Introduction
Asthma is one of the most common chronic respiratory
diseases, characterized by variable airflow obstruction, airway
inflammation and remodeling, bronchial hyperresponsiveness and
mucus hypersecretion, excessive infiltration of leukocytes
(particularly eosinophils) into the airways, and intrapulmonary
overexpression of Th2 cytokines, including interleukin (IL)-4, IL-5
and IL-13 (1,2). Increasing evidence has indicated that
the incidence of asthma has markedly increased worldwide, and its
morbidity and mortality rates have increased in previous decades,
despite advances in understanding its pathophysiological mechanism
(3,4). In addition, although asthma treatment
has improved by the implementation of management guidelines, and
the use of inhaled corticosteroids and β-2 agonists as the first
line treatment for asthmatics (5),
current treatments and the well-known side effects of
corticosteroids are not always satisfactory in clinical practice
(6). Therefore, novel or
alternative approaches for the treatment of asthma are potentially
useful and increasingly critical.
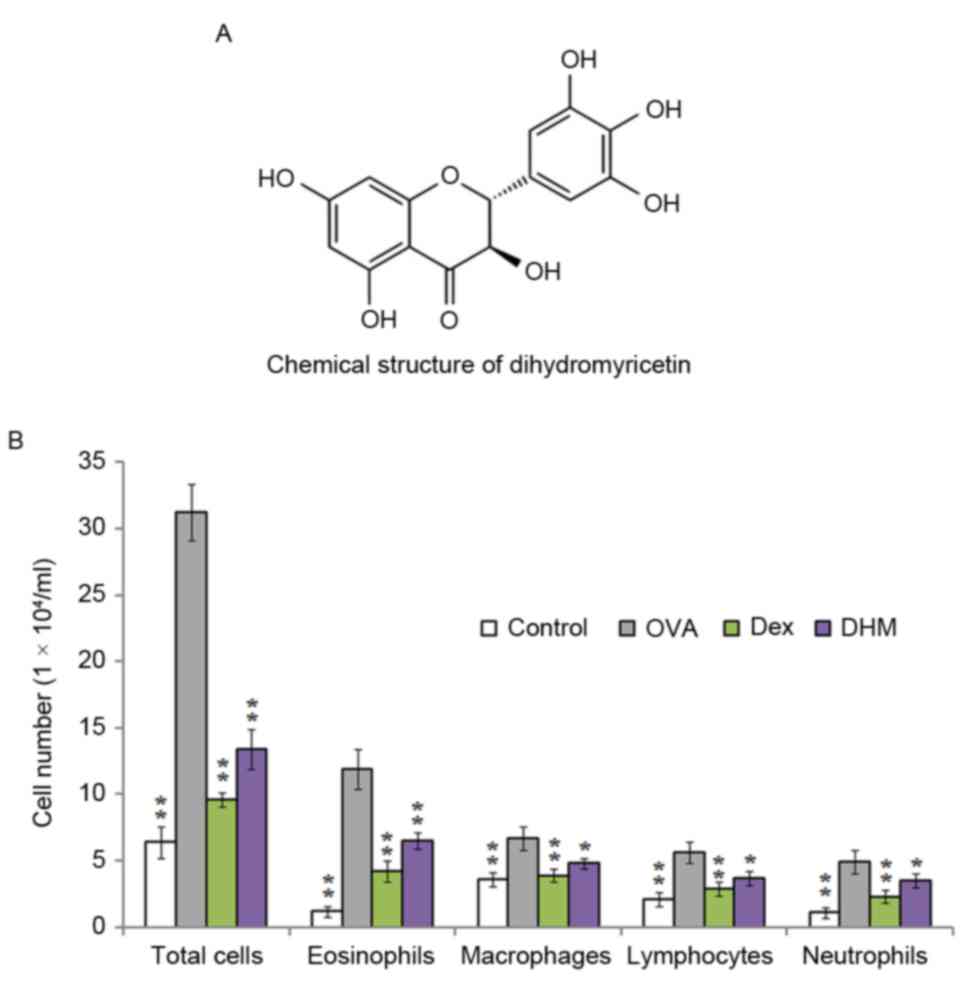
Dihydromyricetin (DHM) is a plant flavonoid
component isolated from the tender stem and leaves of Ampelopsis
grossedentata, which is widely used in traditional Chinese
medicine in South China for preventing and treating hepatitis,
chronic nephritis, vomiting, acid regurgitation, polyorexia and
halitosis (7,8). The chemical structure of DHM is shown
in Fig. 1A, which is similar to
that of myrecetin, a natural flavonoid found in berries, grapes,
vegetables, herbs, fruits and other plants with anticancer
activities (9,10). Previous studies have indicated that
DHM exhibits a range of biological and pharmacological activities,
including hepatic protection (11,12),
attenuation of cardiomyocyte hypertrophy (13), antimicrobial activity,
anti-oxidation and antitumor effects (14–17).
In previous years, the anti-inflammatory effect of
DHM has attracted increased interest. DHM supplementation has been
found to exert anti-inflammatory activity in patients with
nonalcoholic fatty liver disease through decreased levels of serum
tumor necrosis factor-α, cytokeratin-18 and fibroblast growth
factor 21 (18). Additionally,
studies have suggested that DHM possesses anti-inflammatory effects
via inhibiting the activity of nuclear factor κB (NF-κB) and
mitogen-activated protein kinase (MAPK) signaling pathways
(19,20). However, no information is currently
available on the effect of DHM treatment on a non-infectious mouse
airway inflammatory model. Therefore, in the present study, an
ovalbumin (OVA) -induced asthmatic model was used to evaluate
whether DHM has a distinct anti-inflammatory role in asthmatic
mice.
Materials and methods
Preparation of DHM
DHM was purchased from Sigma- Aldrich; Merck KGaA
(Darmstadt, Germany), dissolved in ethanol and prepared as a 10
mg/ml stock solution, which was diluted to the final concentration
with sterile phosphate-buffered saline (PBS; pH 7.4) immediately
prior to use.
