Introduction
Acute kidney injury (AKI) is a common clinical
phenomenon, and a major cause of high morbidity and mortality
during the perioperative period (1–3).
During the short term (~6 h) after AKI has occurred, the glomerular
filtration decreases sharply, the serum creatinine and blood urea
nitrogen (BUN) increase, and the urine volume decreases, which
results in variable kidney damage and eventually chronic kidney
disease or terminal-stage renal disease (4,5).
Conservative treatment and renal alternative therapy are the
commonly used treatments for AKI; however, they cannot effectively
prevent or intervene in AKI. Therefore, there is an urgent need to
for research on the pathogenesis of AKI and the development of new
treatment options, so as to improve the treatment effects of
AKI.
Ferroptosis is an iron-dependent non-apoptotic type
of cell death caused by intracellular lipid peroxidation metabolism
disorder, which is mainly characterized by the accumulation of
lipid peroxides and the overload of iron ions (6). When the acyl-CoA synthetase
long-chain family member 4 (ACSL4) is overactivated and the
glutathione peroxidase (GPX4) expression is reduced, iron
accumulates and induces ferroptosis (7). It has been reported that ferroptosis
is also a major pathological basis for the occurrence and
development of AKI (8).
Reduced glutathione (RGSH) combines with peroxides
and free radicals, which provides anti-oxidation effects, regulates
the metabolism and protects cells. RGSH has been used in the
adjuvant therapy of numerous diseases, such as liver, brain and
kidney diseases. It has been previously reported that RGSH can
provide protective effects in ischemia-reperfusion AKI (9), but whether its protective mechanism
is related to ferroptosis is unclear.
In the present study, by constructing in
vitro and in vivo AKI models, with ferroptosis as an
entry point, the mechanism of RGSH in ameliorating AKI was
evaluated.
Materials and methods
HK-2 cell culture
HK-2 cells were purchased from The Cell Bank of Type
Culture Collection of The Chinese Academy of Sciences, and cultured
in DMEM (containing 10% fetal bovine serum, 100 U/ml penicillin and
100 U/ml streptomycin; Gibco; Thermo Fisher Scientific, Inc.) at
37°C in a 5% CO2 incubator. When the cells were cultured
to 90% confluency, they were treated using 0.25% trypsin for 2–3
min at 37°C and seeded on a 6-well plate at a density of
1×105/well. After overnight culture in the
aforementioned conditions, cells were grouped and treated to
generate the HK-2 cell ferroptosis model and intervention as
follows: i) Control group; ii) erastin (ferroptosis inducer) group
(10 µmol/l erastin); iii) RSL3 (ferroptosis inducer) group (0.1
µmol/l RSL3) (10); iv) erastin +
RGSH group (10 µmol/l erastin for 24 h then 10 mmol/l RGSH was
added); and v) RSL3 + RGSH group (0.1 µmol/l RSL3 for 24 h then 10
mmol/l RGSH was added) (11).
Mouse AKI model
The animal use plan was approved by the Animal Care
and Use Committee of Jiaxing Second Hospital (approval no.
20200713-2). The specific pathogen free BALB/c mice (n=30) were
purchased from Beijing Vital River Laboratory Animal Technology
Co., Ltd. Same sex litter mates were housed together in
individually ventilated cages with two or four mice/cage. During
the whole duration of the experiment (7 days), all mice were
maintained on a regular diurnal 12 h light/dark cycle with ad
libitum access to food and water. The study was performed
strictly according to The Guide for Care and Use of Laboratory
Animals formulated by National Institutes of Health. The
researchers monitored animals twice daily. Health was monitored by
weight (twice weekly), food and water intake, and general
assessment of animal activity. Humane endpoints to help minimize
harm, complied with the humane standards of the American Veterinary
Medical Association (12),
including the mice showed an inability to feed and drink on their
own, weight loss of >20% of their starting body weight, were
clearly depressed in the absence of anesthesia, did not respond to
shouts of repulsion, were unable to move freely, or their body
temperature was consistently below 37°C. A total of eighteen mice
(male; age, 6–8 weeks) were randomly divided into the control
group, model group and RGSH group (n=6).
Anesthesia was administered intraperitoneally using
sodium pentobarbital (50 mg/kg). The depth of anesthesia was
assessed for ~5 min and mice were placed immediately on a 37°C
thermostatic heating pad. After the mice were anesthetized, an
incision of 1.5-2.0 cm was cut along the midline of the abdomen,
and the skin and peritoneum were separated layer by layer. After
entering the abdominal cavity, the left and right renal pedicles
were quickly blocked using non-invasive micro-arterial clips. A
change in the color of the kidneys from bright red to purple-black,
indicated that clipping was successful. After 45 min of clipping,
the arterial clip was removed, and blood perfusion was restored. At
this point, the kidneys quickly changed from purple-black to bright
red, returning to their original color. After the operation, the
abdominal cavity was closed by layered suture. The overall duration
of the experiment was limited to 60 min. A total of 1 h after
successful modeling, the mice in the RGSH group received an
intraperitoneal injection of 800 mg/kg RGSH (13) and the mice in the other two groups
were administered an equal volume of normal saline, this was
repeated for 6 consecutive days. After the operation, the mice were
kept warm at 24–29°C, and provided with water and feed. At the end
of the experimental period, the mice were anesthetized using 50
mg/kg sodium pentobarbital, and the orbital blood was collected and
stored at 4°C overnight. Mice were euthanized by cervical
dislocation and death was verified by absence of heartbeat and
pupil dilation. The kidneys were collected after euthanasia and
after stripping off the capsule, part of the tissues were fixed
using 10% formalin at 45°C for 1 h and embedded in paraffin. RNA
and protein were extracted from the remaining tissues.
