Introduction
As the most common sustained arrhythmia diagnosed in
the clinic, atrial fibrillation (AF) significantly increases the
mortality and morbidity of patients by impairing cardiac function
and causing stroke (1).
Epidemiological studies have demonstrated that diabetes mellitus
(DM) is one of the major risk factors leading to the pathogenesis
of AF, which increases the risk by ~40% (2). It was previously reported that
autonomic, electrical, electromechanical and structural remodeling,
including oxidative stress, connexin remodeling and glycemic
fluctuations, triggered by DM, contribute to AF pathophysiology
(3). However, the underlying
mechanism of the mutual relationship between AF and DM remains
mostly unknown, which limits the prevention and treatment of
DM-induced AF. Streptozotocin (STZ) is a natural chemical, which
can be taken up by pancreatic B cells via the glucose transporter
and exert toxic effects. Due to its distinctive effect, STZ is
widely applied as a tool to induce experimental DM animal models
(4). Hayami et al (5) investigated the impact of a DPP-4
inhibitor on AF in a rat model induced by STZ, and found that the
administration of STZ greatly increased atrial fibrosis, but
sulfonylurea and DPP-4 inhibitors inhibited inflammation and
fibrosis of the atria.
Previous research has demonstrated that inflammation
and oxidative stress play a critical role in the relationship
between DM and AF (6). Therefore,
agents mitigating inflammation and oxidative stress might be useful
in preventing DM-induced AF. Hydrogen sulfide (H2S) has
drawn considerable attention, not only due to its inherent activity
in human physiology, but also because of its potential as a
cardiovascular protector (7). Most
studies of H2S and cardiovascular disorders have focused
on myocardial ischemia/reperfusion injury rather than arrhythmia,
especially AF (7,8). In addition, there is evidence that
downregulated PI3K-Akt-eNOS expression is related to an increased
AF inducibility in diabetic rats (9). In addition, it has been noted that
H2S is associated with inflammation and oxidative-stress
responses (10,11). In the present study, it was
hypothesized that H2S could reverse AF and reduce the
incidence of AF in diabetic rats via the PI3K-Akt-eNOS signaling
pathway, so the effect of H2S on DM-induced AF and its
underlying mechanisms were explored.
Materials and methods
Animal model
A total of 80 adult Sprague-Dawley (SD) rats were
used in this study, which was approved by the Experimental Animal
Administration Committee of the Second Military Medical University
(Shanghai, China). Animal experiments were performed following the
Guide for the Care and Use of Laboratory Animals (National
Institutes of Health publication 85–23, revised 1996). The
12-week-old male rats (weight 200–220 g) were randomly divided into
the control group, the DM group, the H2S group, and the
DM+H2S group (each group included 20 rats). All rats
were fed a routine diet and maintained in a standard room
environment (18-23°C, humidity 40–60%, 12-h light/dark cycle, and
free access to food and water). Animal health and behavior were
monitored and evaluated every week, including general condition,
appetite, sleep status and survival.
Rats of the DM group and the DM+H2S group
were administered STZ (60 mg/kg; Wako Chemicals USA, Inc.)
dissolved in citrate buffer (Sigma-Aldrich; Merck KGaA)
intraperitoneally (i.p.) at the age of 12 weeks. After one week,
the rats were tested for fasting blood glucose (FBG) level. The
fasting time was 16 h. If the FBG level was >200 mg/dl, then the
rats were selected for the following experiments (5). At the same time, the control group
and the H2S group were administered citrate buffer only.
After the injection, the H2S group and the
DM+H2S group were administered 15 µmol/kg (i.p.) sodium
hydrosulfide (NaHS, exogenous H2S donor; Sigma-Aldrich;
Merck KGaA) every week for 8 consecutive weeks, whereas the control
group and the DM group were administered normal saline only. At the
age of 20 weeks, all rats were subjected to the following
experiments.
