blot
analysis of Src and p-Src protein in vivo. (C)
Immunohistochemistry of Src and p-Src protein expression in ovarian
cancer xenografts. p-Src, phospho-Src-Y416; CTR, control; D,
dasatinib; T, paclitaxel. |
 | Table IIBody weight, tumor weight and tumor
volume in ovarian cancer xenografts. |
Table II
Body weight, tumor weight and tumor
volume in ovarian cancer xenografts.
| A, A2780
xenografts |
|---|
|
|---|
| Treatment | n | Weight (g)
| Tumor volume | Tumor weight | TIR |
|---|
| Day 0 | Day 31 |
|---|
| Control | 5/8 | 20.88±0.18 | 22.47±0.89 | 2465.0±459.1 | 2.12±0.34 | |
| Dasatinib | 6/12 | 20.93±0.72 | 22.37±0.89 | 1400.2±231.3 | 1.67±0.30 | 43.197 |
| Paclitaxel | 6/11 | 21.17±0.45 | 23.08±0.72 | 1016.9±176.3 | 1.34±0.20 | 58.764 |
| Combined | 6/11 | 21.25±0.41 | 21.7±1.1 | 574.3±126.1 | 0.93±0.19 | 76.702 |
| B, HO8910
xenografts |
|---|
|
|---|
| Treatment | n | Weight (g)
| Tumor volume | Tumor weight | TIR |
|---|
| Day 0 | Day 31 |
|---|
| Control | 6/11 | 18.30±0.60 | 22.32±0.40 | 1695.2±162.5 | 2.65±0.28 | |
| Dasatinib | 6/10 | 19.10±0.66 | 20.88±0.58 | 1119±168.6 | 1.55±0.30 | 33.99 |
| Paclitaxel | 6/12 | 19.45±0.66 | 20.57±0.88 | 923.2±139.9 | 1.54±0.22 | 45.54 |
| Combined | 6/10 | 17.28±0.51 | 20.35±0.57 | 698.3±145.7 | 1.65±0.42 | 58.51 |
Discussion
Ovarian carcinoma is the leading cause of
reproductive-associated cancer mortality among females worldwide
(1). Despite high initial
remission rates using paclitaxel and platinum-based chemotherapy,
<75% of patients with advanced-stage ovarian carcinoma will
relapse (1). Targeted agents have
been the primary focus of treatment efforts for patients with
recurrent ovarian cancer. A number of studies have aimed to
investigate novel antitumor drugs that interfere with the critical
signaling pathways associated with the occurrence and progression
of ovarian cancer. Dasatinib is a competitive inhibitor of a number
of tyrosine kinases, including SFKs (27). A number of studies have suggested
that dasatinib alone or in combination with other drugs, such as
paclitaxel, exhibits preclinical antitumor activity in human
ovarian cancer (22,23,25).
However, the synergistic mechanisms associated with dasatinib
treatment combined with paclitaxel, remain unknown. The results of
the present study suggested that dasatinib treatment enhanced the
paclitaxel-associated antitumor activities in ovarian cancer cells.
This may be explained by the inhibitory effects of dasatinib on the
Src signal pathway.
Mayer and Krop (28) demonstrated that Src regulates a
number of signaling pathways that affect proliferation, survival,
migration, invasion and angiogenesis in tumor cells, and that Src
is activated and overexpressed in numerous types of solid tumors
(6–10,16,26,29).
The current study demonstrated overexpression of Src and p-Src in
human ovarian cancer tissues (13). In the present study, the Src
signaling pathway was activated, and p-Src was overexpressed in six
human ovarian cancer cell lines. Given the effect of Src signaling
on ovarian cancer, Konecny et al (22) studied 34 ovarian cancer cell lines
and demonstrated that dasatinib inhibits cell proliferation in
vitro with 0.001–11.3 µM IC50 values. In the
current study, dasatinib was found to inhibit ovarian cancer cell
proliferation. Low concentration dasatinib (IC50~8
µM) reduced cell proliferation, and Src and p-Src protein
expression levels were downregulated in response to dasatinib
treatment at varying concentrations and incubation times.
Therefore, dasatinib cytotoxicity in ovarian cancer may be
explained by the inhibition of Src pathway activation. Teoh et
al (23) suggested that
dasatinib caused a reduction in p-Src expression in ovarian cell
lines. The results of the present study confirm these findings.