Detection of BUN and malondialdehyde
(MDA) levels
The collected blood was centrifuged at 1,006 × g for
10 min at room temperature, and then, the serum was transferred
into a new Eppendorf tube. The MDA and BUN levels were quantified
using the BUN Detection research-use-only kit (cat. no. EIABUNX10;
Invitrogen; Thermo Fisher Scientific, Inc.) and MDA Assay Kit
(competitive ELISA) (cat. no. ab238537; Abcam) according to the
manufacturers protocols.
Staining and immunohistochemistry
(IHC)
The fixed, paraffin embedded kidney tissues were cut
into 5 µm thick sections. After baking (68°C), the slices were
dewaxed with xylene and rehydrated with ethanol in a descending
alcohol series. Then, hematoxylin and eosin (H&E) staining and
Prussian blue staining were performed according to the
manufacturer's protocol, an optical microscope (Nikon Corporation)
was used for observation and imaging, and ImageJ 2.0.0 (National
Institutes of Health) was used for analysis.
The protein expression levels of ACSL4 and GPX4 in
the kidney were assessed using immunohistochemistry. After
dewaxing, rehydration and antigen retrieval according to the
aforementioned method, the sample was endogenous peroxidase
activity was quenched using 3% hydrogen peroxide solution and the
sections were blocked using 5% bovine serum albumin (Roche
Diagnostics GmbH) for 10 min at room temperature. Sections were
incubated with primary antibodies against ACSL4 (1:200; cat. no.
PA5-30026; Invitrogen; Thermo Fisher Scientific, Inc.) and GPX4
(1:200; cat. no. PA5-10251; Invitrogen; Thermo Fisher Scientific,
Inc.) overnight at 4°C. The sections were then washed with PBS, and
incubated with Goat anti-Rabbit IgG (H+L) Secondary Antibody (cat.
no. 31210; Invitrogen; Thermo Fisher Scientific, Inc.) for 1 h at
room temperature. After washing the sample, DAB color development
was performed for 45 s. Sections were imaged using an optical
microscope (Nikon Corporation) with a ×400 objective, and the cells
with positive staining were quantified using ImageJ 2.0.0 (National
Institutes of Health).
Reverse transcription-quantitative PCR
(RT-qPCR)
Total RNA was extracted from the mouse kidney and
HK-2 cells using a column-type animal tissue total RNA extraction
and purification kit (Sangon Biotech Co., Ltd.), and then reverse
transcribed to synthesize complementary DNA using a PrimeScript™ RT
Reagent Kit with gDNA Eraser Kit (Takara Bio, Inc.). qPCR was
performed using the TB Green® Premix Ex TaqTM II Kit
(Takara Bio, Inc.), with GAPDH as the control gene. The thermal
program included the following melting curve steps: 10 min at 95°C
for 1 cycle, followed by 40 cycles for 10 sec at 95°C, 20 sec at
60°C and 15 sec at 72°C, and then a gradual increase from 72°C to
95°C at 0.5°C per sec; the data were collected every 6 sec. Changes
in the mRNA expression levels were calculated using the
2−ΔΔCq method (14).
All experiments were performed according to the manufacturer's
protocols, and the primer sequences used were presented in Table I.
 | Table I.Sequences of the primers used for
reverse transcription-quantitative PCR. |
Table I.
Sequences of the primers used for
reverse transcription-quantitative PCR.
| Gene | Sequence (5′-3′) |
|---|
| m-GPX4 | F:
GTGGAAATGGATGAAAGTC |
|
| R:
AGCCGTTCTTATCAATGA |
| h-GPX4 | F:
TGTGGAAGTGGATGAAGA |
|
| R:
ATGAGGAACTGTGGAGAG |
| m-ACSL4 | F:
CTTCCTCTTAAGGCCGGGAC |
|
| R:
TGCCATAGCGTTTTTCTTAGATTT |
| h-ACSL4 | F:
AAGTGAATCGCAGAGTGAATA |
|
| R:
AGAAGATGGCAATGGTGTT |
| m-GAPDH | F:
TGTGTCCGTCGTGGATCTGA |
|
| R:
TTGCTGTTGAAGTCGCAGGAG |
| h-GAPDH | F:
GAAGGCTGGGGCTCATTT |
|
| R:
CAGGAGGCATTGCTGATGAT |
Western blotting
Total protein from the kidneys and HK-2 cells in
each group collected using RIPA buffer (Thermo Fisher Scientific,
Inc.), and the protein content was determined using the BCA method.
