Many professional activities expose workers to
several biological agents representing a consistent risk factor for
the development of infective and non-infective pathologies. Among
these activities, including different professional areas such as
agriculture, breeding of livestock, food industry and
biotechnology, the most dangerous biohazard is the health-care
associated activity. Because of the intrinsic purpose of hospital
workplace, health care workers (HCWs) may be exposed to biological
agents. Accordingly, HCWs are frequently controlled and monitored
because of the high risk of biological contamination during their
activities (1). It was assessed
that the biological risk in workplaces is responsible for
>300,000 deaths per year worldwide underlining the importance of
the development of new monitoring strategies and approaches to
prevent the spread of contamination in indoor and closed
workplaces, such as hospitals (2).
One of the main sources of nosocomial biohazard
contamination are the bio-aerosols containing a plethora of
microorganisms, including endotoxins and molds, able to determine
infections in both patients and HCWs through their inhalation
(3,4). Another source of contamination,
especially for viral infections, may occur by direct exposure to
biological fluids, including blood, urine, semen and cerebral
spinal fluid (5). Unfortunately,
this contamination is often linked to percutaneous transmission
occurring after needle-stick injuries or cuts with other sharp
instruments (6).
HCWs can also be infected by several viruses. Many
of these may cause neoplastic transformation and are recognized as
‘carcinogenic to human (group 1) by the International Agency for
Research on Cancer (IARC)’. Among these, Epstein-Barr virus (EBV),
hepatitis B and C viruses (HBV and HCV), human T-cell lymphotropic
virus type 1 (HTLV-1), human herpes virus type 8 (HHV-8) and human
papillomavirus (HPV) are the most common viruses responsible for
cancer development after chronic infection (10–17).
The discovery of novel antiviral therapies, including that for HCV
infection (18), may reduce the
development of many cancer types. Based on the above, our research
group investigated the antiviral and antiproliferative effects of
novel compounds belonging to the class of C-nucleosides showing
encouraging results for the treatments of cancer, especially in the
context of viral infections (19).
Our previous studies described the frequency of HCV
infection among HCWs and a case of non-Hodgkin lymphoma was
diagnosed during the survey (20,21).
According to this observation, in the present review, HCV infection
among HCWs is analyzed taking into account the association with
lymphoma development.
Several studies show that a correct knowledge and
training of health-care workers significantly reduces the risk of
accidental exposure to biological agents. Notably, the frequency of
accidental exposure to biohazard agents increases among workers
with less working seniority, such as nursing students or trainees,
compared to the older workers (22–24).
Conversely, other studies showed that workers with >15 years
professional experience had an incidence rate for accidental
contamination three times higher than workers with a work
experience ≤5 years (25). These
data may be due to a more prolonged exposure to biological risk in
workers with higher work experience and not to the inexperience of
the workers (26–28).
The most common mode of transmission of HBV and HCV,
during health-care work activities, is due to percutaneous exposure
and sharp injuries (29–31). Of note, many HCV infected patients
do not show severe clinical manifestations and do not reveal their
infection status to HCWs. Accordingly, the accidental contact with
the infected material was previously very common. In fact, the
World Health Organization (WHO) stated that in the European area
only the percutaneous exposure risk of HBV and HCV infections in
the health-care workers is >450,000 cases of which 340,000 for
HBV virus and 149,000 for HCV (31–33).
According to the current regulation, caution by all HCWs have to be
applied with the patients with and without any diagnosed
infections.
Our research group conducted a 10-year observational
study to determine the frequency of HCV infection among HCWs from a
single institution. This study included a case series of 403
workers employed in various clinical areas. This study showed that
the high prevalence of HCV infection was found in nurses (3%) and
physicians/surgeons (5%) in comparison to the other health-care
worker categories. An important result of the study was that in the
10-year survey there were no new infections by HCV in the monitored
workers. This result stresses the concept that the correct handling
procedures of hazardous biological materials and the use of
personal protective equipment lead to a reduction or a total
avoidance of the risk of infection due to biohazard materials
(20,34). Therefore, these data are in
agreement with previous studies demonstrating that the education of
workers employed in hospitals or laboratories on the prevention of
needle-stick accidents or sharp injuries is able to decrease
needle-stick injuries (35–37).
The cross contamination occurred between infected patients and
health-care workers and vice versa could be avoided wearing
protective barriers (gloves and lab coat), washing hands frequently
and taking care in using biological materials, needles or sharp
objects. The use of written protocols and standard procedures is
certainly a good strategy that allows to minimize the risk of
accidental infection caused by HCV and other hazardous biological
agents with which workers may come into contact in hospitals
(38,39).