Furthermore, the results of the current study suggested that
paclitaxel activated Src signaling in ovarian cancer cells. In the
current study, p-Src expression was upregulated in A2780 and HO8910
cell lines following treatment with different concentrations of
paclitaxel. However, Src protein expression was not upregulated.
These results were confirmed in the in vivo studies. Based
on the results of the present study, it is hypothesized that
primary and acquired resistance to paclitaxel in ovarian cancer may
be due to the activation of the Src signaling pathway, and the
associated cancer cell proliferation, angiogenesis, invasion and
dissemination.
A significant synergetic antitumor effect was
observed following treatment with a combination of dasatinib and
paclitaxel, which was associated with inhibition of Src pathway
activity. In accordance with the results of the in vitro
study, dasatinib suppressed the growth of ovarian cancer xenografts
in nude mice compared with the controls (TIR 43.2% in A2780 cells,
and 34.0% in HO8910 cells, both P<0.01). Furthermore, when
combined with paclitaxel, a synergistic antitumor effect was
observed in vitro (CI<1; TIR values were 76.7 and 58.5%
in A2780 cells and HO8910 cells, respectively, P<0.05). The
synergy between dasatinib and paclitaxel was associated with the
inhibition of p-Src protein expression. These results suggested
that paclitaxel exhibits antitumor activity in ovarian cancer, but
may also activate the Src signal pathway, which promotes cell
survival and drug resistance.
The mechanisms underlying dasatinib-enhanced
antitumor activity and the association with paclitaxel, remain
unclear. SFK inhibitors enhance paclitaxel sensitivity by inducing
cell apoptosis, autophagy, microtubule stability and neovasculature
(30). George et al
(31) demonstrated that Src
inhibition reduces the critical intracellular concentration at
which pacli-taxel induces tubulin stabilization and apoptosis.
Furthermore, Chen et al (32) demonstrated that Src inhibition
alone activates caspase-3 and promotes apoptosis. The results of
the present study suggested that dasatinib promoted apoptosis in a
mouse xenograft model. The results suggested that dasatinib
exhibited a dose- and time-dependent effect on the level of
apoptosis in ovarian cancer cell lines (both P<0.05). Therefore,
dasatinib is capable of enhancing apoptosis following paclitaxel
treatment.
The use of additive targets in cancer therapy, such
as the use of targeted agents in combination with cytotoxic drugs,
is becoming increasingly common. Ovarian cancer is highly
responsive to first-line chemotherapy, following optimal debulking
surgery. However, relapses are frequently observed in patients, due
to the development of resistance to conventional chemotherapy
drugs. Therefore, combination therapy may be useful for the
treatment of ovarian cancer (33).
Novel therapeutic agents in combination with conventional therapies
may prevent the emergence of resistance, thereby prolonging
remission and improving long-term survival. In the present study, a
synergistic effect was observed following treatment with a
combination of dasatinib and paclitaxel, in vitro and in
vivo. A number of studies have demonstrated that SFK inhibition
sensitizes cancer cells to paclitaxel-based treatments by
modulating cell survival and proliferation, autophagy, microtubule
stability, motility, and tumor angiogenesis (23,32,34–36).
Numerous mechanisms have been proposed in order to explain these
observations.
The present study demonstrated that p-Src expression
levels were markedly increased following paclitaxel treatment.
Therefore, paclitaxel activates Src signaling. However, dasatinib
treatment appeared to suppress p-Src expression, in vitro
and in vivo. Similarly, a separate study demonstrated that
oxaliplatin activates Src signaling via a reactive oxygen
species-dependent mechanism, and a trend was observed between the
degree of Src activation following oxaliplatin treatment and the
degree of synergy between dasatinib and oxaliplatin (37). Furthermore, acquired and persistent
resistance to paclitaxel is associated with upregulation of
Multi-Drug Resistance (MDR)-1, increased DNA damage tolerance and
drug metabolism, altered micro-tubule isotype expression and
mutations of β-tubulin (31). The
inhibition of certain SFKs eliminated the resistance of ovarian
cancer cells via an MDR-independent mechanism. However, the
pathways underlying this process remain unclear (31). A study has shown that dasatinib may
enhance paclitaxel sensitivity by suppressing B cell lymphoma-2 and
cyclin dependent kinase 1 expression in ovarian cancer cells via a
p27(Kip1)-dependent process (34).
