Introduction
In animals with hypertension-induced renal injury,
excessive accumulation of oxygen free radicals was observed
together with down-regulation of antioxidase, indicating that
oxidative stress has a crucial role in hypertension-induced renal
injury (1). Reactive oxygen
species (ROS), including superoxide radicals, hydrogen peroxide and
hydroxyl radicals, have been reported to be closely associated with
the pathogenesis of hypertension and renal damage (2,3). The
underlying mechanisms may be as follows: i) ROS affects vascular
resistance via inactivating nitric oxide, resulting in arteriolar
vasoconstriction and elevation of peripheral hemodynamic
resistance; and ii) ROS may cause lesions in renal tissues
(4).
Increasing evidence has revealed that hypertension
is an independent risk factor for end-stage renal disease (5,6).
However, the exact mechanism has remained to be sufficiently
defined. It has been indicated that oxygen free radicals are able
to trigger the elevation of blood pressure by inactivating nitric
oxide, which finally raises the systemic vascular resistance
(7). Reactive oxygen species also
induce cellular injury and contribute to fibrosis and formation of
atherogenic oxidized lipoproteins (8). Based on these facts, the present
study hypothesized that the hypertension-induced renal injury is,
at least in part, due to elevated generation of oxygen free
radicals.
Melatonin (MLT) has been reported to ameliorate
renal ischemic re-perfusion injury through its radical-scavenging
activity (9,10). However, only few studies have been
conducted to investigate its roles in hypertension-induced renal
injury (11). The present study
aimed to investigate the roles of MLT in hypertensive rats with
renal damage.
Materials and methods
Animals
Healthy male Wistar rats (weighing 180–220 g) were
purchased from the Laboratory Animal Center of Shanxi Medical
University (Taiyuan, China). The rats were housed with a 12 h
light/dark cycle, at 37°C, in an atmosphere containing 75%
humidity. All animal were provided with ad libitum access to
food and water. All the experiments were performed according to the
Principles of Laboratory Animal Care (NIH Publication no. 86–23,
revised 1985) and the regulation of the Committee on the Use and
Care of Animals of Fudan University (Shanghai, China), and approved
by the Ethics Committee of the Shanxi Medical University (Taiyuan,
China).
Preparation of hypertensive rats
The animals were subjected to occlusion of the left
renal artery as previously described (12). In brief, the rats were anesthetized
using 10% chloral hydrate. The renal artery of the left kidney was
exposed and clipped with an artery clamp. In the sham control
group, a sham procedure, which included the entire surgery expect
the artery clipping, was applied.
Experimental design
Rats were divided into a sham control group (n=8),
which was subjected to sham operation and received vehicle
treatment (physiological saline intraperitoneally at 0.1 ml/100 g),
a vehicle group (n=8), which was subjected to occlusion of the left
renal artery and vehicle treatment, and the MLT group (n=8), which
was subjected to occlusion of the left renal artery and injected
intraperitoneally with MLT (10 mg/kg/day; Cayman Chemical Company,
Ann Arbor, MI, USA). The animals were sacrificed with 10% chloral
hydrate (Huayueyang Biotech Co. Ltd., Beijing, China) at week 12
after treatment.
Creatinine assay
Determination of serum creatinine was performed by
Jaffe's reaction (13). In brief,
aortic blood samples were obtained and centrifuged to separate the
serum. Serum creatinine was determined with an automated system
(Express 550 Analyzer; Ciba Corning Diagnostic Corp, East Walpole,
MA, USA).
Determination of urine protein
Urine samples were collected 24 h prior to
scarification of the animals with sterilized devices (Metrical GRID
Trade Co., Ltd, Kunshan, China). The urine protein concentration
was determined using the Coomassie Brilliant Blue G-250 (product
code B-0770; Sigma-Aldrich, St. Louis, MO, USA) method as
previously described (14).
Malondialdehyde (MDA) assay and
superoxide dismutase (SOD) assay
MDA in the renal tissues was determined using a kit
purchased from Abcam (Cambridge, UK; cat. no. ab118970) according
to the manufacturer's instructions. The activity of SOD was
determined using the SOD assay kit (cat. no. KT-034; Kamiya
Biomedical Company, Seattle, WA, USA) using the V-5100H
spectrophotometer (Shanghai Metash Instruments Co., Ltd., Shanghai,
China).