In our experience, the above mentioned 10-year
study, revealed that one of the HCV-infected HCWs, with a chronic
infection history of 25 years, developed a mucosa-associated
lymphoid tissue lymphoma (MALT) of the liver (20). Molecular analyses of tumor tissue
indicated that immunoglobulin gene combinations were those usually
detected among HCV-associated lymphomas (11). Furthermore, the discovery of MALT
lymphoma with the concomitant HCV infection prompted us to extend
the investigation to a larger cohort of HCWs. Thus, a tailored
health surveillance program to 3,138 health-care workers employed
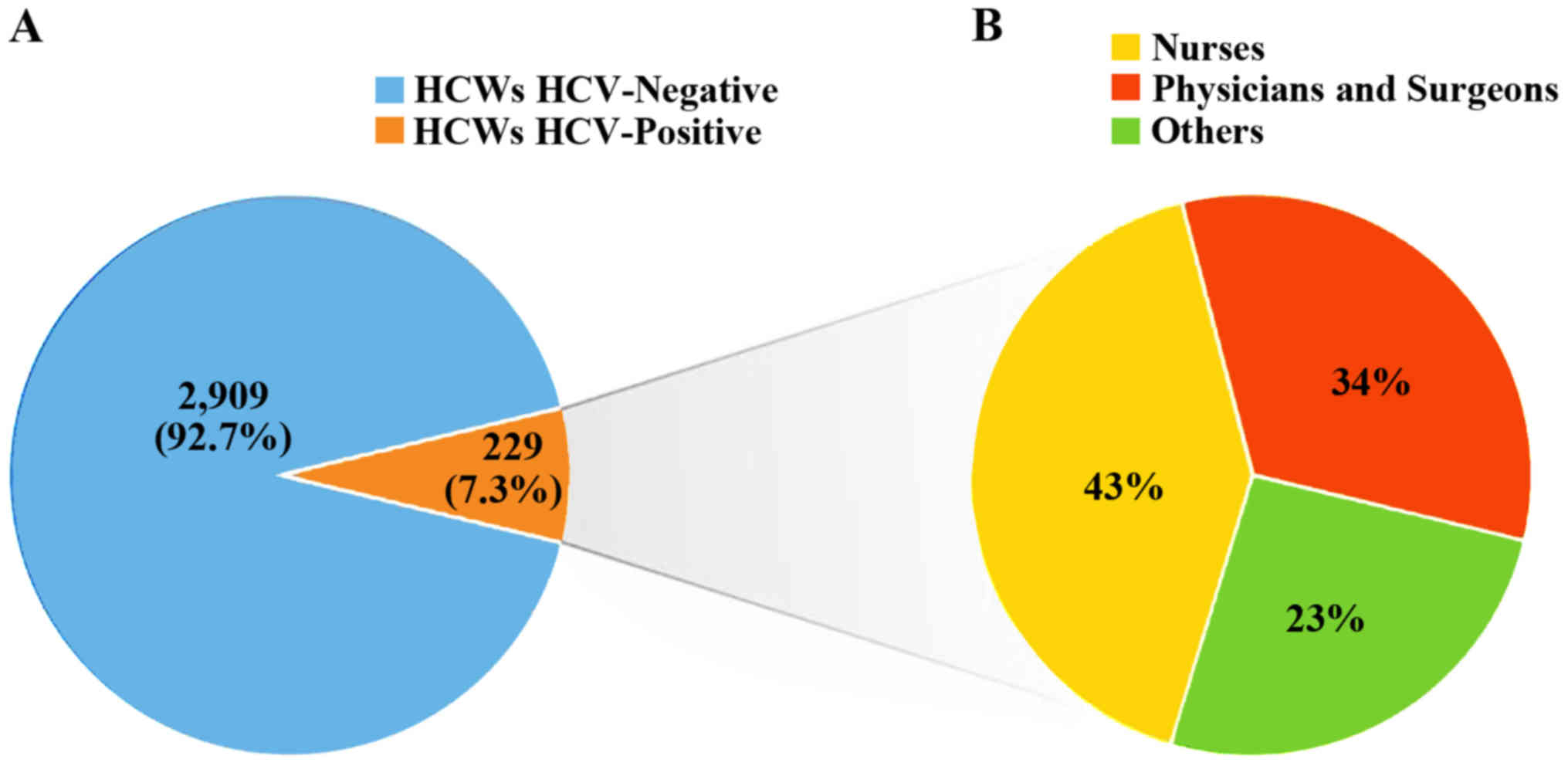
in four Italian medical institutions was applied (21). Of these, 1,352 (43%) were nurses,
953 (30%) were physicians and surgeons and 833 (27%) were other
employees working in medical institutions. All the workers were
screened for HCV infection by anti-HCV antibodies. HCV infection
was detected in 229 out of 3,138 HCWs (7.3%). Of the HCV-infected
HCWs, 43% were nurses, 34% physician and surgeons and 23% were
other employees (Fig. 1).