SDS-PAGE gel electrophoresis was performed, equal amounts of
protein (40 µg) were separated on 10% gels using SDS-PAGE and the
samples were then transferred to polyvinylidene fluoride membranes.
The membranes were blocked with 3% skimmed milk at room temperature
for 1 h, and incubated with primary antibodies against ACSL4
(1:1,000; cat. no. PA5-30026), GPX4 (1:1,000; cat. no. PA5-10251)
and GAPDH (1:5,000; cat. no. MA1-16757) (all Invitrogen; Thermo
Fisher Scientific, Inc.) overnight at 4°C. Membranes were washed
using TBST [50 mmol/l Tris-HCl (pH 8.0), 150 mmol/l NaCl, and 0.1%
Tween-20] then incubated with HRP-conjugated goat anti-rabbit IgG
(H+L) secondary antibodies (1:2,000; cat. no. 31460; Invitrogen;
Thermo Fisher Scientific, Inc.) at room temperature for 1 h.
Finally, the color was developed using ECL supersensitive
luminescent solution (Thermo Fisher Scientific, Inc.), and images
were collected and analyzed using a Bio-Rad Gel Doc XR+ imaging
system (Bio-Rad Laboratories, Inc.).
Cell viability assay
HK-2 cells were seeded in the 96-well plate at a
density of 1.5×103 cells/well. After 48 h of culture (at
37°C in a 5% CO2 incubator), the CCK-8 working solution
was added to the sample and incubated for 1 h. The absorbance of
the cells in the wells was then measured at 490 nm using the
Multiskan Sky Microplate Spectrophotometer (Thermo Fisher
Scientific, Inc.) to evaluate the cell viability.
Detection of apoptosis by flow
cytometry
HK-2 cells were seeded into a 6-well plate and the
number of cells was adjusted to ~1×105 after
trypsinization. Samples were then centrifuged at 200 × g at room
temperature for 5 min, the supernatant was discarded, and the cells
were resuspended in PBS. A total of 5 µl of Annexin V-FITC and 5 µl
of propidium iodide were added to each well, were mixed by
pipetting, and incubated at room temperature in the dark for 15
min. The samples were then assessed using MACSQuant Analyzer 16
(Miltenyi Biotec GmbH) and data analyses were processed using
FlowJo v10.6.2 software (FlowJo, LLC).
Statistical methods
The statistical analysis was conducted using