Pathological analysis
For the pathological analysis, the renal tissues
were treated using conventional procedures, including formalin
fixation, dehydration and embedding. Subsequently, the sections (3
µm) were stained using hematoxylin and eosin (H&E; Alfa
Aesar, Shanghai, China) and Masson's trichrome (Sigma-Aldrich),
respectively. The pathological results were evaluated by two
members of staff blinded to the study. The degree of injury was
evaluated according to the damaged area of renal tubules using the
following scoring system: 0, no injury; 1, injury in <10%; 2,
injury in 11–25%; 3, injury in 26–45%; 4, injury in 46–75%; and 5,
injury in >75% of the observed area. The evaluation was
performed in 10 randomly selected fields in each slice, and was
observed under a magnification of 200x.
Reverse-transcription polymerase chain
reaction (RT-PCR) analysis
In the present study, the mRNA expression of heme
oxygenase-1 (HO-1), intercellular adhesion molecule-1 (ICAM-1),
inducible nitric oxide synthase (iNOS) and endothelial nitric oxide
synthase (eNOS) was determined using RT-PCR amplification. Total
RNA was extracted using TRIzol reagent TRIzol (Invitrogen Life
Technologies, Shanghai, China). according to the manufacturer's
instructions. The first-strand cDNA was synthesized with a random
primer (Sangon Biotech Co., Ltd., Shanghai, China) using the
SuperScript III reverse transcriptase (Invitrogen Life
Technologies, Carlsbad, CA, USA). PCR amplification was performed
using the primers and amplification conditions listed in Table I. GAPDH was amplified under the
same reaction conditions, accordingly, to serve as the internal
standard. Finally, the PCR products were electrophoresed on 1.5%
agarose gels and analyzed using a Gel Documentation
E-Gel® Imager system (Invitrogen Life Technologies).
 | Table IPrimer sequences and amplification
conditions of reverse transcription polymerase chain reaction. |
Table I
Primer sequences and amplification
conditions of reverse transcription polymerase chain reaction.
| Gene | Primer sequence
(5′–3′) | Amplification
conditions |
|---|
| iNOS | F,
CAGGTGCTATTCCCAGCCCAACA
R, CATTCTGTGCAGTCCCAGTGAGGAA | 94°C for 3 min; 30
cycles of 94°C for 30 sec,
61°C for 30 sec and 72°C for 60 sec; 72°C for 5 min |
| eNOS | F,
TTCTGGCAAGACCGATTACACGACAT
R, AAAGGCGGAGAGGACTTGTCCAAA | 94°C for 3 min; 30
cycles of 94°C for 30 sec,
55°C for 30 sec and 72°C for 60 sec; 72°C for 5 min |
| HO-1 | F,
GGGAAGGCCTGGCTTTTTT
R, CACGATAGAGCTGTTTGAACTTGGT | 94°C for 3 min; 30
cycles of 94°C for 30 sec,
56°C for 30 sec and 72°C for 60 sec; 72°C for 5 min |
| ICAM-1 | F,
GTGAGCGTCCATATTTAGGCATGG
R, ACAGACACTAGAGGAGTGAGCAGG | 94°C for 3 min; 30
cycles of 94°C for 30 sec, 59.6°C
for 30 sec and 72°C for 60 sec; 72°C for 5 min |
| GAPDH | F,
AACGACCCCTTCATTGAC
R, TCCACGACATACTCAGCAC | 94°C for 3 min; 30
cycles of 94°C for 30 sec, 57.8°C
for 30 sec and 72°C for 60 sec; 72°C for 5 min |
Immunohistochemical analysis
Immunohistochemical analysis based on the
Streptavidin-Biotin Complex was performed according to a previously
published method (15). The
primary antibodies were HO-1 (1:300; cat. no. sc-136960; Santa Cruz
Biotechnology, Inc., Dallas, TX, USA), ICAM-1 (1:150; cat. no.
sc-1511; Santa Cruz Biotechnology, Inc.), iNOS (1:100; cat. no.
sc-650; Santa Cruz Biotechnology, Inc.) and eNOS (1:200; ab195944;
Abcam). β-Actin (1:200; cat. no. sc-130301; Santa Cruz
Biotechnology, Inc.) served as the loading control. Horseradish
peroxidase-conjugated secondary antibodies were purchased from the
Gene Tex Inc. (Irvine, CA, USA).