Animals
Female C57BL/6 mice (4–6 weeks old) were purchased
from Beijing Biocytogen Company (Beijing, China), and maintained in
a pathogen-free animal room at a constant temperature (25°C) in
12:12-h light:dark cycle with access to water and standard chow
ad libitum. The guidelines of the Animal Care and Use
Committee (ACUC) of Nanjing Chest Hospital (Nanjing, China) were
adhered to in strict accordance, and the experimental procedures
were reviewed and approved by the ACUC.
Sensitization and treatment
protocols
The mice were divided into four groups, each
containing eight mice: Negative control group; OVA group,
OVA+dexamethasone (Dex; Sigma-Aldrich; Merck KGaA) group; and
OVA+DHM group. The induction of asthma in the mice treated with OVA
(grade Ш) was performed as described previously (21). Briefly, each mouse was sensitized
with 20 µg of OVA in 1 mg aluminum hydroxide by intraperitoneal
injection on days 0, 7 and 14. On days 21–27, the OVA-challenged
mice were exposed to inhalation with 5% OVA solution, which was
aerosolized using an ultrasonic nebulizer for 1 h per day. The mice
in the negative control groups were sensitized and challenged with
an equal volume of PBS, instead of the OVA and drug treatment. The
other three groups of asthma-induced mice were administered
intraperitoneally with 10 mg/kg of DHM, based on preliminary
experiments and a previous study (6), or 2 mg/kg of OVA as a positive
control between days 14 and 27.
Collection of bronchoalveolar lavage
(BAL) fluid
Following the final challenge, the mice were
sacrificed and the thoracic cavity was immediately opened by
careful dissection. The trachea was then exposed, and BAL fluid was
collected by lavage of the lung through the trachea infused with
three aliquots of PBS (0.3, 0.3 and 0.4 ml) in a total volume of 1
ml. The fluids were then centrifuged at 400 × g for 5 min at
4°C, and the pellets were recovered for cellular analysis. The
supernatants were stored at −80°C until biochemical analyses.
Counts of inflammatory cells in BAL
fluid
The cell pellets were resuspended in 500 µl of PBS,
and the total number of viable cells were counted using a
hemocytometer through Trypan blue exclusion. Cytological
examination was performed as described previously (22). Briefly, cytospin preparations were
produced using a Cytospin (Thermo Fisher Scientific, Inc., Waltham,
MA, USA) and stained with modified Wright's stain. Differential
cell counting was performed on at least 200 cells in each slide
using standard morphological criteria under a light microscope
(CX41; Olympus Corporation, Tokyo, Japan).
ELISA
The expression levels of OVA-specific IgE and IgG1
in the mouse sera and cytokines in the BAL fluid were measured
using the ELISA method, according to a previously described method
(2) with modifications. Briefly,
blood samples were immediately collected from murine orbita
following sacrifice of the mice on day 28, followed by
centrifugation at 1,000 × g for 15 min at 4°C. Aliquots of
the serum were then stored at −80°C until analysis. For
OVA-specific IgE and IgG1 analysis, microplate wells were
respectively coated with purified rat anti-mouse IgE (ab99574;
1:300; Abcam, Cambridge, UK) and IgG1 (ab99656; 1:300; Abcam),
followed by incubation with blocking buffer at room temperature for
1 h and subsequent washing with PBS. Subsequently, mouse sera were
added to the microplate wells and incubated for 2 h at room
temperature, followed by incubation with biotin-labeled anti-mouse
IgE or IgG1 for 1 h at room temperature. The reactions were read
using an automated spectrophotometric plate reader (PerkinElmer,
Inc., Waltham, MA, USA) at 450 nm. The levels of IL-4, IL-5 and
IL-13 in the BAL fluid were also determined using corresponding
specific ELISA kits (BD Biosciences, Franklin Lakes, NJ, USA).
Lung tissue histopathology
Following collection of BAL fluid, lung tissues were
excised from the mice and fixed in 10% (v/v) formalin overnight.
The tissue was then embedded in paraffin and cut into sections of 5
µm thickness, followed by deparaffinization and rehydration. The
sections were then stained with hematoxylin and eosin (H&E) for
detecting the infiltration of inflammatory cells, and stained with
periodic acid-Schiff (PAS) staining to measure mucus production
under a light microscope (CX41; Olympus Corporation).
Measurement of airway
hyperresponsiveness (AHR)
AHR was measured as described previously (23). Briefly, 24 h following the final
OVA challenge, conscious and unrestrained mice were used to
evaluate AHR using whole-body plethysmography (Buxco Electronics,
Inc., Wilmington, NC, USA). Each mouse was placed in a single
chamber and subjected to exposure of aerosolized PBS, followed by
5, 10, 20 and 40 mg/ml solutions of aerosolized methacholine in PBS
for 3 min each time (n=4), and the interval duration between each
exposure was 30 min. Following each exposure of methacholine at
different concentrations, bronchoconstriction was recorded using
whole-body plethysmography. The results were calculated as the
proportion of the respective basal Penh values obtained from the
PBS-challenged control mice.
Statistical analysis
Data are expressed as the mean ± standard deviation.
Statistical analysis was performed using the SPSS statistical
software package (version 11.0; SPSS, Inc., Chicago, IL, USA) using
Student's two-tail t-test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Effect of DHM on the infiltration of
inflammatory cells in BAL fluid
Alterations in cellular components, particularly
eosinophils, are critical in the development of asthma. To evaluate
the anti-inflammatory effects of DHM, inflammatory cells, including
eosinophils, macrophages, lymphocytes and neutrophils, in the BAL
fluid of mice challenged with OVA were stained with Wright's stain
and counted. The results demonstrated that OVA challenge resulted
in an apparent increased influx of eosinophils, macrophages,
lymphocytes and neutrophils into the BAL fluid of the
OVA-sensitized mice. However, DHM challenge significantly reduced
the number of these inflammatory cells in the BAL fluid, compared
with OVA-challenged mice (Fig.
1B).