GraphPad Prism 9 (Graphpad Software; Dotmatics). All data are
presented as the mean ± standard deviation. Differences between
groups were statistically analyzed using one-way analysis of
variance and Tukey's post-hoc test. P<0.05 was considered to
indicate a statistically significant difference.
Results
RGSH can inhibit ferroptosis in mice
with AKI
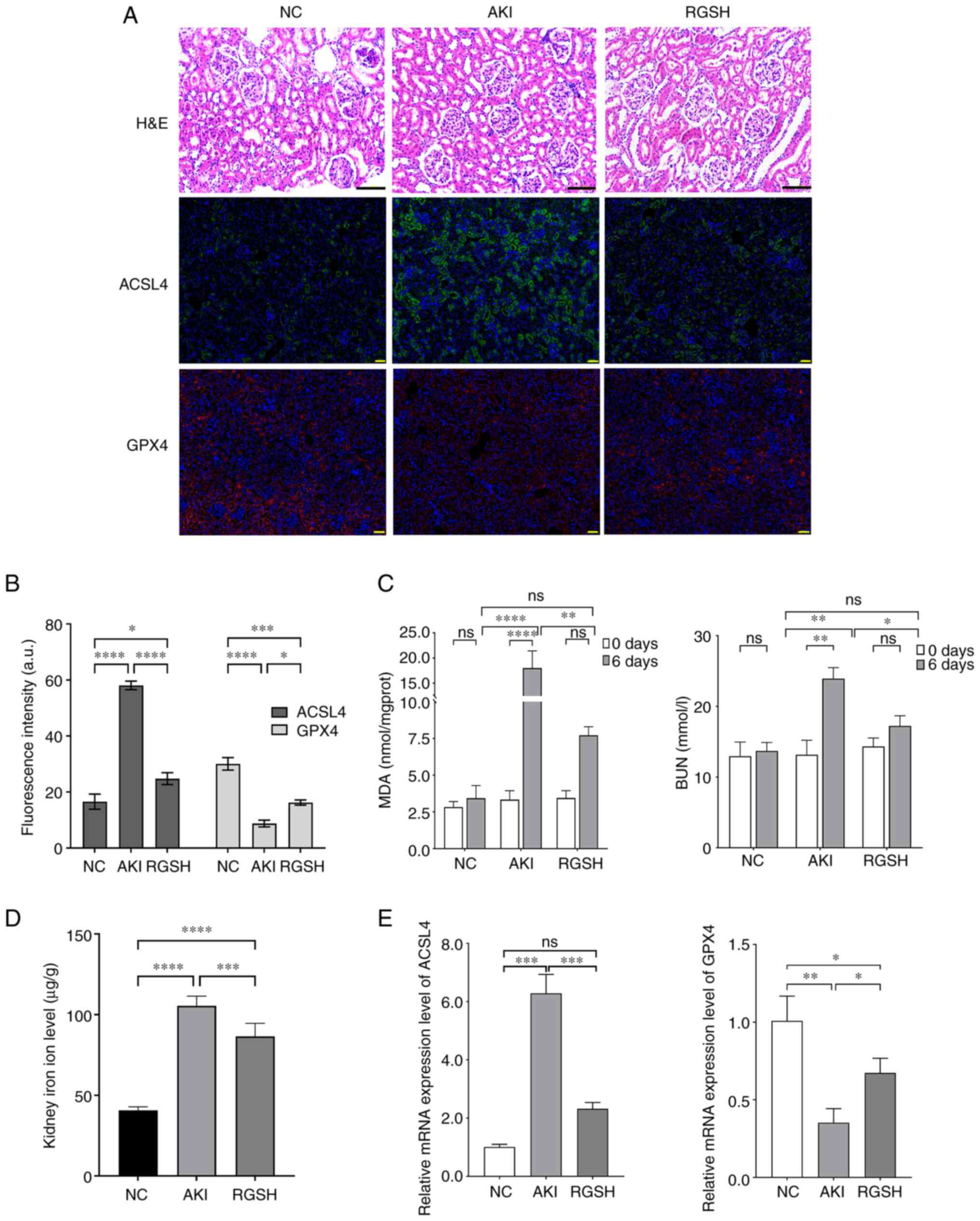
The H&E staining results of the renal tubular
epithelial cells in the mice in the AKI model group demonstrated
massive atrophy and necrosis, the tubular space was widened, and
the kidney structure was severely damaged. The glomerular damage in
mice in the RGSH group was alleviated and the level of renal
structural damage was reduced. The IHC results demonstrated that
ACSL4 protein expression levels increased markedly, and GPX4
protein expression levels decreased markedly in the AKI model group
compared with the control group. However, the ACSL4 protein
expression levels were markedly decreased and the GPX4 protein
expression levels were markedly increased in the RGSH group
compared with the AKI model group (Fig. 1A and B). The BUN and MDA levels of
mice in different groups was assessed. Compared with the control
group, the BUN and MDA levels in the AKI model group were markedly
increased, whereas the BUN and MDA levels in the RGSH group were
markedly lower than that of the AKI model group, which indicated
recovery (Fig. 1C). The level of
iron ions in the glomerulus of mice in the model group was
significantly higher than that in the control group, whereas the
iron ion level in the RGSH group was significantly lower than that
in the AKI model group. (Fig. 1D).
The mRNA expression levels of ACSL4 and GPX4, assessed using
RT-qPCR were consistent with the IHC results. The mRNA expression
level of ACSL4 increased significantly and the mRNA expression
level of GPX4 decreased significantly in the AKI group compared
with the control; however, the mRNA expression level of ACSL4
decreased significantly and the mRNA expression level of GPX4