Intraperitoneal glucose tolerance test
(IPGTT) and intraperitoneal insulin tolerance test (IPITT)
As previously reported (12), IPITT and IPGTT were conducted at
the age of 20 weeks. In terms of IPGTT, the rats were fasted
overnight for 15 h, and were given 1.5 gr/kg glucose through an
i.p. injection. Blood was collected from the tail vein for glucose
measurements at 0, 10, 20, 30, 60, 90 and 120 min after glucose
injection. As for IPITT, the rats received 2.5 U/kg insulin via
i.p. injection, and then blood was drawn from the tail vein for
glucose measurements at 0, 20, 30, 40, 60, 90 and 120 min after
insulin administration.
Intracardiac programmed electrical
stimulus
As previously described, all groups were examined
with electrophysiological characteristics via intracardiac
programmed electrical stimulus (13). Each animal was anesthetized with 2%
isoflurane (Beijing Hongxin Technology) inhalation and fixed on a
heated pad at the prone position to maintain 37°C body temperature.
Surface electrocardiogram (ECG; B&W TEKSystems, Inc.) and
intracardiac electrograms were recorded simultaneously. P wave
duration and an indicator of intra-atrial conduction time were
measured. An electrode catheter (1.1 F; Millar) was placed into the
right atrium through the right jugular vein. A burst of electrical
stimuli for 30 sec was used to test the inducibility of atrial
arrhythmias. The burst test was conducted 3 times, and >two
incidents of AF observed (P wave disappeared and lasted >2 sec)
was judged as the onset of AF. LabChart Software 7.0
(ADInstruments) was used to record and analyze electrocardiogram
data.
Western blot analysis
As previously described (14), expression levels of key proteins of
the PI3K/Akt/endothelial nitric oxide synthase (eNOS) pathway in
the atrial myocardium were examined with western blotting. The
membranes were incubated with the following primary antibodies
overnight at 4°C, anti-PI3K (1:2,000, cat. no. ab151549; Abcam),
anti-Akt (1:2,000, cat. no. ab8805; Abcam), anti-phosphorylated
(p)-Akt (1:500, cat. no. 9611; Cell Signaling Technology, Inc.),
anti-p-eNOS (1:500, cat. no. ab184154; Abcam), anti-eNOS (1:500,
cat. no. ab76198, Abcam) and anti-β-actin (1:5,000, cat. no.
ab179467; Abcam). Following the primary incubation, membranes were
incubated with rabbit anti-mouse (1:5,000, cat. no. ab150113;
Abcam) or goat anti-rabbit HRP-conjugated secondary antibody
(1:5,000, cat. no. ab150077; Abcam). Gel Imaging system (Bio-Rad
Laboratories, Inc.) and ImageJ software (Version 1.8, National
Institutes of Health) were used to image and analyze the western
blotting bands.
Reverse transcription-quantitative
(RT-q)PCR
Total RNA from atrial myocardium samples was
extracted using TRIzol (Takara Biotechnology Co., Ltd.). Total RNA
(1,000 ng) was reverse transcribed into cDNA using the
Prime-Script™ RT Reagent kit (Takara Biotechnology Co., Ltd.).
Before performing the RT reaction, RNA (10 µl) was heated to 65°C
for 5–10 min, and then quenched on ice. Then, the inversion system
was prepared according to the instructions of the cDNA kit, the
sample was placed at 25°C for 10 min and then incubated at 42°C for
1 h. Following which, the cDNA was denatured at 95°C and placed on
ice.
RT-qPCR was performed using SYBR-Green (Takara
Biotechnology Co., Ltd.) and normalized to β-actin expression. The
fibroblast-to-myofibroblast transition marker α-smooth muscle
actin, and atrial fibrosis markers, transforming growth factor
(TGF)-β, collagen I, collagen III, were examined. A total of 30
cycles of PCR were performed: Denaturation at 95°C for 30 sec,
annealing at 60°C for 45 sec, and extension at 72°C for 60 sec.