Statistical analysis
The data are presented as the mean ± standard
deviation. Student's t-test and χ2 test were performed
to carry out inter-group comparisons. Data analysis was performed
using SPSS 16.0 software (SPSS, Inc., Chicago, IL, USA). P<0.05
was considered to indicate a statistically significant
difference.
Results
MLT attenuates hypertension-associated
increases in blood pressure
The blood pressure in each group was monitored at
weeks 0, 4, 6, 8 and 12 of MLT treatment. Compared with the sham
control group, a significant increase in blood pressure was
observed in the vehicle group at weeks 4, 6, 8 and 12 (P<0.01)
(Fig. 1). In the MLT group, a
significant increase in blood pressure was observed at weeks 4, 6
and 8 (P<0.05). However, MLT treatment significant attenuated
the hypertension-induced increase in blood pressure at week 12
compared with that in the vehicle group (P<0.01).
MLT attenuates hypertension-induced
increases in urine protein excretion and serum creatinine
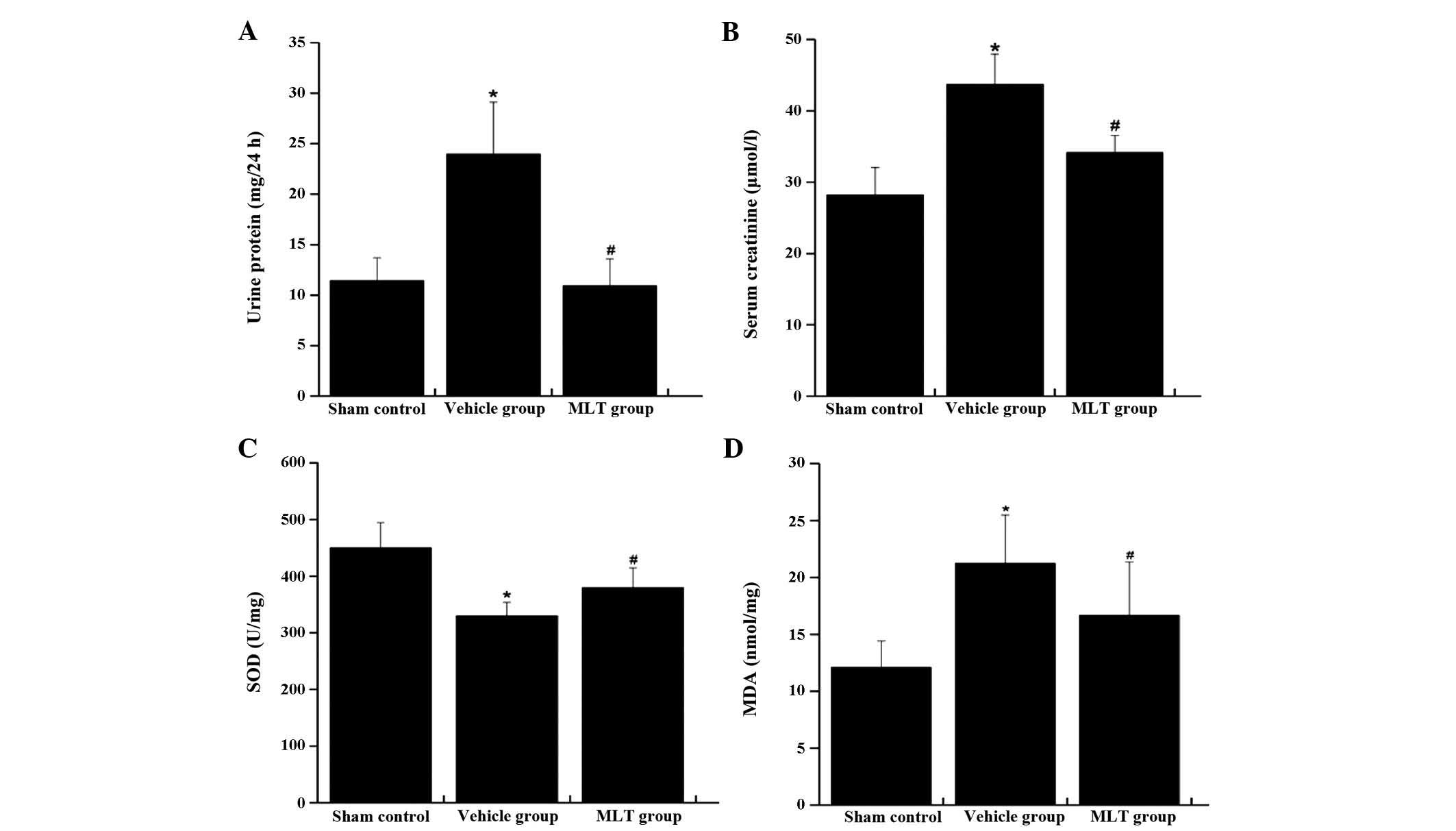
The excretion of urine protein and the concentration
of serum creatinine were markedly elevated in the vehicle group
compared with those in the sham control group (P<0.01) (Fig. 2A and B). In the group treated with
MLT, the increases in urine protein and serum creatinine were
attenuated compared with those in the vehicle group (P<0.01)
(Fig. 2A and B).