increased significantly in the RGSH group compared with the AKI
group (Fig. 1E). These results
demonstrated that the acute kidney injury induces ferroptosis in
the renal cells and that RGSH ameliorated this process.
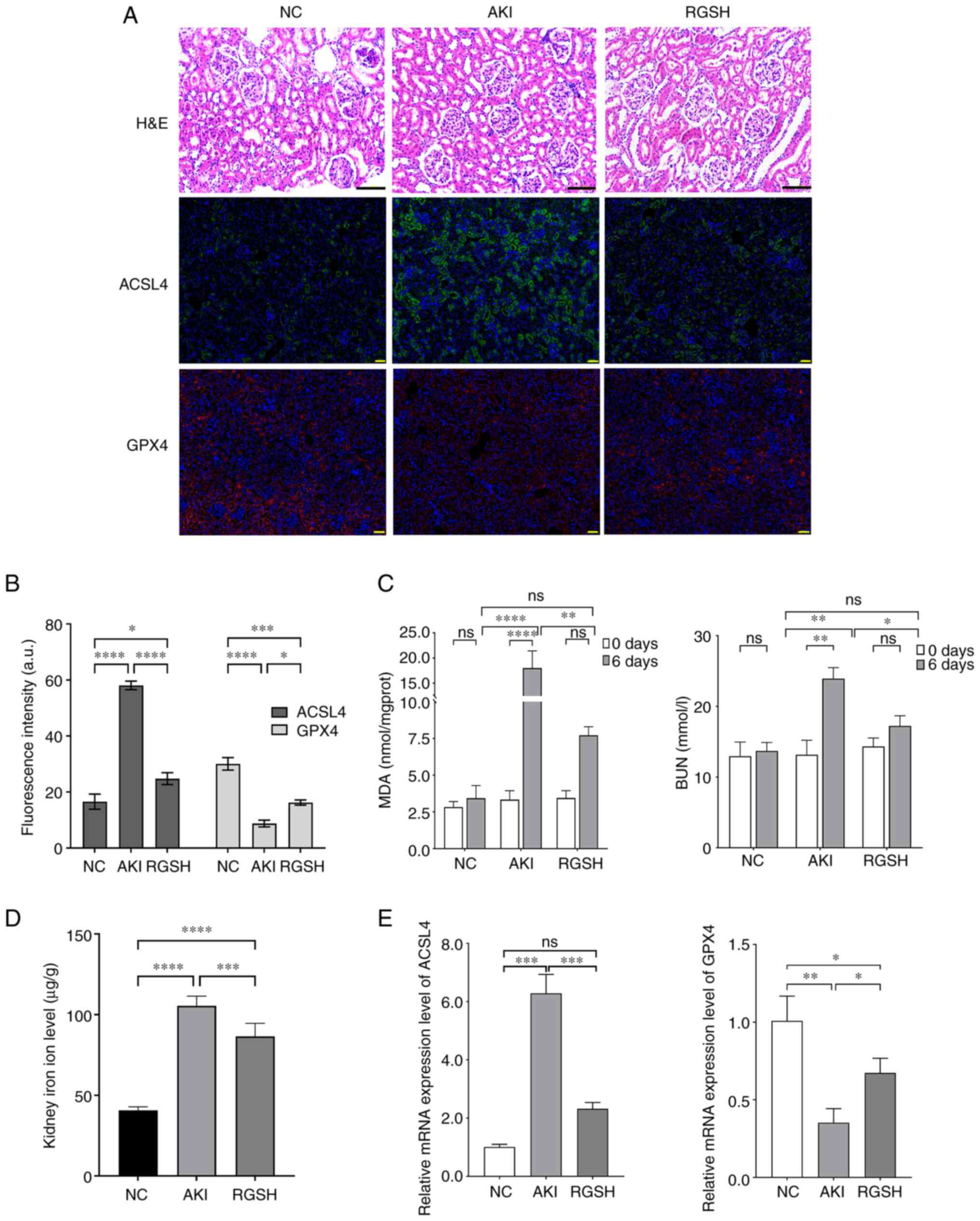 | Figure 1.Detection of mouse AKI indexes. (A)
Renal injury in the glomeruli of mice in various groups assessed
using H&E staining and the protein expression of ACSL4 and GPX4
in the mouse kidney in different groups according assessed using
immunohistochemical staining. (B) The fluorescence intensity of
ACSL4 or GPX4-expressing region in immunofluorescence (Fig. 1A) was calculated using ImageJ
software. (C) BUN and MDA levels of mice in different groups. (D)
Iron ion level in the glomeruli of mice in various groups. (E) mRNA
expression levels of ACSL4 and GPX4 assessed using reverse
transcription-quantitative PCR. Scale bars: H&E, 100 µm; IHC,
50 µm. *P<0.05, **P<0.01 and ***P<0.001. AKI, acute kidney
injury; ACSL4, acyl-CoA synthetase long-chain family member 4; BUN,
blood urea nitrogen; GPX4, glutathione peroxidase; H&E,
hematoxylin and eosin; MDA, malondialdehyde; NC, negative control;
RGSH, reduced glutathione; ns, not significant. |
RGSH can inhibit ferroptosis induced
by ferroptosis inducers erastin and RSL3 in HK-2 cells
A HK-2 cell ferroptosis model was constructed using
erastin and RSL3. The flow cytometry results demonstrated that the
RGSH intervention could markedly reduce cell death caused by
ferroptosis (Fig. 2A). The
statistical comparison of apoptosis rate is shown in Fig. 2B. The results of cell viability
experiments demonstrated that cell viability in the erastin and
RSL3 model groups were significantly reduced compared with the
control. After RGSH intervention, the cell viabilities were
significantly enhanced and markedly recovered (Fig. 2C). Furthermore, RGSH intervention
also significantly alleviated the reduction in lipid oxide levels
caused by ferroptosis inducers (Fig.
2D). These results indicated that RGSH could inhibit the
ferroptosis of HK-2 cells induced by the ferroptosis inducers
erastin and RSL3.