The primer sequences are listed as follows: Akt,
5′-AGCATGGAGTGTGTGGACAG-3′ (forward) and 5′-GATGATCCATGCGGGGCTT-3′
(reverse); eNOS, 5′-CGACTATCCTGTATGGCTCTGAG-3′ (forward) and
5′-GATCCCCATTGCCAAATGTGC-3′ (reverse); PI3K,
5′-GCTCTTTCCCCAGCTGAACT-3′ (forward) and 5′-ACACAGTGTCGCTGGTTTGA-3′
(reverse); β-actin: 5′-CATCCTGCGTCTGGACCGG-3′ (forward) and
5′-TAATGTCACGCACGATTTCC-3′ (reverse); TGF-β,
5′-CCCAGCATCTGCAAAGCTC-3′ (forward) and 5′-GTCAATGTACAGCTGCCGCA-3′
(reverse); collagen I, 5′-CATGTTCAGCTTTGTGGACCT-3′ (forward) and
5′-GCAGCTGACTTCAGGGATGT-3′ (reverse). The average expression of
β-actin was used as an internal reference gene to normalize input
cDNA. Relative gene expression was calculated via the threshold
cycle value (CT) and the formula 2−∆∆Cq (15). All of the reactions were repeated
at least twice, with at least 3 replicates for every sample.
Masson's trichrome staining
According to a previous report (16), Masson's trichrome staining was
conducted to evaluate the extent of atrial fibrosis. After the rats
were sacrificed, atrium samples were rapidly excised, rinsed with
PBS, fixed in 4% paraformaldehyde at 4°C overnight, and embedded in
paraffin. Then, 5-µm-thick sections at of the atrium were cut.
Masson's trichrome kit (cat. no. HT15; Sigma-Aldrich; Merck KGaA)
was used according to the manufacturer's instruction. ImageJ
software (Version 1.8; National Institutes of Health) was used to
evaluate the area of fibrosis. Each section was examined in 5
randomly-selected high-power fields (×400) and middle-power fields
(×200) under a light microscope. Collagen volume fraction
(CVF)=Collagen area (blue)/Total area ×100%.
Cell culture
Cardiac fibroblasts (CFs) were harvested from the
different groups, according to a previous report (17). Following attachment to uncoated
culture plates, all unattached or weakly attached cells were
removed. Then, the attached fibroblasts were washed and grown in
DMEM (Gibco; Thermo Fisher Scientific, Inc.) supplemented with 10%
FBS (Gibco; Thermo Fisher Scientific, Inc.) at 37°C. CFs were
plated on a 96-well plate at a density of 1×104/well and
cultured for 24 h.
Cell proliferation assay
As previously described (18), cell proliferation was examined
using an MTT assay. Data values are expressed as fold-change
compared with the control group.
Cell migration
As previously described (18), cell migration was examined with the
real-time cell analyzer (RTCA) migration experiment. The CFs were
seeded in RTCA Cim-16 plates in a serum-free DMEM medium with a
cell density of at least 20,000/well. A chemoattractant of full
growth medium (DMEM with 5–10% bovine serum albumin; cat. no.
A1933; Sigma-Aldrich; Merck KGaA) was applied in the lower chamber.
The RTCA device (xCELLigence RTCA; Roche Diagnostics) was used for
measurements in a time-resolved manner (18). The values are expressed as
fold-change compared with the control group.
Statistical analysis
GraphPad Prism 7.0 (GraphPad Software, Inc.) was
used for statistical analysis. The AF incidence of four groups was
compared with the Chi-square test. For comparison of normally
distributed variables, one-way ANOVA and Tukey's post hoc test was
performed. For comparison of AF duration, Kruskal-Wallis test and
Dunn's multiple comparisons post hoc test were conducted. Data are
presented as the mean ± SD. P<0.05 was considered to indicate a
statistically significant difference.
Results
DM model results
As demonstrated in Fig.