MLT attenuates hypertension-induced
decreases of SOD and increases of MDA in renal tissues
The SOD activity in renal tissues showed marked
decrease in the vehicle group compared with that in the sham
control group (P<0.01) (Fig.
2C). In the vehicle group, the expression of MDA was markedly
increased compared with that in the sham control group (P<0.01)
(Fig. 2D). Of note, the activity
of SOD was rescued and the expression of MDA was attenuated by
treatment with MLT (P<0.05).
MLT reduces the infiltration of
inflammatory cells and oedema/atrophy of renal tubules after
hypertension-induced renal injury
H&E staining and Masson's staining was performed
to determine the pathological features of the renal tissues. In the
sham control group, the renal tissues were clearly presented, and
the renal tubular epithelial cells were intact and aligned in
order. In the vehicle group, vacuolar degeneration and granular
degeneration was revealed in the renal tubular epithelial cells.
Infiltration of inflammatory cells, oedema and atrophy of renal
tubules were also observed. Of note, these pathological changes
were attenuated in the group treated with MLT (Fig. 3).
MLT modulates the expression of iNOS,
eNOS, HO-1 and ICAM-1
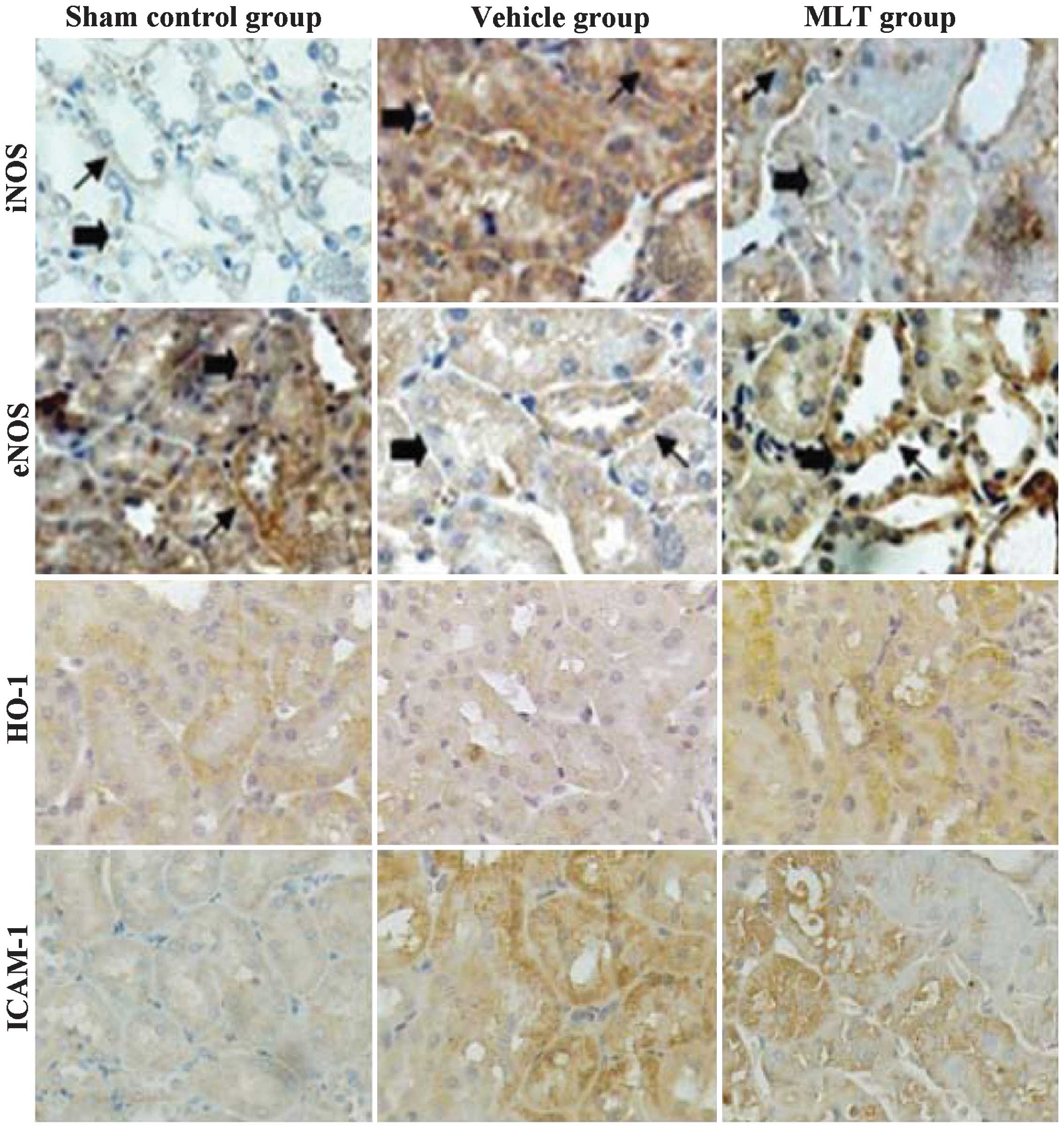
Immunohistochemical analysis showed that iNOS, eNOS,
HO-1 and ICAM-1 were mainly expressed in the cytoplasm of the renal
tubular epithelial cells (Fig. 4).
A minority of iNOS protein was detected in the nuclei as well. In
addition, ICAM-1 was also detected in renal parenchyma. In the sham
control group, the expression of ICAM-1 and iNOS was weakly
positive; however, their expression was enhanced in the
hypertensive rats. Compared with the vehicle group, the expression
of iNOS and ICAM-1 was significantly attenuated in the MLT group.
The expression of HO-1 and eNOS was significantly decreased in the
vehicle group compared with that in the sham control group.
However, in the rats treated with MLT, the expression of HO-1 and
eNOS was significantly increased compared with that in the vehicle
group. In parallel with the protein expression of iNOS, eNOS, HO-1
and ICAM-1, RT-PCR showed the same effects of hypertension and MLT
treatment on the associated mRNA expression levels (Fig. 5): iNOS and ICAM-1
mRNA was elevated in the hypertensive rats compared with that in