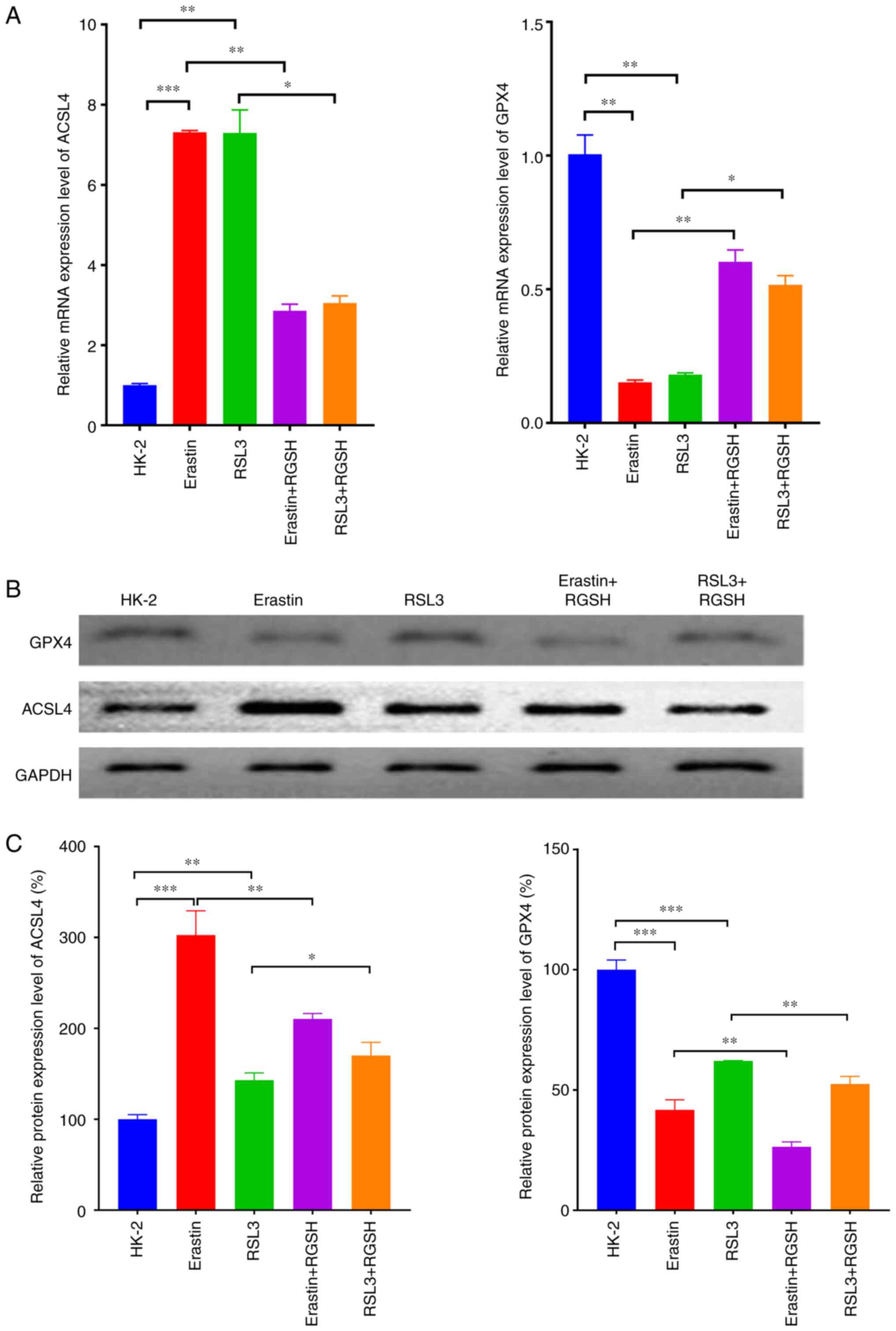
RGSH can inhibit ferroptosis through
the regulation of the levels of ferroptosis-related proteins
RT-qPCR was used to assess detect the mRNA
expression levels of the ferroptosis-related proteins ACSL4 and
GPX4 in HK-2 cells under certain treatments. In the model groups
which used erastin and RSL3 to induce ferroptosis, the mRNA
expression level of ACSL4 increased significantly and the mRNA
expression level of GPX4 decreased significantly compared with the
control. Compared with their respective model groups, in both the
erastin + RGSH and RSL3 + RGSH groups, the mRNA expression level of
ACSL4 decreased significantly and the mRNA expression level of GPX4
increased significantly (Fig. 3A).
The protein expression levels of ACSL4 and GPX4 semi-quantified
using western blotting were consistent with the RT-qPCR results
(Fig. 3B and C). These results
suggested that RGSH intervention could restore the changes in
ferroptosis-related proteins induced by the ferroptosis inducers,
thereby inhibiting ferroptosis.
Discussion
The damage to red blood cells during the
perioperative period can cause hemoglobin to escape and enter the
kidney through the blood circulation, which can lead to AKI.
Different degrees of renal damage affect the quality of life and
long-term prognosis of the patients (15,16).
When AKI occurs, the renal tubules are damaged and the glomerular
filtration rate drops sharply, which results in an increase in
serum creatinine and blood urea nitrogen (17). In the AKI mouse model built in
present study, the BUN and serum MDA levels markedly increased,
marked glomerular damage occurred and it was demonstrated that the
RGSH intervention could alleviate these effects, which demonstrated
the protective effect of RGSH in AKI.
Ferroptosis is widely present in a number of cells
types and regulates numerous pathological processes, including
those involved in certain neurodegenerative diseases (such as
Alzheimer's disease), tumors, stroke and traumatic brain injury
(18–21). Ferroptosis affects the occurrence
and development of AKI (8,22). Therefore, attenuation of
ferroptosis could be an important strategy to ameliorate AKI. The
expression levels of ferroptosis-related factors, including lipid
oxides, iron ions, ACSL4 and GPX4, are closely related to the
degree of ferroptosis in AKI (23–26).
The present study demonstrated that when AKI occurred, the iron ion
level in the renal tissues increased significantly, the mRNA
expression level of ACSL4 increased significantly and the mRNA
expression level of GPX4 decreased significantly, which indicated
the occurrence of ferroptosis in the kidney.