The mechanisms involved in the paclitaxel-activated Src pathway are
unclear. However, it is clear that this activation is a primary
factor in the synergistic effects of combined dasatinib and
paclitaxel treatment in ovarian cancer. The present study suggested
that dasatinib increased the cytotoxicity of paclitaxel in ovarian
cancer, possibly a result of dasatinib-driven inhibition of
paclitaxel-induced Src activity. Therefore, in response to
dasatinib treatment, apoptosis was enhanced and paclitaxel
resistance was delayed in ovarian cancer cells.
The preclinical data in the present study suggests
that dasatinib is a potential therapeutic agent for ovarian cancer.
When combined with paclitaxel, dasatinib is able to further enhance
anti-ovarian cancer activity, and may delay or prevent paclitaxel
resistance.
Acknowledgments
The authors would like to thank Professor Xiaofeng
Zhu for his support in conducting this study. The study was funded
by The Natural Science Foundation of Guangdong Province
(S2013010015575).
References
|
1
|
Jelovac D and Armstrong DK: Recent
progress in the diagnosis and treatment of ovarian cancer. CA
Cancer J Clin. 61:183–203. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2012. CA Cancer J Clin. 62:10–29. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shah NP, Tran C, Lee FY, Chen P, Norris D
and Sawyers CL: Overriding imatinib resistance with a novel ABL
kinase inhibitor. Science. 305:399–401. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yeatman TJ: A renaissance for SRC. Nat Rev
Cancer. 4:470–480. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Brunton VG and Frame MC: Src and focal
adhesion kinase as therapeutic targets in cancer. Curr Opin
Pharmacol. 8:427–432. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wheeler DL, Iida M and Dunn EF: The role
of Src in solid tumors. Oncologist. 14:667–678. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Summy JM and Gallick GE: Src family
kinases in tumor progression and metastasis. Cancer Metastasis Rev.
22:337–358. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dehm SM and Bonham K: SRC gene expression
in human cancer: The role of transcriptional activation. Biochem
Cell Biol. 82:263–274. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Morgan L, Nicholson RI and Hiscox S: SRC
as a therapeutic target in breast cancer. Endocr Metab Immune
Disord Drug Targets. 8:273–278. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lutz MP, Esser IB, Flossmann-Kast BBM, et
al: Overexpression and activation of the tyrosine kinase Src in
human pancreatic carcinoma. Biochem Biophys Res Commun.
243:503–508. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Budde RJ, Ke S and Levin VA: Activity of
pp60c-src in 60 different cell lines derived from human tumors.
Cancer Biochem Biophys. 14:171–175. 1994.PubMed/NCBI
|
|
12
|
Wiener JR, Windham TC, Estrella VC, et al:
Activated SRC protein tyrosine kinase is overexpressed in
late-stage human ovarian cancers. Gynecol Oncol. 88:73–79. 2003.
View Article : Google Scholar
|
|
13
|
Huang YW, Chen C, Xu MM, Li JD, Xiao J and
Zhu XF: Expression of c-Src and phospho-Src in epithelial ovarian
carcinoma. Mol Cell Biochem. 376:73–79. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lombardo LJ, Lee FY, Chen P, et al:
Discovery of N-(2- chloro- 6- methyl- phenyl)- 2-(6-(4-(2-
hydroxyethyl)-piperazin - 1- yl)- 2- methylpyrimidin- 4-
ylamino)thiazole- 5- carboxamide (BMS- 354825), a dual Src/Abl
kinase inhibitor with potent antitumor activity in preclinical
assays. J Med Chem. 47:6658–6661. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gnoni A, Marech I, Silvestris N, Vacca A
and Lorusso V: Dasatinib: an anti-tumour agent via Src inhibition.
Curr Drug Targets. 12:563–578. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nam S, Kim D, Cheng JQ, et al: Action of
the Src family kinase inhibitor, dasatinib (BMS-354825), on human
prostate cancer cells. Cancer Res. 65:9185–9189. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Johnson FM, Saigal B, Talpaz M and Donato
NJ: Dasatinib (BMS-354825) tyrosine kinase inhibitor suppresses
invasion and induces cell cycle arrest and apoptosis of head and
neck squamous cell carcinoma and non-small cell lung cancer cells.