Intriguingly, a case of gastric Malt lymphoma was observed among
those with HCV infection (21). As
revealed in the previous independent survey of HCWs by Marconi
et al, 2010, the molecular analyses performed in such Malt
tumor tissue supported the notion that HCV infection was associated
with the malignant transformation (20).
Health-care professionals are a working category
particularly exposed to biological risk factors during the normal
working activities. These workers are daily subjected to
occupational biological exposure in handling blood-borne samples or
other biological fluids. One of the main sources of accidental
contamination is represented by percutaneous and mucocutaneous
infections (24). Microorganisms
contained in aerosols, aerial dissemination caused by ventilation
systems and direct infection with affected patients represent other
ways of contamination (50). The
application of the standard precautions during work activities is
the most important reason in reducing the risk of blood-borne
pathogen transmission that in turn may result in reduction of
infection-related cancers.
|
1
|
Messineo A and Marsella LT: Biological
hazards and healthcare-associated infections in Italian healthcare
facilities: Some considerations on inspections and accountability.
Ann Ig. 27:799–807. 2015.PubMed/NCBI
|
|
2
|
Corrao CR, Mazzotta A, La Torre G and De
Giusti M: Biological risk and occupational health. Ind Health.
50:326–337. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Srikanth P, Sudharsanam S and Steinberg R:
Bio-aerosols in indoor environment: Composition, health effects and
analysis. Indian J Med Microbiol. 26:302–312. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Heimbuch BK, Wallace WH, Balzli CL, Laning
ML, Harnish DA and Wander JD: Bioaerosol exposure to personnel in a
clinical environment absent patients. J Occup Environ Hyg.
13:D11–D15. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tarantola A, Abiteboul D and Rachline A:
Infection risks following accidental exposure to blood or body
fluids in health care workers: A review of pathogens transmitted in
published cases. Am J Infect Control. 34:367–375. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Castella A, Vallino A, Argentero PA and
Zotti CM: Preventability of percutaneous injuries in healthcare
workers: A year-long survey in Italy. J Hosp Infect. 55:290–294.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pierce GE: Pseudomonas aeruginosa,
Candida albicans, and device-related nosocomial infections:
Implications, trends, and potential approaches for control. J Ind
Microbiol Biotechnol. 32:309–318. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Beggs CB, Kerr KG, Noakes CJ, Hathway EA
and Sleigh PA: The ventilation of multiple-bed hospital wards:
Review and analysis. Am J Infect Control. 36:250–259. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Furneri PM, Garozzo A, Musumarra MP,
Scuderi AC, Russo A and Bonfiglio G: Effects on adhesiveness and
hydrophobicity of sub-inhibitory concentrations of netilmicin. Int
J Antimicrob Agents. 22:164–167. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shinozaki-Ushiku A, Kunita A and Fukayama
M: Update on Epstein-Barr virus and gastric cancer (Review). Int J
Oncol. 46:1421–1434. 2015.PubMed/NCBI
|
|
11
|
Libra M, Gloghini A, De Re V, Rupolo M,
Navolanic PM, Gasparotto D, Stivala F, Spina M, Boiocchi M and
Carbone A: Aggressive forms of non-Hodgkins lymphoma in two
patients bearing coinfection of Epstein-Barr and hepatitis C
viruses. Int J Oncol. 26:945–950. 2005.PubMed/NCBI
|
|
12
|
Gloghini A, Gaidano G, Larocca LM,
Pierconti F, Cingolani A, Dal Maso L, Capello D, Franceschi S,
Tirelli U, Libra M, et al: Expression of cyclin-dependent kinase
inhibitor p27Kip1 in AIDS-related diffuse large-cell
lymphomas is associated with Epstein-Barr virus-encoded latent
membrane protein 1. Am J Pathol. 161:163–171. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Arzumanyan A, Reis HM and Feitelson MA:
Pathogenic mechanisms in HBV- and HCV-associated hepatocellular
carcinoma. Nat Rev Cancer. 13:123–135. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
De Re V, Caggiari L, De Zorzi M, Repetto
O, Zignego AL, Izzo F, Tornesello ML, Buonaguro FM, Mangia A,
Sansonno D, et al: Genetic diversity of the KIR/HLA system and
susceptibility to hepatitis C virus-related diseases. PLoS One.