1, the FBG value was evaluated in the four groups at different
points, including before the STZ injection, 1, 4 and 8 weeks after
STZ injection. Before the injection, there was no difference in FBG
among the four groups (P=0.5204), and the FBG varied between 90 and
110 mg/dl (Fig. 1A). However, 1
week after the STZ injection, the DM group and the
DM+H2S group demonstrated a significant increase in the
FBG level to 410.8±92.0 and 454.1±93.4 mg/dl, respectively, which
were significantly higher than the control group and the
H2S group (P<0.0001). At the same time, there was no
significant difference between the DM and DM+H2S group,
and between the control group and the H2S group (both
P>0.05; Fig. 1B). The FBG level
was examined 4 and 8 weeks after STZ injection, when NaHS had been
administered. The results presented similar trends with the FBG
level 1 week after STZ injection. The FBG of the DM group and the
DM+H2S group was significantly higher than the control
group and the H2S group (P<0.0001). At the same time,
there was no difference between the DM group and the
DM+H2S group, the control group and the H2S
group (both P>0.05) (Fig. 1C and
D).
IPITT and IPGTT (Fig.
1E and F) was performed to test insulin tolerance and glucose
tolerance. The results were consistent with the FBG test, showing
that the DM group and the DM+H2S group shared similar
insulin and glucose tolerance, which was notably higher than the
control group and the H2S group. However, there was no
difference between the control group and the H2S group,
and no difference DM+H2S group and the DM group. No
significant side effects of NaHS were observed in the
H2S group and the DM+H2S group.
AF inducibility and persistence
As shown in Fig. 2,
the intracardiac programmed electrical stimulus was applied to
examine the AF inducibility of the four groups. Fig. 2A shows representative ECG figures
of burst pacing and the subsequent heart rhythm. Compared with the
other three groups, the DM group exhibited a much higher
susceptibility of induced AF, with a significantly higher AF
incidence (P=0.017). There was no statistical difference between
the control group, the H2S group and the
DM+H2S group in AF incidence (Fig. 2B). The AF duration of the DM group
was significantly higher than the control group and the
H2S group (P=0.005). Although the AF duration of the
DM+H2S group was lower than the DM group, there was no
statistical significance (P=0.085; Fig. 2C).
Atrial fibrosis
Atrial remodeling of the four groups was also
evaluated using Masson's trichrome staining (Fig. 3). More blue-stained collagen was
observed in the DM group, indicating a more severe atrial fibrosis
than the other groups, whereas the DM+H2S group suffered
less fibrosis than the DM group (Fig.
3A). Fibrosis was quantified the with ImageJ software. The CVF
value was calculated for the four groups, which indicated that the
CVF of the DM group was significantly higher than the other groups
(P<0.0001). At the same time, there was no significant
difference among the control group, the H2S group and
the DM+H2S group (all P>0.05; Fig. 3B). The key markers of fibrosis,
including TGF-β and Collagen I, were also determined (Fig. 3C and D), which demonstrated that
TGF-β and Collagen I of the DM group was significantly higher than
the other groups (P<0.0001). Fibrosis of the different groups
was also examined at the cellular level by comparing the
proliferation and migration of CFs. CF proliferation and migration
of the DM group was significantly increased. In contrast,
proliferation and migration of the DM+H2S group were
lower than the DM group (P<0.0001; Fig. 3E and F).