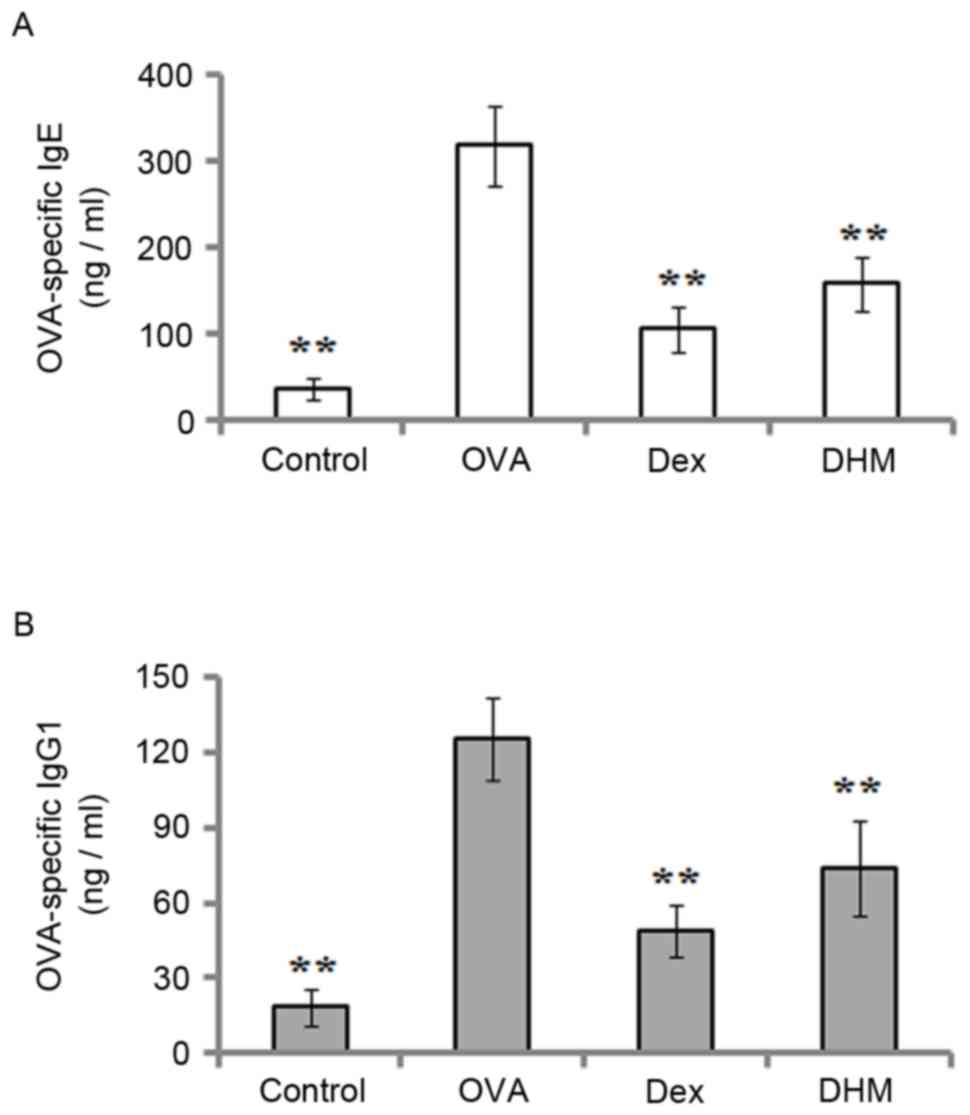
Effect of DHM on the release of
OVA-specific IgE and IgG1 into serum
In the pathogenesis of the allergic response, IgE
and IgG1 are associated with inflammatory cells. Therefore, the
levels of OVA-specific IgE and IgG1 in the serum were determined
using ELISA. As shown in Fig. 2,
the results demonstrated that the levels of IgE (Fig. 2A) and IgG1 (Fig. 2B) in the serum were markedly
increased in the OVA-treated mice, compared with the control mice.
However, DHM treatment significantly decreased the OVA-specific
levels of IgE and IgG1, compared with the OVA-challenged group.
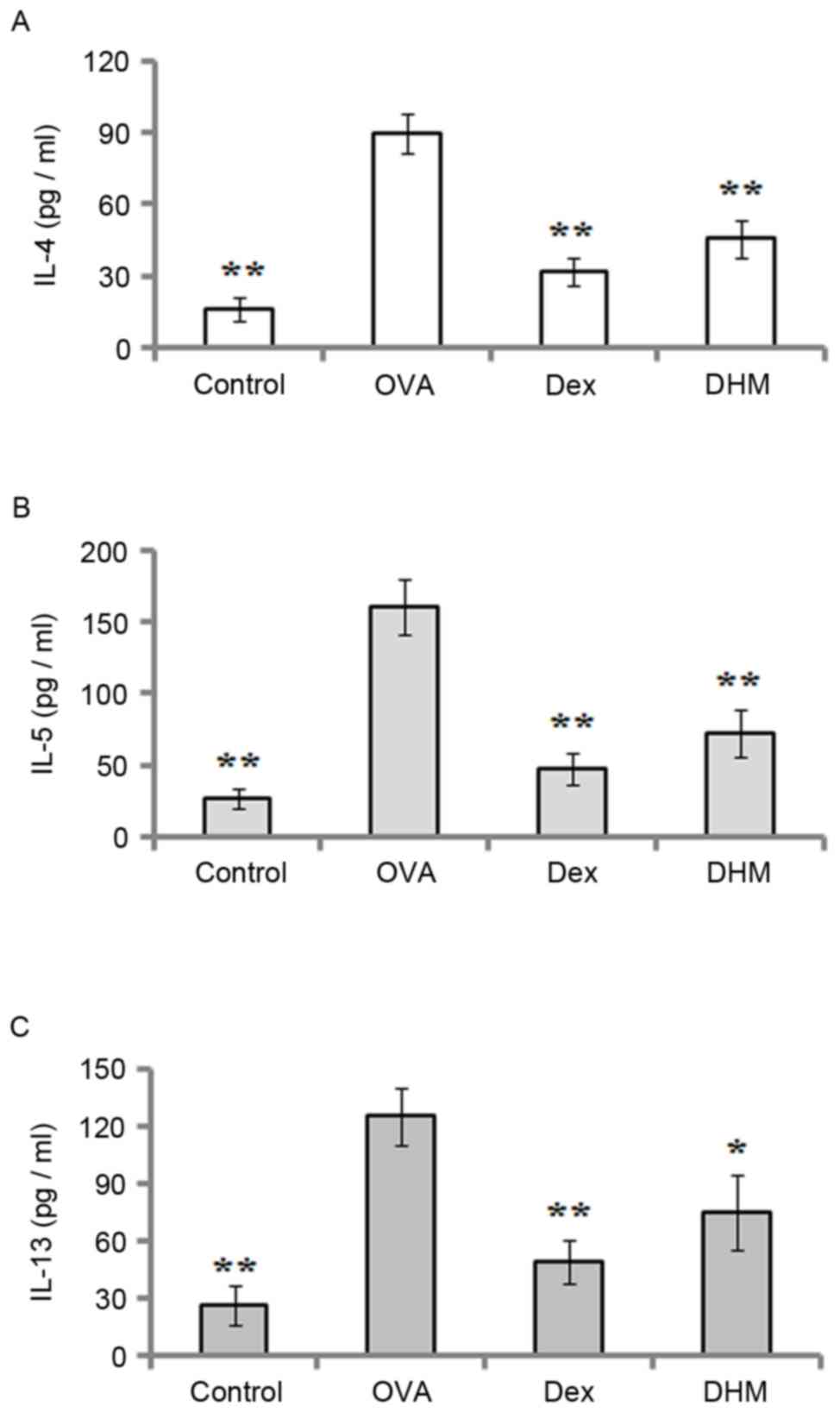
Effect of DHM on cytokine levels
To determine the effect of DHM on the release of
cytokines in OVA-challenged mice, the levels of IL-4, IL-5 and
IL-13 in the BAL fluid were measured using ELISA 24 h following the
final challenge. As shown in Fig.