10:e01174202015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Beral V, Peterman T, Berkelman R and Jaffe
H: AIDS-associated non-Hodgkin lymphoma. Lancet. 337:805–809. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Libra M, Scalisi A, Vella N, Clementi S,
Sorio R, Stivala F, Spandidos DA and Mazzarino C: Uterine cervical
carcinoma: Role of matrix metalloproteinases (Review). Int J Oncol.
34:897–903. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Petry KU: HPV and cervical cancer. Scand J
Clin Lab Invest Suppl. 244:59–62. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ewers EC, Shah PA, Carmichael MG and
Ferguson TM: Concurrent systemic chemoimmunotherapy and
sofosbuvir-based antiviral treatment in a hepatitis C
virus-infected patient with diffuse large B-cell lymphoma. Open
Forum Infect Dis. 3:ofw2232016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Giofrè SV, Romeo R, Carnovale C, Mancuso
R, Cirmi S, Navarra M, Garozzo A and Chiacchio MA: Synthesis and
biological properties of
5-(1H-1,2,3-triazol-4-yl)isoxazolidines: A new class of
C-nucleosides. Molecules. 20:5260–5275. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Marconi A, Candido S, Talamini R, Libra M,
Nicoletti F, Spandidos DA, Stivala F and Proietti L: Prevalence of
hepatitis C virus infection among health-care workers: A 10-year
survey. Mol Med Rep. 3:561–564. 2010.PubMed/NCBI
|
|
21
|
Rapisarda V, Marconi A, Candido S,
Nicolosi D, Salmeri M, Gangemi P, Proietti L, Spandidos DA, Bracci
M, Fenga C, et al: A tailored health surveillance program unveils a
case of MALT lymphoma in an HCV-positive health-care worker. Oncol
Lett. 5:651–654. 2013.PubMed/NCBI
|
|
22
|
Maniar HH, Tawari AA, Suk M, Bowen TR and
Horwitz DS: Percutaneous and mucocutaneous exposure among
orthopaedic surgeons: Immediate management and compliance with CDC
protocol. J Orthop Trauma. 29:e391–e394. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mohammadi N, Allami A and Mohamadi Malek
R: Percutaneous exposure incidents in nurses: Knowledge, practice
and exposure to hepatitis B infection: Percutaneous exposure
incidents in nurses. Hepat Mon. 11:186–190. 2011.PubMed/NCBI
|
|
24
|
Petrucci C, Alvaro R, Cicolini G, Cerone
MP and Lancia L: Percutaneous and mucocutaneous exposures in
nursing students: An Italian observational study. J Nurs Scholarsh.
41:337–343. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kosgeroglu N, Ayranci U, Vardareli E and
Dincer S: Occupational exposure to hepatitis infection among
Turkish nurses: Frequency of needle exposure, sharps injuries and
vaccination. Epidemiol Infect. 132:27–33. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Alese OO, Alese MO, Ohunakin A and Oluyide
PO: Seroprevalence of hepatitis B surface antigen and occupational
risk factors among health care workers in Ekiti State, Nigeria. J
Clin Diagn Res. 10:LC16–LC18. 2016.PubMed/NCBI
|
|
27
|
Chiarakul S, Eunumjitkul K, Vuttiopas S,
Vorapimol AR, Kaewkungwal J and Poovorawan Y: Seroprevalence and
risk factors of hepatitis B virus infection among health care
workers at the Institute of Neurology. J Med Assoc Thai.
90:1536–1545. 2007.PubMed/NCBI
|
|
28
|
Ciorlia LA and Zanetta DM: Hepatitis B in
healthcare workers: Prevalence, vaccination and relation to
occupational factors. Braz J Infect Dis. 9:384–389. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mischke C, Verbeek JH, Saarto A, Lavoie
MC, Pahwa M and Ijaz S: Gloves, extra gloves or special types of
gloves for preventing percutaneous exposure injuries in healthcare
personnel. Cochrane Database Syst Rev. 3:CD0095732014.
|
|
30
|
Mbaisi EM, Nganga Z, Wanzala P and Omolo
J: Prevalence and factors associated with percutaneous injuries and
splash exposures among health-care workers in a provincial
hospital, Kenya, 2010. Pan Afr Med J. 14:102013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Prüss-Ustün A, Rapiti E and Hutin Y:
Estimation of the global burden of disease attributable to
contaminated sharps injuries among health-care workers. Am J Ind
Med. 48:482–490. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Westermann C, Peters C, Lisiak B, Lamberti
M and Nienhaus A: The prevalence of hepatitis C among healthcare
workers: A systematic review and meta-analysis. Occup Environ Med.