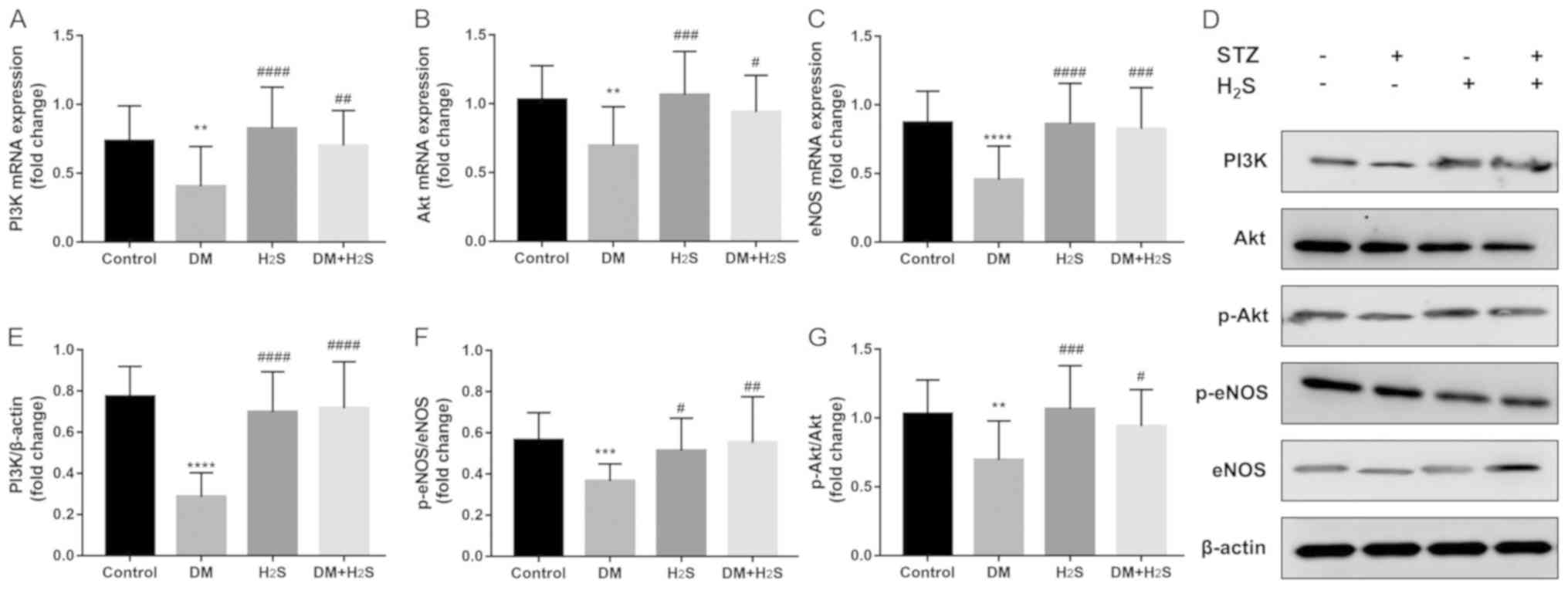
PI3K/Akt/eNOS signaling pathway
As shown in Fig. 4,
the classic PI3K/Akt/eNOS signaling pathway was evaluated in the
four groups with RT-qPCR (Fig.
4A-C) and western blot analysis (Fig. 4D-G). The results demonstrated that
this pathway was significantly downregulated in the DM group
compared with the control group, which was reversed in the
DM+H2S group. The expression levels of PI3K/Akt/eNOS
were significantly higher in the DM+H2S group
(P<0.0001). Compared with the DM group, p-Akt/Akt and
p-eNOS/eNOS ratios were significantly increased in the
DM+H2S group (Fig. 4F and
G).
Discussion
H2S, an endogenous active molecule, has
been demonstrated to be effective in organ protection for
ischemia/reperfusion injury (8).
However, data concerning its effect on AF incidence, especially on
DM-induced AF, is minimal. In the present study, SD rats were used
as the research subject and a DM model was successfully established
using STZ. It was demonstrated that DM rats had higher AF incidence
and duration, which is associated with worse atrial fibrosis. It
was also found that H2S could reduce AF incidence and
mitigate the atrial fibrosis, which was achieved via the
PI3K/Akt/eNOS pathway. Although there was no statistical difference
between the DM group and DM+H2S group in AF duration,
which could be attributed to the sample size, we propose that
H2S could also shorten AF duration.