3, the results demonstrated that OVA sensitization and
challenge resulted in marked elevations in the production of IL-4,
IL-5 and IL-13 in the BAL fluid of the mice, however, these
elevated levels of IL-4 (Fig. 3A),
IL-5 (Fig. 3B) and IL-13 (Fig. 3C) were significantly downregulated
by treatment with DHM and the positive control, Dex.
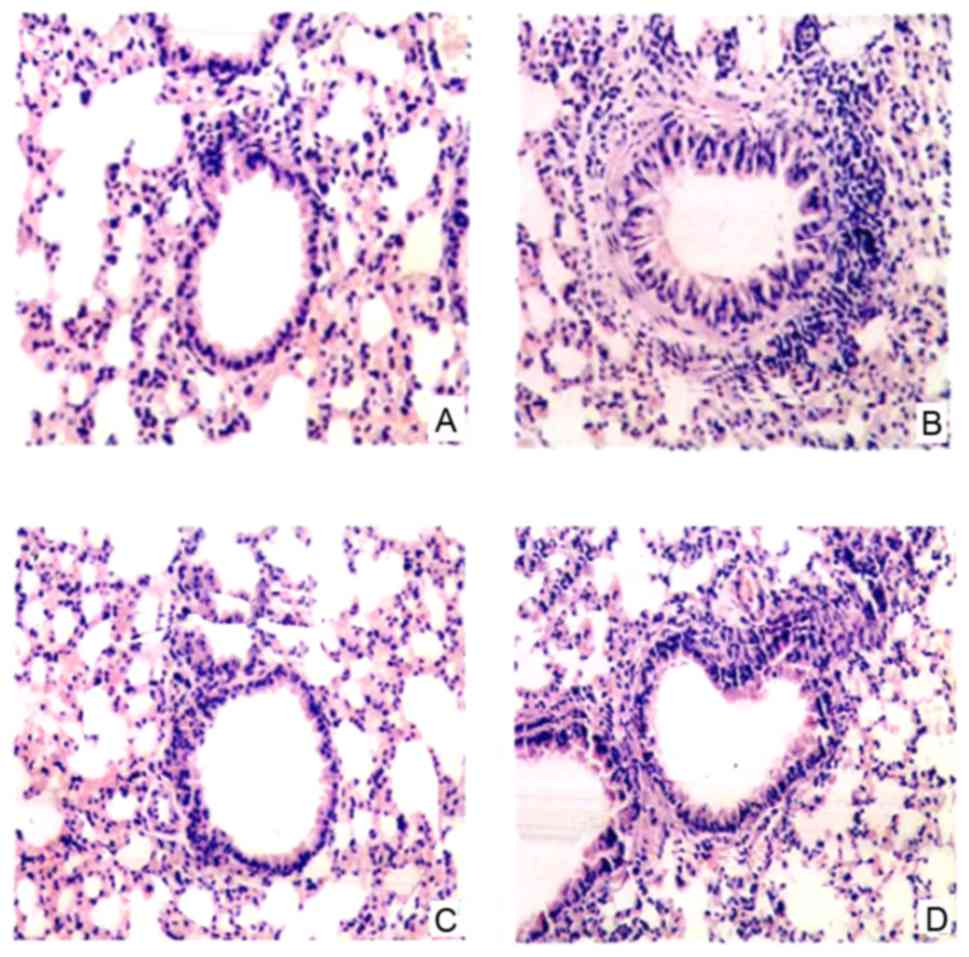
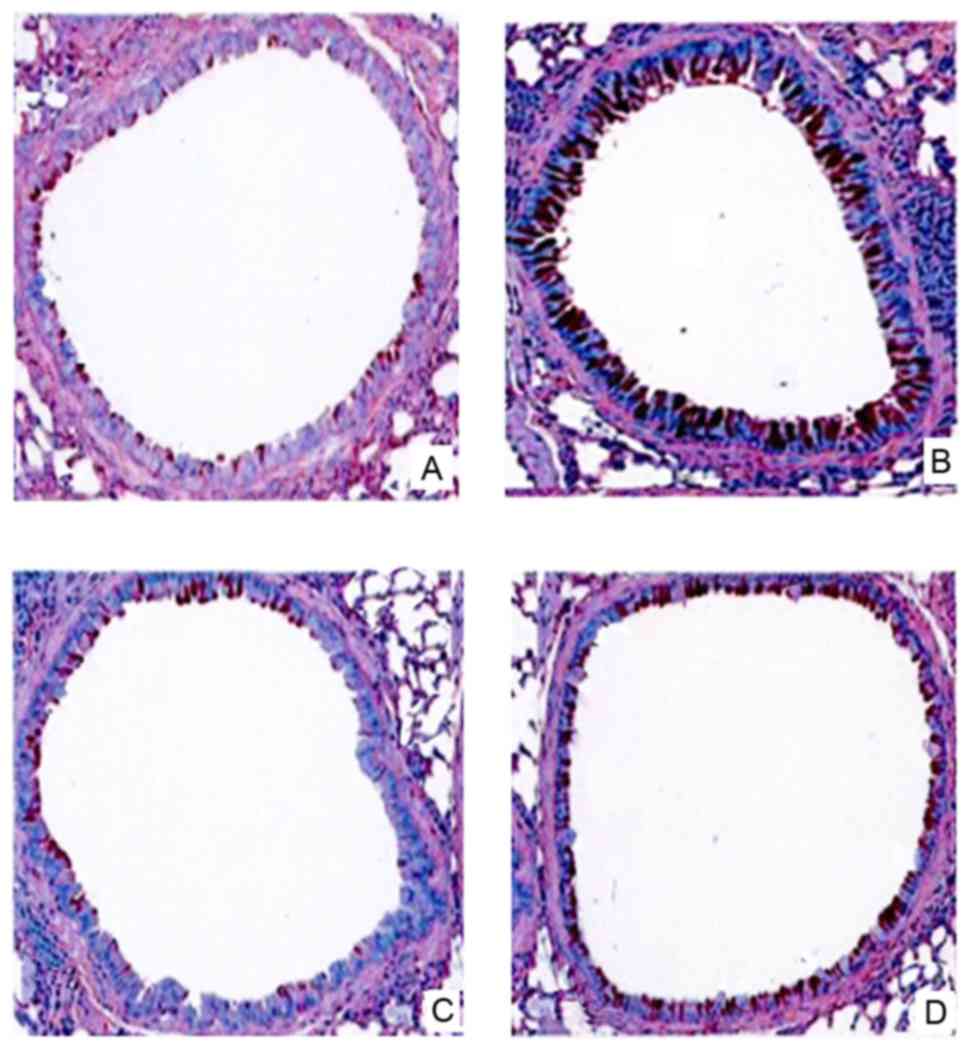
Effect of DHM on OVA-induced
inflammatory cells in lung tissue
To evaluate the anti-inflammatory effect of DHM,
asthmatic lung tissue was collected from the mice 24 h following
the final OVA challenge, and stained with H&E solution. The
results showed that no inflammatory cell infiltration was observed
in the normal lung tissue of the control mice (Fig. 4A). By contrast, in the
OVA-challenged mice, the infiltration of inflammatory cells, which
were predominantly eosinophils, were found in the peribronchial and
perivascular areas of the lung tissue (Fig. 4B). However, DHM treatment and
positive control (Dex) treatment effectively inhibited the
infiltration of inflammatory cells into the lung tissues of the
OVA-challenged mice (Fig.
4C-D).
Effect of DHM on airway goblet cell