72:880–888. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Prüss-Ustün A, Rapiti E and Hutin Y: Sharp
injuries: Global burden of disease from sharp injuries to
health-care workersEnvironmental Burden of Disease Series. No. 3.
Prüss-Üstün A, Campbell-Lendrum D, Corvalán C and Woodward A: World
Health Organisation; Geneva: 2003
|
|
34
|
Proietti L, Malaponte G, Libra M,
Navolanic PM, Bevelacqua Y, Travali S and Mazzarino MC: Analysis of
hepatitis C virus infection among health-care workers: An
observational study. Minerva Gastroenterol Dietol. 51:255–259.
2005.PubMed/NCBI
|
|
35
|
Haiduven DJ, Phillips ES, Clemons KV and
Stevens DA: Percutaneous injury analysis: Consistent
categorization, effective reduction methods, and future strategies.
Infect Control Hosp Epidemiol. 16:582–589. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Tarigan LH, Cifuentes M, Quinn M and
Kriebel D: Prevention of needle-stick injuries in healthcare
facilities: A meta-analysis. Infect Control Hosp Epidemiol.
36:823–829. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
De Carli G, Abiteboul D and Puro V: The
importance of implementing safe sharps practices in the laboratory
setting in Europe. Biochem Med (Zagreb). 24:45–56. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Davanzo E, Frasson C, Morandin M and
Trevisan A: Occupational blood and body fluid exposure of
university health care workers. Am J Infect Control. 36:753–756.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
van Gemert-Pijnen J, Hendrix MG, Van der
Palen J and Schellens PJ: Effectiveness of protocols for preventing
occupational exposure to blood and body fluids in Dutch hospitals.
J Hosp Infect. 62:166–173. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Denniston MM, Jiles RB, Drobeniuc J,
Klevens RM, Ward JW, McQuillan GM and Holmberg SD: Chronic
hepatitis C virus infection in the United States, National Health
and Nutrition Examination Survey 2003 to 2010. Ann Intern Med.
160:293–300. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
41
|
Bartosch B, Thimme R, Blum HE and Zoulim
F: Hepatitis C virus-induced hepatocarcinogenesis. J Hepatol.
51:810–820. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Taborelli M, Polesel J, Montella M, Libra
M, Tedeschi R, Battiston M, Spina M, Di Raimondo F, Pinto A, Crispo
A, et al: Hepatitis B and C viruses and risk of non-Hodgkin
lymphoma: A case-control study in Italy. Infect Agent Cancer.
11:272016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Cacoub P, Commarmond C, Sadoun D and
Desbois AC: Hepatitis C virus infection and rheumatic diseases: The
impact of direct-acting antiviral agents. Rheum Dis Clin North Am.
43:123–132. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Cacoub P, Comarmond C, Domont F, Savey L,
Desbois AC and Saadoun D: Extrahepatic manifestations of chronic
hepatitis C virus infection. Ther Adv Infect Dis. 3:3–14. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Terrier B and Cacoub P: Renal involvement
in HCV-related vasculitis. Clin Res Hepatol Gastroenterol.
37:334–339. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Aslam F, Alam M and Lakkis NM: Hepatitis C
and carotid atherosclerosis: A retrospective analysis.
Atherosclerosis. 209:340–343. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Libra M, Polesel J, Russo AE, De Re V,
Cinà D, Serraino D, Nicoletti F, Spandidos DA, Stivala F and
Talamini R: Extrahepatic disorders of HCV infection: A distinct
entity of B-cell neoplasia? Int J Oncol. 36:1331–1340. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Libra M, Gloghini A, Malaponte G, Gangemi
P, De Re V, Cacopardo B, Spandidos DA, Nicoletti F, Stivala F,
Zignego AL, et al: Association of t(14;18) translocation with HCV
infection in gastrointestinal MALT lymphomas. J Hepatol.
49:170–174. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Libra M, Gasparotto D, Gloghini A,
Navolanic PM, De Re V and Carbone A: Hepatitis C virus (HCV) I
hepatitis C virus (HCV) infection and lymphoproliferative
disorders. Front Biosci. 10:2460–2471. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Beggs C, Knibbs LD, Johnson GR and
Morawska L: Environmental contamination and hospital-acquired
infection: Factors that are easily overlooked. Indoor Air.
25:462–474. 2015. View Article : Google Scholar : PubMed/NCBI
|