the animals of the sham control group, while these increases were
attenuated by treatment with MLT. With regard to the mRNA
expression of HO-1 and eNOS, a significant decrease was observed in
the hypertensive rats, which was rescued by MLT treatment
(P<0.01).
Discussion
Oxidative stress has been considered to have
important roles in the genesis and development of
hypertension-induced renal injury (16). The present study aimed to
investigate the protective effects of MLT, an effective
anti-oxidant, in hypertensive rats. The results indicated that MLT
attenuated in creases in blood pressure as well as renal injury in
hypertensive rats.
Proteinuria has been reported to be clearly
associated with an increased risk of mortality in patients with
chronic kidney disease (17). To
date, urine protein and serum creatinine have been recognized as
effective screening tools for the substantial risks associated with
proteinuria (18,19). In the present study, the excretion
of urine protein and serum creatinine was elevated in the vehicle
group at week 12, indicating reduced renal function. Pathological
analysis at week 12 indicated severe injury of the right renal
tubule, which was characterized by an aberrant structure, vacuolar
degeneration and granular degeneration of renal tubular epithelial
cells, infiltration of inflammatory cells, as well as oedema and
atrophy of the renal tubules. Of note, in the group treated with
MLT, the excretion of urine protein and the concentration of serum
creatinine was markedly reduced compared with that in the vehicle
group. In addition, the pathological changes were attenuated,
including alleviation of vacuolar degeneration, granular
degeneration of renal tubular epithelial cells and oedema of renal
tubules. All of these results demonstrated that MLT exerted a
protective effect against renal injury in hypertensive rats.
In a previous study, abnormalities in the lipid
peroxidation were observed in patients with renal disorders
(20). MDA is a product of lipid
peroxidation induced by oxidants and oxidative stress (21), and has been speculated to have
important roles in the pathogenesis of renal diseases. In the
present study, the generation of MDA in renal tissues was elevated
in the vehicle group, indicating that oxidative stress generated in
the kidneys also contributed to the elevation of blood pressure.
