Introduction
A number of pathological injuries, such as infection
and ischemia-reperfusion injury (I/R), are common in liver
transplantation and partial hepatectomy (1–3).
Furthermore, I/R is a common pathophysiological process (1). Liver parenchymal and non-parenchymal
cells undergo apoptosis or are lysed under ischemic and hypoxic
conditions, profoundly affecting the recovery of postoperative
liver function (1–3). Liver failure may be the outcome of
such severe damage, subsequently endangering the life of the
patient (1–4). The mechanisms underlying early I/R
injury include Küpffer cell activation, hepatocyte swelling and
hepatic microcirculation dysfunction, and liver sinusoidal
endothelial cells (LSECs) have an important role in regulating
hepatic microcirculation (5–11).
Extensive apoptosis and a loss of normal function due to I/R injury
may lead to further injury, apoptosis and disrupted liver
regeneration (5–7). Therefore, studying the specific
mechanism underlying hypoxia-reoxygenation (H-R) injury in LSECs is
important to reduce the incidence and severity of hepatic I/R
injury.
LSECs have a unique shape, including a very thin
cytoplasmic extension and a perforated membrane, termed
fenestration. Cells with normal fenestration are considered to be
in the differentiation state (12–14).
By contrast, a reduction in or abrogation of fenestration is termed
capillarization, and LSECs in the dedifferentiation state are
associated with hepatic stellate cell activation, liver fibrosis,
liver ischemia and hypoxia-effect aggravation (12–14).
LSECs with healthy fenestrae play a normal role, and therefore, it
is important to maintain the fenestration of LSECs to reduce liver
I/R injury and promote liver regeneration. The maintenance of LSEC
fenestration requires the participation of both paracrine and
autocrine cell signals (13).
Vascular endothelial growth factor (VEGF), which has a key role in
fenestration regulation, is mediated through nitric oxide
(NO)-dependent and NO-independent pathways (15,16).
VEGF may also prevent the capillarization of LSECs (16).
In our previous study, it was demonstrated that LESC
proliferation and fenestration maintenance is mediated by
regulation of the Sentrin/SUMO-specific protease 1
(SENP1)/hypoxia-inducible factor-1α (HIF-1α)/VEGF signaling axis
under hypoxic conditions (17).
The ubiquitin-specific proteases, SENPs, have an important function
in the posttranslational SUMO modification of proteins (17,18).
Furthermore, SENP1 is highly sensitive to hypoxia and can regulate
the stability of HIF-1α in the nucleus by desumoylation (17–19).
In addition, SENP1 and HIF-1α can promote the actions of each
other, forming a positive feedback loop and, through this feedback
loop, HIF-1α activates the expression of VEGF (17–19).
However, this adaptation of cells to hypoxia has only been
identified in the hepatic sinusoid (19), and whether this mechanism underlies
the effect mediated by LSECs in H-R injury to reduce damage is
unknown.
In the present study, it was found that LSECs
upregulated the expression of SENP1 and HIF-1α following H-R.
However, whether these proteins have a role in the H-R injury of
LSECs has not, to the best of our knowledge, been studied.
Therefore, the present study utilized mouse LSECs to construct an
in vitro H-R model to explore the relationship between SENP1
and LSEC H-R injury, and to explore the specific mechanism of
action to provide new targets for the clinical reduction of hepatic
I/R injury.
Materials and methods
Cell culture and establishment of an
LSEC H-R model
Mouse primary LSECs were purchased from iCell
Technologies, Inc. This company obtained LSECs from male C57BL/6
mice by digesting dissected liver tissue with elastase and
collagenase and then culturing the cells at 37°C with 5%
CO2 in primary endothelial cell culture medium (iCell
Bioscience, Inc.). In the present study, LSECs were inoculated in a
6-well culture plate and the culture medium was changed every 24 h.
When the cells reached 90% confluency in each well, H-R was
performed in a closed chamber at 37°C. For this, the cells were
cultured under anoxic conditions [a N2/CO2
(95:5) gas mixture] for 6 h and were then reoxygenated in an
air/CO2 (95:5) gas mixture for 24 h. The cells were
maintained in low serum (<5%) culture medium (iCell Bioscience,
Inc.). The cells in the control group were exposed to normoxia
[air/CO2 (95/5)] (20).
Reagents
Rabbit antibodies against SENP1 (cat. no. AF0275)
and HIF-1α (cat. no. AF1009) were purchased from Affinity
Biosciences. Rabbit antibodies against heme oxygenase (HO-1; cat.
no. ab189491), Bax (cat. no. ab32503), Bcl-2 (cat. no. ab182858),
cleaved-caspase-3 (cat. no. ab2302), β-actin (cat. no. ab8227) and
GAPDH (cat. no. ab9485) were purchased from Abcam. Goat anti-rabbit
HRP-conjugated secondary antibodies were purchased from Proteintech
Group, Inc. (cat. no. PR30012). Dimethyloxalylglycine (DMOG) was
purchased from MedChemExpress. Short interfering (si)-HIF-1α,
si-SENP1 and control oligonucleotides were synthesized by Shanghai
GenePharma Co., Ltd. These siRNAs were transfected into LSECs by
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.).