There are several ways to build DM animal models,
including Zucker Diabetic Fatty rats, BioBreeding rats,
LEW.1AR1-iddm rats, Goto-Kakizaki rats, chemically induced diabetic
models, and non-obese diabetic mouse and Akita mouse models
(19). Hayami et al used
STZ to damage pancreatic islet B cells and significantly increase
blood glucose, and found that diabetic rats suffered severe
inflammation and atrial fibrosis (5). The present study used the same models
as Hayami, and found that diabetic rats had not only worse atrial
fibrosis, but also higher AF incidence and duration. Notably, the
application of STZ for the DM model causes islet B cell injury and
a shortage of insulin, which is similar to type 1 diabetes without
insulin resistance. Saito et al (4) used another diabetic rat model by
administrating a high-fat diet and low-doses of STZ. In this way,
the rats had the characteristics of insulin resistance and high
blood glucose, which simulates type 2 diabetes.
Research on DM and AF has demonstrated that
autonomic, electrical, electromechanical and structural remodeling,
including oxidative stress, connexin remodeling and glycemic
fluctuations, could be important reasons why patients with DM are
at higher risk of AF (20). Among
all the mechanisms, oxidative stress and related structural
remodeling lay the foundation of abnormal electrical activity
(6). Chang et al (21) led a large-scale cohort study and
found that metformin use was associated with a decreased risk of AF
in patients with type 2 DM who were not using other anti-diabetic
medication, most likely via attenuation of atrial cell
tachycardia-induced myolysis and oxidative stress. Another study
used the xanthine oxidase inhibitor allopurinol to prevent
oxidative stress-mediated atrial remodeling in alloxan-induced DM
rabbits (22).
Activation of the PI3K/Akt/eNOS signaling pathway is
associated with reduced reactive oxygen species production
(23,24). Chong et al (25) found that resveratrol could decrease
left atrial fibrosis and regulate variation in ion channels to
reduce AF through the PI3K/Akt/eNOS signaling pathway. Hydrogen
sulfide is closely associated with the PI3K/Akt pathway. Xiao et
al (26) investigated the
effects of hydrogen sulfide on myocardial fibrosis and found that
the protective effect of H2S against diabetes-induced
myocardial fibrosis might be associated with the attenuation of
autophagy via the upregulation of the PI3K/Akt1 signaling pathway.
The present study found that H2S could significantly
upregulate the PI3K/Akt/eNOS signaling pathway and reduce atrial
fibrosis induced by DM. However, Xiao et al (26) demonstrated decreased autophagy
resulted from PI3K/Akt1 activation, which was not found in this
study. Another study led by Liu et al (27) also confirmed that H2S
could ameliorate rat myocardial fibrosis induced by thyroxine,
which may be associated with autophagy activated by upregulation of
the PI3K/Akt signaling pathway and downregulation of miR-21,
miR-34a and miR-214.
Several limitations of the present study must be
noted. Firstly, despite the protective effect of H2S on
DM-induced AF and atrial fibrosis, further mechanisms, such as
inflammation, apoptosis or autophagy, were not investigated in this
study due to limited time and funds. Secondly, this study only used
the STZ-induced DM model, which is similar to type 1 DM, so
conclusions are limited. Finally, electrical remodeling and cardiac
structural function could be altered by DM status, which was also
not investigated. However, these limitations can be resolved in
further studies.
In conclusion, DM can lead to the structural
remodeling of atrial fibrosis, increasing AF incidence and
persistence. Administration of H2S does not affect
glucose metabolism, but can significantly mitigate atrial fibrosis
and reduce the incidence of AF, probably via the activation of the
PI3K/Akt/eNOS pathway.
Acknowledgements
Not applicable.
Funding
This study was supported by the Outstanding Young
Physician Program of Changzheng Hospital, Young Physician Startup
Fund of Changzheng Hospital, and Project of Shanghai Science and
Technology Commission (grant no. 17ZR1439100).