hyperplasia and mucus production
To evaluate the effect of DHM on mucus
overproduction caused by goblet cell hyperplasia, lung tissue
sections were stained with PAS staining. As shown in Fig. 5, the results demonstrated that
mucus hypersecretion and goblet cell hyperplasia were observed in
the bronchi of the airways in the OVA-challenged mice, but not in
the control mice (Fig. 5A and B).
However, mucus production and the number of goblet cells were
markedly decreased in the Dex-treated (Fig. 5C) and DHM-treated (Fig. 5D) asthmatic mice.
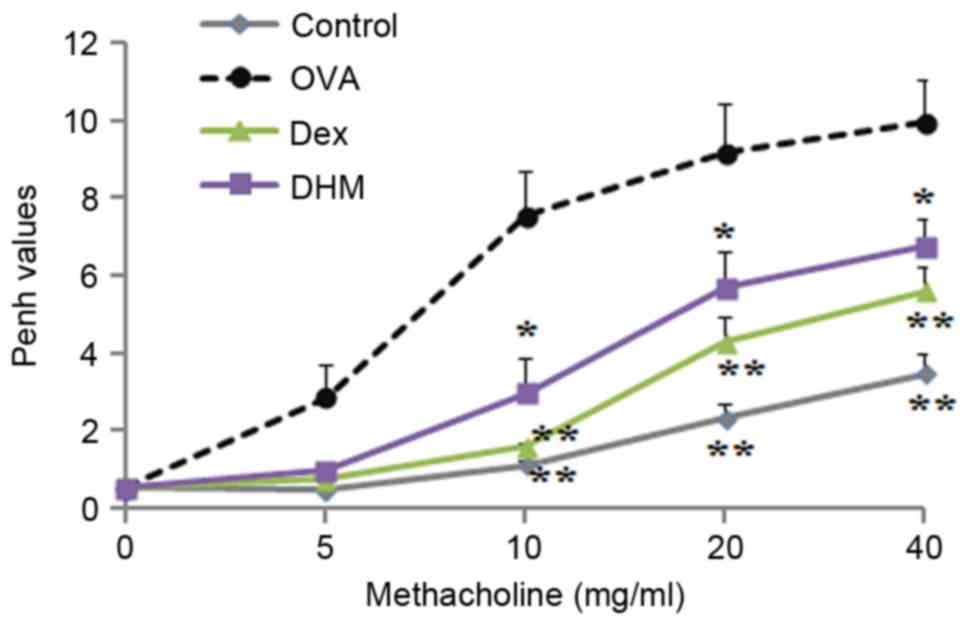
Effect of DHM on AHR
To determine the inhibitory effect of DHM on AHR,
the OVA-challenged mouse model, in which methacholine served as an
AHR promoter, was used. AHR was calculated by Penh values (enhanced
pauses). The results showed that, in the OVA-challenged mice, the
Penh value was higher, compared with that of control group when the
concentration of methacholine increased between 5 and 40 mg/ml.
Treatment with the positive control (Dex) or DHM significantly
decreased the Penh value, compared with that in the OVA-challenged
group at a methacholine concentration range of 10–40 mg/ml
(Fig. 6).