However, the increases of MDA were attenuated in the group treated
with MLT. SOD constitutes the first line of defence against
reactive oxygen species (22). In
the present study, the activity of SOD was markedly increased in
the MLT group compared with that in the vehicle group. All of these
results indicated that MLT reduced oxidative stress in renal
tissues.
In normal renal tissues, the expression of iNOS is
comparatively low; however, in renal tissues with pathologic
disorders, its expression is significantly upregulated, and is
considered the main source for the generation of nitric oxide,
which is a major effector molecule of hypertension (23). Under normal pathological
conditions, eNOS is the major source of nitric oxide; however, in
renal tissues with pathological lesions, a de-coupling process of
eNOS was induced, which resulted in the generation of
O2− (24). Finally,
massive apoptosis and necrosis were reported in renal tubular
epithelial cells following hypertension (24). In the present study, the expression
of iNOS was markedly upregulated in the hypertensive vehicle group,
which was attenuated in the group treated with MLT. With regard to
eNOS, the expression in the vehicle group was markedly
downregulated, which was attenuated in the group treated with MLT.
Based on these results, it was speculated that the mechanism of
action of MLT may involve the elevated generation of nitric oxide
in renal tubular epithelial cells through downregulating the
generation of iNOS and upregulation of eNOS in renal tissues,
finally resulting in a decrease in blood pressure and attenuation
of renal tubular injury.
The expression of ICAM-1 reflects the infiltration
of inflammatory cells (25). In
the vehicle group, the expression of ICAM-1 was markedly increased,
which was attenuated in the group treated with MLT. HO-1 has been
reported to have protective effects in renal tissues, serving as
the rate-limiting enzyme of catalyzing hemocrystallin into
biliverdin and carbon monoxide (26). In the present study, the expression
of HO-1 was markedly reduced in the vehicle group compared with
that in the sham control. However, treatment with MLT rescued HO-1
levels following hypertension. It is therefore speculated that MLT
has protective effects against renal injury through inhibiting the
infiltration of inflammatory cells and enhancing the expression of
HO-1.
In conclusion, MLT was able to alleviate
hypertension and associated renal injury in rats. This protective
effect may be associated with the reduction of oxidative stress,
inhibition of infiltration of inflammatory cells and the
enhancement of anti-oxidant molecules by MLT.
References
|
1
|
Zhou XJ, Laszik Z, Wang XQ, Silva FG and
Vaziri ND: Association of renal injury with increased oxygen free
radical activity and altered nitric oxide metabolism in chronic
experimental hemosiderosis. Lab Invest. 80:1905–1914. 2000.
View Article : Google Scholar
|
|
2
|
Swei A, Lacy FA, DeLano FA and
Schmid-Schönbein GW: Oxidative stress in the Dahl hypertensive rat.
Hypertension. 30:1628–1633. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shah SV, Baliga R, Rajapurkar M and
Fonseca VA: Oxidants in chronic kidney disease. J Am Soc Nephrol.
18:16–28. 2007. View Article : Google Scholar
|
|
4
|
Uehara Y, Kawabata Y, Shirahase H, Wada K,
Hashizume Y, Morishita S, Numabe A and Iwai J: Oxygen radical
scavengers and renal protection by indapamide diuretic in
salt-induced hypertension of Dahl strain rats. J Cardiovasc
Pharmacol. 22(Suppl 6): S42–S46. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ferguson R and Morrissey E: Risk factors
for end-stage renal disease among minorities. Transplant Proc.
25:2415–2420. 1993.PubMed/NCBI
|
|
6
|
Tozawa M, Iseki K, Iseki C, Kinjo K,
Ikemiya Y and Takishita S: Blood pressure predicts risk of
developing end-stage renal disease in men and women. Hypertension.
41:1341–1345. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vaziri ND, Liang K and Ding Y: Increased
nitric oxide inactivation by reactive oxygen species in
lead-induced hypertension. Kidney Int. 56:1492–1498. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vaziri ND, Oveisi F and Ding Y: Role of
increased oxygen free radical activity in the pathogenesis of
uremic hypertension. Kidney Int. 53:1748–1754. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tan DX, Manchester LC, Terron MP, Flores
LJ and Reiter RJ: One molecule, many derivatives: A never-ending
interaction of melatonin with reactive oxygen and nitrogen species?