Previous studies have reported that RGSH can inhibit
oxidative stress and thus alleviate liver damage (27), and improve renal function in
patients by reducing the serum creatinine levels (28). A study has also reported that RGSH
can effectively eliminate oxygen free radicals and treat the AKI
rats with ischemia reperfusion (29). These studies suggested that RGSH
served a protective role for the body through its redox function.
In the present study, RGSH reduced the level of iron ions and ACSL4
in AKI, and increased the expression of GPX4, thereby reducing the
degree of kidney damage, which demonstrated that RGSH could
ameliorate hemolytic AKI via regulation of the ferroptosis pathway,
which was consistent with the results of previous studies that RGSH
affects ferroptosis via regulation of the ferroptosis-related gene
GPX4 (30). In the in vitro
experiments, construction of the HK-2 cell ferroptosis model
demonstrated that RGSH could significantly increase cell viability
and significantly increase the lipid oxide level in cells, which
inhibited cell apoptosis. These results indicated that RGSH may
inhibit cell death through the ferroptosis signaling pathway and
exert a protective effect on AKI. However, the experiments in the
present study were not sufficient to completely elucidate the
underlying mechanisms of ferroptosis in AKI through molecular and
animal model experiments alone, and similarly RGSH intervention on
AKI is only a meaningful first experiment. Although the results of
the present study indicated that RGSH could improve the poor
outcomes of AKI by modulating the ferroptosis signaling pathway,
the mechanisms underlying the occurrence of ferroptosis in AKI have
not been evaluated in depth. We hypothesize that another major
cause of AKI is the release of hemoglobin from ruptured
erythrocytes following major open surgery (31); however, the use of hemoglobin
chloride for stimulating kidney injury does not accurately mimic
the features of open surgery. Further study is required to develop
the model of surgical AKI, including partial hepatectomy in
mice.
In conclusion, RGSH intervention can down-regulate
the renal ACSL4 mRNA expression level and up-regulate the GPX4 mRNA
expression level in the development of AKI, and reduce the lipid
oxide and iron ion levels, thereby reducing iron accumulation,
alleviating cell damage and ameliorating intraoperative AKI by
inhibiting ferroptosis. The protective effect of RGSH on AKI by
inhibiting ferroptosis provides a new therapeutic strategy, which
could guide the use of medication and the treatment of
perioperative AKI in the clinic.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LH performed the histological examination of the
kidney and YS performed the molecular biology experiments. LH wrote
the manuscript. LH and YS confirm the authenticity of all the raw
data. Both authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was performed strictly following
The Guide for Care and Use of Laboratory Animals formulated by
National Institutes of Health. The animal use plan was approved by
the Animal Care and Use Committee of Jiaxing Second Hospital
(approval no. 20200713-2).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hounkpatin H, Fraser S, Glidewell L,
Blakeman T, Lewington A and Roderick P: Predicting risk of
recurrent acute kidney injury: A systematic review. Nephron.
142:83–90. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Saadat-Gilani K and Zarbock A:
Perioperative renal protection. Curr Opin Crit Care. 27:676–685.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Calvert S and Shaw A: Perioperative acute
kidney injury. Perioper Med (Lond). 1:62012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Singbartl K and Kellum J: AKI in the ICU:
Definition, epidemiology, risk stratification, and outcomes. Kidney
Int. 81:819–825. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sul YH, Lee JY, Kim SH, Ye JB, Lee JS,
Yoon SY and Choi JH: Risk factors for acute kidney injury in
critically ill patients with torso injury: A retrospective
observational single-center study. Medicine (Baltimore).
100:e267232021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dixon S and Stockwell B: The role of iron
and reactive oxygen species in cell death. Nat Chem Biol. 10:9–17.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sha R, Xu Y, Yuan C, Sheng X, Wu Z, Peng
J, Wang Y, Lin Y, Zhou L, Xu S, et al: Predictive and prognostic
impact of ferroptosis-related genes ACSL4 and GPX4 on breast cancer
treated with neoadjuvant chemotherapy. EBioMedicine. 71:1035602021.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Carney E: Ferroptotic stress promotes the
AKI to CKD transition. Nat Rev Nephrol. 17:6332021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Park EJ, Dusabimana T, Je J, Jeong K, Yun
SP, Kim HJ, Kim H and Park SW: Honokiol protects the kidney from
renal ischemia and reperfusion injury by upregulating the
glutathione biosynthetic enzymes. Biomedicines. 8:3522020.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen H, Qi Q, Wu N, Wang Y, Feng Q, Jin R
and Jiang L: Aspirin promotes RSL3-induced ferroptosis by
suppressing mTOR/SREBP-1/SCD1-mediated lipogenesis in
PIK3CA-mutatnt colorectal cancer. Redox Biol. 55:1024262022.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xiao MD: J.X: Effect of reduced
glutathione on high glucose-induced reactive oxygen species,
nuclear factor-kappa B andosteopontin in human renal tubular
epithelial cells. Jiangsu Med J. 34:2008.