Discussion
Asthma is one of the most common inflammatory
diseases of the airways, characterized by increased infiltration of
various inflammatory cells into the lung airways, bronchial
hyperresponsiveness, reversible airway obstruction and reduced
respiratory function (24). Due to
the prevalence of asthma worldwide and the various side effects
resulting from the long-term use of corticosteroids and β-2
agonists, it is necessary to investigate effective therapeutic
agents for the treatment of asthma. DHM is a major bioactive
flavonoid, originally isolated from the medical herb, Ampelopsis
grossedentata, which has been found to possess various
pharmacological activities (8).
However, the effect of DHM treatment on asthma remains to be
elucidated. In the present study, the anti-inflammatory effect of
DHM in an OVA-induced asthmatic mouse model was investigated. It
was found that DHM effectively suppressed the infiltration of
inflammatory cells into the airways of the asthmatic mice,
decreased the numbers of eosinophils, macrophages, lymphocytes and
neutrophils into the BAL fluid, and inhibited the elevated levels
of IL-4, IL-5 and IL-13 in the BAL fluid. In addition, reduction in
the levels of OVA-specific IgE and IgG1 was observed in the serum
of mice challenged with DHM. The present study is the first, to the
best of our knowledge, to evaluate the effects of DHM in a
non-infectious mouse model of asthma.
Previous studies have indicated that asthma was
originally considered to be a Th2-mediated disease (25). Accordingly, Th2 cytokines have
distinct and significant effects in the pathogenesis of asthma.
Their overproduction induces the inflammatory response and airway
remodeling, and contributes to the initiation and pathogenesis of
acute asthma (26). Therefore,
cytokines have become a major target of novel therapies for asthma.
In the present study, it was found that the levels of IL-4, IL-5
and IL-13 in the BAL fluid were markedly elevated in OVA-challenged
mice, but were decreased following DHM treatment. In a previous
study, DHM was demonstrated to possess anti-inflammatory activity
through reducing the production of tumor necrosis factor-α and
cytokeratin-18 in patients with non-alcoholic fatty liver disease
(18). Proinflammatory cytokines,
including IL-4, IL-5 and IL-13, expressed by Th2 cells are directly
involved in the initiation and maintenance of allergic disease
(27). IL-4 may be responsible for
the production of IgE (28). IL-5
promotes the mobilization of eosinophils from the bone marrow, and
recruits eosinophils into the airways (29). IL-13 is important in eosinophilic
inflammation, mucus hypersecretion and airway luminal narrowing
(30). The data in the present
study suggested that DHM treatment decreased the levels of IL-4,
IL-5 and IL-13 in the OVA-induced asthmatic mouse, which at least
contributed to the anti-inflammatory effect of DHM.
Eosinophilia is a major hallmark of allergic
diseases. Eosinophils are the predominant inflammatory cells in
asthmatic lung tissues, and are known principal effector cells in
the pathogenesis of allergic inflammation (31). The recruitment of eosinophils into
the airways is a multistep process, which is coordinated by various
cytokines and adhesion molecules (32). The results of the present study
demonstrated that DHM treatment effectively reduced the number of
eosinophils in the BAL fluid of the OVA-challenged mice. Other
leukocytes, including neutrophils, macrophages and lymphocytes, are
also important mediators for the inflammatory response. In the
present study, DHM treatment ameliorated airway eosinophilia, as
shown by the decreased numbers of eosinophils, macrophages,
lymphocytes and neutrophils in the BAL fluid and lung tissues of
the OVA-sensitized mice. Additionally, the findings demonstrated
that DHM treatment significantly decreased mucus hypersecretion. A
previous study indicated that mucus hypersecretion was increased by
hypertrophy of goblet cells in the lung tissue of asthma, which is
involved in airway obstruction (33).
Increased levels of serum IgE and IgG1 are a
hallmark of the Th2 immune response, and it generally observed in
OVA-challenged animals, similar to the increase in pollen-specific
IgE in hayfever sufferers (34).
The biological activity of IgE is mediated through its interaction
with its high affinity IgE receptor on mast cells and basophils
(22). It has been reported that
the neutralization of IgE decreased the recruitment of eosinophils
into the airway following allergen challenge (35). In the present study, DHM treatment
inhibited the increased serum production of IgE and IgG1, which
suggested that the anti-allergy effect of DHM was associated with
the decreased production of IgE and IgG1.
AHR is a useful marker of airway abnormality in
asthma, and its development involves various inflammatory cells and
mediators. The data obtained in the present study demonstrated that
DHM significantly suppressed the OVA-induced AHR to inhaled
methacholine. IL-5-mediated eosinophilia is important in AHR
development by generating various proinflammatory products,
including cysteinyl-leukotrienes, major basic protein, eosinophilic
cationic protein and other lipid mediators, which are closely
associated with AHR (36).
Additionally, IL-4 and IL-13 have been reported to induce AHR in
mouse asthma models (37). Thus,
the DHM-mediated reduction of AHR may be associated with reduction
in the production of IL-4, IL-5 and IL-13.
Previous studies have indicated that the production
of several inflammatory cytokines is regulated by MAPKs and NF-κB
(38–40). The MAPK signaling cascade is
important in the activation of inflammatory cells. Suppression of
the extracellular signal-regulated kinase (ERK) signaling pathway
may be a therapeutic target for the treatment of allergic airway
inflammation (4). In addition,
when NF-κB is activated, several inflammatory cytokines are
upregulated in asthmatic airways, and the AHR and mucus secretion
are enhanced in allergic inflammation (41). Previous studies have suggested that
DHM inhibits the activation of NF-κB and the phosphorylation of p38
and c-Jun N-terminal kinase, but not ERK1/2, in
lipopolysaccharide-stimulated macrophages (18,20,42).
In the present study, it was hypothesized that DHM inhibited the
inflammatory response in the asthma model through a similar
mechanism; however, this requires clarification in future
investigations.
In conclusion, the present study showed that DHM
treatment effectively inhibited the increased number of
inflammatory cells, including eosinophils, macrophages, lymphocytes
and neutrophils, in the mouse asthma model induced by OVA, and also
effectively suppressed the elevated levels of IgE and IgG1, and of
the IL-4, IL-5 and IL-13 cytokines in the OVA-challenged mice.