Availability of data and materials
The datasets used and or/analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XX and JX designed the study. XX, QY and XL acquired
and interpreted the data. WX, PW, and JS conducted the animal
experiments. QY and JX prepared the manuscript and supervised the
study protocol. All authors read and approved the manuscript and
agree to be accountable for all aspects of the research in ensuring
that the accuracy or integrity of any part of the work are
appropriately investigated and resolved.
Ethics approval and consent to
participate
The present study was approved by the Experimental
Animal Administration Committee of the Second Military Medical
University (Shanghai, China). Animal experiments were performed
following the Guide for the Care and Use of Laboratory Animals
(National Institutes of Health publication 85–23, revised
1996).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lip GY, Tse HF and Lane DA: Atrial
fibrillation. Lancet. 379:648–661. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bell DSH and Goncalves E: Atrial
fibrillation and type 2 diabetes: Prevalence, etiology,
pathophysiology and effect of anti-diabetic therapies. Diabetes
Obes Metab. 21:210–217. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Proietti R, Russo V, Wu MA, Maggioni AP
and Marfella R: Diabetes mellitus and atrial fibrillation: Evidence
of a pathophysiological, clinical and epidemiological association
beyond the thromboembolic risk. G Ital Cardiol (Rome). 18:199–207.
2017.(In Italian). PubMed/NCBI
|
|
4
|
Saito S, Teshima Y, Fukui A, Kondo H,
Nishio S, Nakagawa M, Saikawa T and Takahashi N: Glucose
fluctuations increase the incidence of atrial fibrillation in
diabetic rats. Cardiovasc Res. 104:5–14. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hayami N, Sekiguchi A, Iwasaki YK,
Murakawa Y and Yamashita T: No additional effect of DPP-4 inhibitor
on preventing atrial fibrosis in streptozotocin-induced diabetic
rat as compared with sulfonylurea. Int Heart J. 57:336–340. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Karam BS, Chavez-Moreno A, Koh W, Akar JG
and Akar FG: Oxidative stress and inflammation as central mediators
of atrial fibrillation in obesity and diabetes. Cardiovasc
Diabetol. 16:1202017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wu D, Wang J, Li H, Xue M, Ji A and Li Y:
Role of hydrogen sulfide in ischemia-reperfusion injury. Oxid Med
Cell Longev. 2015:1869082015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Citi V, Piragine E, Testai L, Breschi MC,
Calderone V and Martelli A: The role of hydrogen sulfide and
H2S-donors in myocardial protection against ischemia/reperfusion
injury. Curr Med Chem. 25:4380–4401. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang FL, Chu SL, Wang WW and Chen LL:
Downregulated PI3K-Akt-eNOS expression is related to increased
atrial fibrillation inducibility in diabetic rats. Zhonghua Xin Xue
Guan Bing Za Zhi. 46:376–381. 2018.(In Chinese). PubMed/NCBI
|
|
10
|
Olas B: Hydrogen sulfide in signaling
pathways. Clin Chim Acta. 439:212–218. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Toldo S, Das A, Mezzaroma E, Chau VQ,
Marchetti C, Durrant D, Samidurai A, Van Tassell BW, Yin C, Ockaili
RA, et al: Induction of microRNA-21 with exogenous hydrogen sulfide
attenuates myocardial ischemic and inflammatory injury in mice.