Clin Cancer Res. 11:6924–6932. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ceppi P, Papotti M, Monica V, et al:
Effects of Src kinase inhibition induced by dasatinib in non-small
cell lung cancer cell lines treated with cisplatin. Mol Cancer
Ther. 8:3066–3074. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tsao AS, He D, Saigal B, et al: Inhibition
of c-Src expression and activation in malignant pleural
mesothelioma tissues leads to apoptosis, cell cycle arrest, and
decreased migration and invasion. Mol Cancer Ther. 6:1962–1972.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Trevino JG, Summy JM, Lesslie DP, et al:
Inhibition of SRC expression and activity inhibits tumor
progression and metastasis of human pancreatic adenocarcinoma cells
in an orthotopic nude mouse model. Am J Pathol. 168:962–972. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shor AC, Keschman EA, Lee FY, et al:
Dasatinib inhibits migration and invasion in diverse human sarcoma
cell lines and induces apoptosis in bone sarcoma cells dependent on
SRC kinase for survival. Cancer Res. 67:2800–2808. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Konecny GE, Glas R, Dering J, et al:
Activity of the multikinase inhibitor dasatinib against ovarian
cancer cells. Br J Cancer. 101:1699–1708. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Teoh D, Ayeni TA, Rubatt JM, Adams DJ,
Grace L and Starr MD: Dasatinib (BMS-35482) has synergistic
activity with paclitaxel and carboplatin in ovarian cancer cells.
Gynecol Oncol. 121:187–192. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Deng R, Tang J, Xia LP, et al: ExcisaninA,
a diterpenoid compound purified from Isodon MacrocalyxinD, induces
tumor cells apoptosis and suppresses tumor growth through
inhibition of PKB/AKT kinase activity and blockade of its signal
pathway. Mol Cancer Ther. 8:873–882. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Le XF, Mao W, Lu Z, Carter BZ and Bast RC
Jr: Dasatinib induces autophagic cell death in human ovarian
cancer. Cancer. 116:4980–4990. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Vitali R, Mancini C, Cesi V, et al:
Activity of tyrosine kinase inhibitor Dasatinib in neuroblastoma
cells in vitro and in orthotopic mouse model. Int J Cancer.
125:2547–2555. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kim LC, Rix U and Haura EB: Dasatinib in
solid tumors. Expert Opin Investig Drugs. 19:415–425. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mayer EL and Krop IE: Advances in
targeting SRC in the treatment of breast cancer and other solid
malignancies. Clin Cancer Res. 16:3526–3532. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yezhelyev MV, Koehl G, Guba M, et al:
Inhibition of SRC tyrosine kinase as treatment for human pancreatic
cancer growing orthotopically in nude mice. Clin Cancer Res.
10:8028–8036. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Le XF and Bast RC Jr: Src family kinases
and paclitaxel sensitivity. Cancer Biol Ther. 12:260–269. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
George JA, Chen T and Taylor CC: SRC
tyrosine kinase and multidrug resistance protein-1 inhibitions act
independently but cooperatively to restore paclitaxel sensitivity
to paclitaxel-resistant ovarian cancer cells. Cancer Res.
65:10381–10388. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen T, Pengetnze Y and Taylor CC: Src
inhibition enhances paclitaxel cytotoxicity in ovarian cancer cells
by caspase-9-independent activation of caspase-3. Mol Cancer Ther.
4:217–224. 2005.PubMed/NCBI
|
|
33
|
Agarwal R and Kaye SB: Ovarian cancer:
strategies for overcoming resistance to chemotherapy. Nat Rev
Cancer. 3:502–516. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Le XF, Mao W, He G, et al: The role of
p27(Kip1) in dasatinib-enhanced paclitaxel cytotoxicity in human
ovarian cancer cells. J Natl Cancer Inst. 103:1403–1422. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Han LY, Landen CN, Trevino JG, et al:
Antiangiogenic and antitumor effects of SRC inhibition in ovarian
carcinoma. Cancer Res. 66:8633–8639. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kim HS, Han HD, Armaiz-Pena GN, et al:
Functional roles of Src and Fgr in ovarian carcinoma. Clin Cancer
Res. 17:1713–1721. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kopetz S, Lesslie DP, Dallas NA, et al:
Synergistic activity of the SRC family kinase inhibitor dasatinib
and oxaliplatin in colon carcinoma cells is mediated by oxidative
stress. Cancer Res. 69:3842–3849. 2009. View Article : Google Scholar : PubMed/NCBI
|