Additionally, histological staining indicated that DHM treatment
markedly inhibited the infiltration of inflammatory cells in the
lung tissue and reduced mucus hypersecretion by goblet cells in the
airway. These findings suggested that DHM may have inhibitory
effects on airway inflammation and may be a potential therapeutic
agent for the treatment of asthma.
Acknowledgements
The authors would like to thank Dr Joel Thomson at
the Foreign Language Institute in Guangdong Medical College
(Zhanjiang, China) for proofreading the English of this
manuscript.
Glossary
Abbreviations
Abbreviations:
|
DHM
|
dihydromyricetin
|
|
OVA
|
ovalbumin
|
|
PBS
|
phosphate-buffered saline
|
|
Dex
|
dexamethasone
|
|
ELISA
|
enzyme-linked immunosorbent assay
|
|
BAL
|
bronchoalveolar lavage
|
|
NF-κB
|
nuclear factor κB
|
|
AHR
|
airway hyperresponsiveness
|
|
MAPKs
|
mitogen-activated protein kinases
|
References
|
1
|
Deveci F, Muz MH, Ilhan N, Kirkil G,
Turgut T and Akpolat N: Evaluation of the anti-inflammatory effect
of infliximab in a mouse model of acute asthma. Respirology.
13:488–497. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ci X, Chu X, Xiang H, Li X and Deng X:
Anti-inflammatory effects of tilmicosin in a noninfectious mouse
model of allergic asthma. Immunopharmacol Immunotoxicol.
33:626–632. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Munroe ME, Businga TR, Kline JN and Bishop
GA: Anti-inflammatory effects of the neurotransmitter agonist
Honokiol in a mouse model of allergic asthma. J Immunol.
185:5586–5597. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee SH, Kim DW, Kim HR, Woo SJ, Kim SM, Jo
HS, Jeon SG, Cho SW, Park JH, Won MH, et al: Anti-inflammatory
effects of Tat-Annexin protein on ovalbumin-induced airway
inflammation in a mouse model of asthma. Biochem Biophys Res
Commun. 417:1024–1029. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Murad HA and Hasanin AH: The
anti-inflammatory effects of 1,1 dimethyl-4-phenylpiperazinium
(DMPP) compared to dexamethasone in a guinea pig model of ovalbumin
induced asthma. Eur Rev Med Pharmacol Sci. 18:2228–2236.
2014.PubMed/NCBI
|
|
6
|
Kim DY, Park BS, Hong GU, Lee BJ, Park JW,
Kim SY and Ro JY: Anti-inflammatory effects of the R2 peptide, an
inhibitor of transglutaminase 2, in a mouse model of allergic
asthma, induced by ovalbumin. Br J Pharmacol. 162:210–225. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zeng G, Liu J, Chen H, Liu B, Zhang Q, Li
M and Zhu R: Dihydromyricetin induces cell cycle arrest and
apoptosis in melanoma SK-MEL-28 cells. Oncol Rep. 31:2713–2719.
2014.PubMed/NCBI
|
|
8
|
Shen Y, Lindemeyer AK, Gonzalez C, Shao
XM, Spigelman I, Olsen RW and Liang J: Dihydromyricetin as a novel
anti-alcohol intoxication medication. J Neurosci. 32:390–401. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ni F, Gong Y, Li L, Abdolmaleky HM and
Zhou JR: Flavonoid ampelopsin inhibits the growth and metastasis of
prostate cancer in vitro and in mice. PLoS One. 7:e388022012.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huang H, Hu M, Zhao R, Li P and Li M:
Dihydromyricetin suppresses the proliferation of hepatocellular
carcinoma cells by inducing G2/M arrest through the
Chk1/Chk2/Cdc25C pathway. Oncol Rep. 30:2467–2475. 2013.PubMed/NCBI
|
|
11
|
Murakami T, Miyakoshi M, Araho D, Mizutani
K, Kambara T, Ikeda T, Chou WH, Inukai M, Takenaka A and Igarashi
K: Hepatoprotective activity of tocha, the stems and leaves of
Ampelopsis grossedentata, and ampelopsin. Biofactors. 21:175–178.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liang J, Shen Y, Shao XM, Scott MB, Ly E,
Wong S, Nguyen A, Tan K, Kwon B, Olsen RW and Spigelman I:
Dihydromyricetin prevents fetal alcohol exposure-induced behavioral
and physiological deficits: The roles of GABAA receptors in
adolescence. Neurochem Res. 39:1147–1161. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Meng G, Yang S, Chen Y, Yao W, Zhu H and
Zhang W: Attenuating effects of dihydromyricetin on angiotensin
II-induced rat cardiomyocyte hypertrophy related to antioxidative
activity in a NO-dependent manner. Pharm Biol. 53:904–912. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jiang B, Le L, Pan H, Hu K, Xu L and Xiao
P: Dihydromyricetin ameliorates the oxidative stress response
induced by methylglyoxal via the AMPK/GLUT4 signaling pathway in
PC12 cells. Brain Res Bull. 109:117–126. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Liao W, Ning Z, Ma L, Yin X, Wei Q, Yuan
E, Yang J and Ren J: Recrystallization of dihydromyricetin from
Ampelopsis grossedentata and its anti-oxidant activity evaluation.
Rejuvenation Res. 17:422–429. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhao Z, Yin JQ, Wu MS, Song G, Xie XB, Zou
C, Tang Q, Wu Y, Lu J, Wang Y, et al: Dihydromyricetin activates
AMP-activated protein kinase and P38(MAPK) exerting antitumor
potential in osteosarcoma. Cancer Prev Res. 7:927–938. 2014.
View Article : Google Scholar
|
|
17
|
Zhu H, Luo P, Fu Y, Wang J, Dai J, Shao J,
Yang X, Chang L, Weng Q, Yang B and He Q: Dihydromyricetin prevents
cardiotoxicity and enhances anticancer activity induced by
adriamycin. Oncotarget. 6:3254–3267. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen S, Zhao X, Wan J, Ran L, Qin Y, Wang
X, Gao Y, Shu F, Zhang Y, Liu P, et al: Dihydromyricetin improves
glucose and lipid metabolism and exerts anti-inflammatory effects
in nonalcoholic fatty liver disease: A randomized controlled trial.