|
|
12
|
Leary SLU: W.; Anthony, R.; Cartner, S.;
Corey, D.; Grandin, T.; Greenacre, C.; Gwaltney-Bran, S.;
McCrackin, M.; Meyer, R.; Miller, D.; Shearer, J.; Yanong, R.;
Golab, G.;: Patterson-Kane E AVMA guidelines for the euthanasia of
animals: 2013 edition. 2013. https://www.avma.org/KB/Policies/Pages/Euthanasia-Guidelines.aspx
|
|
13
|
Meng XZ: Ni; Zhang, Min; Song, Xuexia;
Liu, Qian; Huang, Xiangyan: Effect of reduced Glutathione onserum
and urinary concentration of NGAL in the rodent model of Cisplatin
induced acute kidney injur. China J Modern Med. 24:2014.
|
|
14
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Goren O and Matot I: Perioperative acute
kidney injury. Br J Anaesth. 115 (Suppl 2):ii3–ii14. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kim-Campbell N, Gretchen C, Callaway C,
Felmet K, Kochanek PM, Maul T, Wearden P, Sharma M, Viegas M, Munoz
R, et al: Cell-free plasma hemoglobin and male gender are risk
factors for acute kidney injury in low risk children undergoing
cardiopulmonary bypass. Crit Care Med. 45:e1123–e1130. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liu D, Zhang C, Hu M and Su K:
Scutellarein relieves the death and inflammation of tubular
epithelial cells in ischemic kidney injury by degradation of COX-2
protein. Int Immunopharmacol. 101:1081932021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lane D, Metselaar B, Greenough M, Bush A
and Ayton S: Ferroptosis and NRF2: An emerging battlefield in the
neurodegeneration of Alzheimer's disease. Essays Biochem.
65:925–940. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xiong R, He R, Liu B, Jiang W, Wang B, Li
N and Geng Q: Ferroptosis: A new promising target for lung cancer
therapy. Oxid Med Cell Longev. 2021:84575212021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li C, Sun G, Chen B, Xu L, Ye Y, He J, Bao
Z, Zhao P, Miao Z, Zhao L, Hu J, You Y, Liu N, Chao H and Ji J:
Nuclear receptor coactivator 4-mediated ferritinophagy contributes
to cerebral ischemia-induced ferroptosis in ischemic stroke.
Pharmacol Res. 174:1059332021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bao Z, Liu Y, Chen B, Miao Z, Tu Y, Li C,
Chao H, Ye Y, Xu X, Sun G, et al: Prokineticin-2 prevents neuronal
cell deaths in a model of traumatic brain injury. Nat Commun.
12:42202021. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang J, Liu Y, Wang Y and Sun L: The
cross-link between ferroptosis and kidney diseases. Oxid Med Cell
Longev. 2021:66548872021.PubMed/NCBI
|
|
23
|
Wang Y, Quan F, Cao Q, Lin Y, Yue C, Bi R,
Cui X, Yang H, Yang Y, Birnbaumer L, et al: Quercetin alleviates
acute kidney injury by inhibiting ferroptosis. J Adv Res.
28:231–243. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Martines A, Masereeuw R, Tjalsma H,
Hoenderop J, Wetzels J and Swinkels D: Iron metabolism in the
pathogenesis of iron-induced kidney injury. Nat Rev Nephrol.
9:385–398. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhao Z, Wu J, Xu H, Zhou C, Han B, Zhu H,
Hu Z, Ma Z, Ming Z, Yao Y, et al: XJB-5-131 inhibited ferroptosis
in tubular epithelial cells after ischemia-reperfusion injury. Cell
Death Dis. 11:6292020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chen C, Wang D, Yu Y, Zhao T, Min N, Wu Y,
Kang L, Zhao Y, Du L, Zhang M, et al: Legumain promotes tubular
ferroptosis by facilitating chaperone-mediated autophagy of GPX4 in
AKI. Cell Death Dis. 12:652021. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vairetti M, Di Pasqua L, Cagna M, Richelmi
P, Ferrigno A and Berardo C: Changes in glutathione content in
liver diseases: An update. Antioxidants (Basel). 10:3642021.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Santos NA, Bezerra CS, Martins NM, Curti
C, Bianchi ML and Santos AC: Hydroxyl radical scavenger ameliorates
cisplatin-induced nephrotoxicity by preventing oxidative stress,
redox state unbalance, impairment of energetic metabolism and
apoptosis in rat kidney mitochondria. Cancer Chemother Pharmacol.
61:145–155. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Han P, Qin Z, Tang J, Xu Z, Li R, Jiang X,
Yang C, Xing Q, Qi X, Tang M, et al: RTA-408 protects kidney from
ischemia-reperfusion injury in mice via activating Nrf2 and
downstream GSH biosynthesis gene. Oxid Med Cell Longev.
2017:76121822017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jia D, Zheng J, Zhou Y, Jia J, Ye X, Zhou
B, Chen X, Mo Y and Wang J: Ferroptosis is involved in hyperoxic
lung injury in neonatal rats. J Inflamm Res. 14:5393–5401. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zuk A and Bonventre JV: Acute kidney
injury. Annu Rev Med. 67:293–307. 2016. View Article : Google Scholar : PubMed/NCBI
|