J Pineal Res. 42:28–42. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sener G, Sehirli AO, Keyer-Uysal M, Arbak
S, Ersoy Y and Yegen BC: The protective effect of melatonin on
renal ischemia-reperfusion injury in the rat. J Pineal Res.
32:120–126. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nava M, Quiroz Y, Vaziri N and
Rodríguez-Iturbe B: Melatonin reduces renal interstitial
inflammation and improves hypertension in spontaneously
hypertensive rats. Am J Physiol Renal Physiol. 284:F447–F454. 2003.
View Article : Google Scholar
|
|
12
|
Wiesel P, Mazzolai L, Nussberger J and
Pedrazzini T: Two-kidney, one clip and one-kidney, one clip
hypertension in mice. Hypertension. 29:1025–1030. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Toora BD and Rajagopal G: Measurement of
creatinine by Jaffe's reaction-determination of concentration of
sodium hydroxide required for maximum color development in
standard, urine and protein free filtrate of serum. Indian J Exp
Biol. 40:352–354. 2002.
|
|
14
|
Lott JA, Stephan VA and Pritchard KA Jr:
Evaluation of the Coomassie Brilliant Blue G-250 method for urinary
protein. Clin Chem. 29:1946–1950. 1983.PubMed/NCBI
|
|
15
|
Chilkoti A, Tan PH and Stayton PS:
Site-directed mutagenesis studies of the high-affinity
streptavidin-biotin complex: Contributions of tryptophan residues
79, 108 and 120. Proc Natl Acad Sci U S A. 92:1754–1758. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Melnikov VY, Faubel S, Siegmund B, Lucia
MS, Ljubanovic D and Edelstein CL: Neutrophil-independent
mechanisms of caspase-1- and IL-18-mediated ischemic acute tubular
necrosis in mice. J Clin Invest. 110:1083–1091. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fulks M, Stout RL and Dolan VF: Urine
protein/creatinine ratio as a mortality risk predictor in
non-diabetics with normal renal function. J Insur Med. 43:76–83.
2012.PubMed/NCBI
|
|
18
|
Côté AM, Brown MA, Lam E, von Dadelszen P,
Firoz T, Liston RM and Magee LA: Diagnostic accuracy of urinary
spot protein: Creatinine ratio for proteinuria in hypertensive
pregnant women: Systematic review. BMJ. 336:1003–1006. 2008.
View Article : Google Scholar
|
|
19
|
Bakoush O, Grubb A, Rippe B and Tencer J:
Urine excretion of protein HC in proteinuric glomerular diseases
correlates to urine IgG but not to albuminuria. Kidney Int.
60:1904–1909. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ongajooth L, Ongajyooth S, Likidlilid A,
Chantachum Y, Shayakul C and Nilwarangkur S: Role of lipid
peroxidation, trace elements and anti-oxidant enzymes in chronic
renal disease patients. J Med Assoc Thai. 79:791–800.
1996.PubMed/NCBI
|
|
21
|
Negre-Salvayre A, Coatrieux C, Ingueneau C
and Salvayre R: Advanced lipid peroxidation end products in
oxidative damage to proteins. Potential role in diseases and
therapeutic prospects for the inhibitors. Br J Pharmacol. 153:6–20.
2008. View Article : Google Scholar
|
|
22
|
Alscher RG, Erturk N and Heath LS: Role of
superoxide dismutases (SODs) in controlling oxidative stress in
plants. J Exp Bot. 53:1331–1341. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kröncke KD, Fehsel K and Kolb-Bachofen V:
Inducible nitric oxide synthase in human diseases. Clin Exp
Immunol. 113:147–156. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
de Oliveira-Sales EB, Nishi EE, Boim MA,
Dolnikoff MS, Bergamaschi CT and Campos RR: Upregulation of AT1R
and iNOS in the rostral ventrolateral medulla (RVLM) is essential
for the sympathetic hyperactivity and hypertension in the 2K-1C
Wistar rat model. Am J Hypertens. 23:708–715. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tang Q and Hendricks RL: Interferon gamma
regulates platelet endothelial cell adhesion molecule 1 expression
and neutrophil infiltration into herpes simplex virus-infected
mouse corneas. J Exp Med. 184:1435–1447. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Motterlini R, Foresti R, Bassi R and Green
CJ: Curcumin, an antioxidant and anti-inflammatory agent, induces
heme oxygenase-1 and protects endothelial cells against oxidative
stress. Free Radic Biol Med. 28:1303–1312. 2000. View Article : Google Scholar : PubMed/NCBI
|