Pharmacol Res. 99:74–81. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qi S, Xin Y, Guo Y, Diao Y, Kou X, Luo L
and Yin Z: Ampelopsin reduces endotoxic inflammation via repressing
ROS-mediated activation of PI3K/Akt/NF-κB signaling pathways. Int
Immunopharmacol. 12:278–287. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hou XL, Tong Q, Wang WQ, Shi CY, Xiong W,
Chen J, Liu X and Fang JG: Suppression of inflammatory responses by
dihydromyricetin, a flavonoid from ampelopsis grossedentata, via
inhibiting the activation of NF-κB and MAPK signaling pathways. J
Nat Prod. 78:1689–1696. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Yang EJ, Lee JS, Yun CY, Ryang YS, Kim JB
and Kim IS: Suppression of ovalbumin-induced airway inflammatory
responses in a mouse model of asthma by Mimosa pudica extract.
Phytother Res. 25:59–66. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Duan W, Chan JH, Wong CH, Leung BP and
Wong WS: Anti-inflammatory effects of mitogen-activated protein
kinase kinase inhibitor U0126 in an asthma mouse model. J Immunol.
172:7053–7059. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee M, Kim S, Kwon OK, Oh SR, Lee HK and
Ahn K: Anti-inflammatory and anti-asthmatic effects of resveratrol,
a polyphenolic stilbene, in a mouse model of allergic asthma. Int
Immunopharmacol. 9:418–424. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bisset LR and Schmid-Grendelmeier P:
Chemokines and their receptors in the pathogenesis of allergic
asthma: Progress and perspective. Curr Opin Pulm Med. 11:35–42.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nakajima H and Takatsu K: Role of
cytokines in allergic airway inflammation. Int Arch Allergy
Immunol. 142:265–273. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ngoc PL, Gold DR, Tzianabos AO, Weiss ST
and Celedón JC: Cytokines, allergy, and asthma. Curr Opin Allergy
Clin Immunol. 5:161–166. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Elias JA, Lee CG, Zheng T, Ma B, Homer RJ
and Zhu Z: New insights into the pathogenesis of asthma. J Clin
Invest. 111:291–297. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yan S, Ci X, Chen N, Chen C, Li X, Chu X,
Li J and Deng X: Anti-inflammatory effects of ivermectin in mouse
model of allergic asthma. Inflamm Res. 60:589–596. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Palmqvist C, Wardlaw AJ and Bradding P:
Chemokines and their receptors as potential targets for the
treatment of asthma. Br J Pharmacol. 151:725–736. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Rosenberg HF, Phipps S and Foster PS:
Eosinophil trafficking in allergy and asthma. J Allergy Clin
Immunol. 119:1303–1312. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kim DY, Ryu SY, Lim JY, Lee YS and Ro JY:
Anti-inflammatory mechanism of simvastatin in mouse allergic asthma
model. Eur J Pharmacol. 557:76–86. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jia GQ, Gonzalo JA, Hidalgo A, Wagner D,
Cybulsky M and Gutierrez-Ramos JC: Selective eosinophil
transendothelial migration triggered by eotaxin via modulation of
Mac-1/ICAM-1 and VLA-4/VCAM-1 interactions. Int Immunol. 11:1–10.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Woodruff PG and Fahy JV: A role for
neutrophils in asthma? Am J Med. 112:498–500. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wu AY, Chik SC, Chan AW, Li Z, Tsang KW
and Li W: Anti-inflammatory effects of high-dose montelukast in an
animal model of acute asthma. Clin Exp Allergy. 33:359–366. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Coyle AJ, Wagner K, Bertrand C, Tsuyuki S,
Bews J and Heusser C: Central role of immunoglobulin (Ig) E in the
induction of lung eosinophil infiltration and T helper 2 cell
cytokine production: Inhibition by a non-anaphylactogenic anti-IgE
antibody. J Exp Med. 183:1303–1310. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Vargaftig BB and Singer M: Leukotrienes
mediate murine bronchopulmonary hyperreactivity, inflammation, and
part of mucosal metaplasia and tissue injury induced by recombinant
murine interleukin-13. Am J Respir Cell Mol Biol. 28:410–419. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Taube C, Duez C, Cui ZH, Takeda K, Rha YH,
Park JW, Balhorn A, Donaldson DD, Dakhama A and Gelfand EW: The
role of IL-13 in established allergic airway disease. J Immunol.
169:6482–6489. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Inoue H, Kato R, Fukuyama S, Nonami A,
Taniguchi K, Matsumoto K, Nakano T, Tsuda M, Matsumura M, Kubo M,
et al: Spred-1 negatively regulates allergen-induced airway
eosinophilia and hyperresponsiveness. J Exp Med. 201:73–82. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhu Q, Xu X, Liu X, Lin J, Kan Y, Zhong Y,
Liu F and Xu J: Sodium houttuyfonate inhibits inflammation by
blocking the MAPKs/NF-κB signaling pathways in bovine endometrial
epithelial cells. Res Vet Sci. 100:245–251. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wu H, Zhao G, Jiang K, Chen X, Rui G, Qiu
C, Guo M and Deng G: IFN-τ alleviates lipopolysaccharide-induced
inflammation by suppressing NF-κB and MAPKs pathway activation in
mice. Inflammation. 39:1141–1150. 2016.PubMed/NCBI
|
|
41
|
Sheller JR, Polosukhin VV, Mitchell D,
Cheng DS, Peebles RS and Blackwell TS: Nuclear factor kappa B
induction in airway epithelium increases lung inflammation in
allergen-challenged mice. Exp Lung Res. 35:883–895. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Tang N, Ma J, Wang KS, Mi C, Lv Y, Piao
LX, Xu GH, Li X, Lee JJ and Jin X: Dihydromyricetin suppresses
TNF-α-induced NF-κB activation and target gene expression. Mol Cell
Biochem. 422:11–20. 2016. View Article : Google Scholar : PubMed/NCBI
|