Circ Cardiovasc Genet. 7:311–320. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sohrabipour S, Sharifi MR, Talebi A,
Sharifi M and Soltani N: GABA dramatically improves glucose
tolerance in streptozotocin-induced diabetic rats fed with high-fat
diet. Eur J Pharmacol. 826:75–84. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jin X, Jiang Y, Xue G, Yuan Y, Zhu H, Zhan
L, Zhuang Y, Huang Q, Shi L, Zhao Y, et al: Increase of late sodium
current contributes to enhanced susceptibility to atrial
fibrillation in diabetic mice. Eur J Pharmacol. 857:1724442019.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Luo T, Chen B and Wang X: 4-PBA prevents
pressure overload-induced myocardial hypertrophy and interstitial
fibrosis by attenuating endoplasmic reticulum stress. Chem Biol
Interact. 242:99–106. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Meng T, Cheng G, Wei Y, Ma S, Jiang Y, Wu
J, Zhou X and Sun C: Exposure to a chronic high-fat diet promotes
atrial structure and gap junction remodeling in rats. Int J Mol
Med. 40:217–225. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shen H, Wang J, Min J, Xi W, Gao Y, Yin L,
Yu Y, Liu K, Xiao J, Zhang YF and Wang ZN: Activation of
TGF-β1/α-SMA/Col I profibrotic pathway in fibroblasts by galectin-3
contributes to atrial fibrosis in experimental models and patients.
Cell Physiol Biochem. 47:851–863. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ma J, Ma S, Yin C and Wu H: Matrine
reduces susceptibility to postinfarct atrial fibrillation in rats
due to antifibrotic properties. J Cardiovasc Electrophysiol.
29:616–627. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Al-Awar A, Kupai K, Veszelka M, Szűcs G,
Attieh Z, Murlasits Z, Török S, Pósa A and Varga C: Experimental
diabetes mellitus in different animal models. J Diabetes Res.
2016:90514262016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Goudis CA, Korantzopoulos P, Ntalas IV,
Kallergis EM, Liu T and Ketikoglou DG: Diabetes mellitus and atrial
fibrillation: Pathophysiological mechanisms and potential upstream
therapies. Int J Cardiol. 184:617–622. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chang SH, Wu LS, Chiou MJ, Liu JR, Yu KH,
Kuo CF, Wen MS, Chen WJ, Yeh YH and See LC: Association of
metformin with lower atrial fibrillation risk among patients with
type 2 diabetes mellitus: A population-based dynamic cohort and in
vitro studies. Cardiovasc Diabetol. 13:1232014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yang Y, Zhao J, Qiu J, Li J, Liang X,
Zhang Z, Zhang X, Fu H, Korantzopoulos P, Letsas KP, et al:
Xanthine oxidase inhibitor allopurinol prevents oxidative
stress-mediated atrial remodeling in alloxan-induced diabetes
mellitus rabbits. J Am Heart Assoc. 7:e0088072018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wang R, Peng L, Zhao J, Zhang L, Guo C,
Zheng W and Chen H: Gardenamide a protects RGC-5 cells from
H(2)O(2)-induced oxidative stress insults by activating
PI3K/Akt/eNOS signaling pathway. Int J Mol Sci. 16:22350–22367.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chu P, Han G, Ahsan A, Sun Z, Liu S, Zhang
Z, Sun B, Song Y, Lin Y, Peng J and Tang Z: Phosphocreatine
protects endothelial cells from Methylglyoxal induced oxidative
stress and apoptosis via the regulation of PI3K/Akt/eNOS and NF-κB
pathway. Vascul Pharmacol. 91:26–35. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chong E, Chang SL, Hsiao YW, Singhal R,
Liu SH, Leha T, Lin WY, Hsu CP, Chen YC, Chen YJ, et al:
Resveratrol, a red wine antioxidant, reduces atrial fibrillation
susceptibility in the failing heart by PI3K/AKT/eNOS signaling
pathway activation. Heart Rhythm. 12:1046–1056. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xiao T, Luo J, Wu Z, Li F, Zeng O and Yang
J: Effects of hydrogen sulfide on myocardial fibrosis and
PI3K/AKT1-regulated autophagy in diabetic rats. Mol Med Rep.
13:1765–1773. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liu M, Li Z, Liang B, Li L, Liu S, Tan W,
Long J, Tang F, Chu C and Yang J: Hydrogen sulfide ameliorates rat
myocardial fibrosis induced by thyroxine through PI3K/AKT signaling
pathway. Endocr J. 65:769–781. 2018. View Article : Google Scholar : PubMed/NCBI
|