Experimental grouping and study
process
First, LSECs were randomly divided into two groups
for an in vitro study: A normoxic group (group A) and an H-R
group (group B). The cells in group B were further subdivided into
a control group, which was an H-R injury only group; a negative
control (NC) group, in which H-R cells were transfected with si-NC;
an si-SENP1 group, in which H-R cells were transfected with
si-SENP1; and an si-SENP1 + HIF-1α agonist rescue group, in which
H-R cells were transfected with si-SENP1 and then treated with an
HIF-1α agonist (DMOG). After 24 h of culture, the cells in each
group were analyzed using a scanning electron microscope to
determine the effect of H-R on LSEC fenestration. The apoptosis and
proliferation rates of the LSECs in each group were measured by
flow cytometry and Cell Counting Kit-8 (CCK-8) assay, respectively,
to study the effect of H-R on these processes. Furthermore, with an
identical procedure, the expression levels of SENP1, HIF-1α, VEGF,
HO-1, Bax, Bcl-2 and Caspase-3 in the normoxic and H-R groups were
measured.
Scanning electron microscopy
examination
After LSECs were seeded onto glass slides, the cells
were treated according to the experimental protocols, quickly fixed
with 3% glutaraldehyde at 4°C for 2 h and then stored at 4°C
overnight. Then, the cells were fixed in a 1% osmium tetroxide (pH
7.4) acetate buffer solution at 4°C for 1 h, dehydrated with a
series of ethanol solutions, dried in a critical-point device and
then plated onto gold in a vacuum coating device. The fenestration
of the cells in each experimental group was determined by
observation with a scanning electron microscope (SU8010; Hitachi,
Ltd.) with a 1.5 kV acceleration voltage and at ×60,000
magnification.
Cell viability determination by CCK-8
assay
The CCK-8 cell viability assay kit contains WST-8
[2-(2-methoxy-4-nitrophenyl)-3-(4-nitrophenyl)-5-(2rec-4-disulfophenyl)-2H-tetrazolium-monosodium
salt; CAS:193149-74-5]. In the presence of an electronic carrier,
WST-8 is reduced by intracellular dehydrogenase to form a
water-soluble orange methylene dye that can be dissolved in tissue
culture medium. The amount of dye produced is proportional to the
number of living cells. Therefore, CCK-8 method is a highly
sensitive and non-radioactive colorimetric method for determining
the number of living cells in cell proliferation experiments. An
LSEC suspension (100 µl of 5×103 cells/well) was
inoculated into a 96-well plate. When the confluency reached 70%,
the cells were cultured in DMEM/F12 without fetal bovine serum
(FBS) for 24 h. Then, the culture plate was incubated in an anoxic
or normoxic incubator and the medium was replaced with DMEM
containing FBS (iCell Bioscience, Inc.). The culture plates were
incubated (5 replicate wells for each time point) for the
appropriate time (specifically grouped according to the
experimental protocol). Then, 10 µl CCK-8 solution (from a CCK-8
detection kit; Peptide Institute, Inc.) was added to the medium and
incubated for 2 h. The absorbance was then measured at 450 nm using
an automatic microplate reader (EL309; BioTek; Agilent
Technologies, Inc.). All experiments were repeated at least three
times.
Detection of apoptosis by flow
cytometry
Apoptosis was analyzed using an Annexin V-FITC
Apoptosis Detection Kit (BD Biosciences). After treatment, the
cells were harvested and precipitated from the solution according
to the aforementioned experimental methods. Binding buffer (100 µl)
was added to each cell sample, and the samples were transferred to
a flow tube. Then, 10 µl propidium iodide and 5 µl Annexin V/FITC
solution was added to the cells and incubated at room temperature
for 15 min. Finally, 900 µl 0.01 M PBS (1X PBS) was added to each
cell sample before flow cytometry analysis. Apoptosis was measured
using a FACScan flow cytometer (BD Biosciences) and analyzed using
FlowJo software (version 10.0; FlowJo LLC). Apoptosis portion
(%)=Q2 (late stage apoptotic cells) + Q3 (early apoptotic
cells).
si-SENP1 transfection into LSECs
First, the cells were inoculated into culture
plates, and the target sequence (sense:
5′-GCAGUUCUGUGUAGCGAAATT-3′, antisense:
5′-UUUCGCUACACAGAACUGCTT-3′) with the highest transfection
efficiency and the appropriate transfection conditions (mass, 10
pmol; 37°C for 48 h) were established based on the manufacturer's
instructions. The negative control sequence was
5′-UUCUCCGAACGUGUCACGUTT-3′ and 5′-ACGUGACACGUUCGGAGAATT-3′. After
which, the transfected cells were divided into groups according to
the aforementioned experimental grouping, and stably transfected
cells were used in the primary and follow-up experiments. The time
interval between transfection and subsequent experimentation was
12–24 h.
Western blotting (WB)
The cells in each group were cultured under the
aforementioned normoxic or H-R conditions and then collected for WB
analysis. First, the proteins were extracted by
radioimmunoprecipitation assay RIPA lysis buffer (cat. no. P0013B)
and 1% PMSF (cat. no. ST506; both Beyotime Institute of
Biotechnology). The concentration of the total protein extracted
from each group was measured via the BCA method, according to the
manufacturer's instructions. The proteins (15 µl/lane; containing
25–40 µg of protein) were then denatured and separated in a 10%
sodium dodecyl sulfate-polyacrylamide gel and then transferred to a
polyvinylidene fluoride membrane. The membrane was blocked with 5%
skimmed milk for 2 h at room temperature and then incubated with
rabbit anti-SENP1 (1:2,000), rabbit anti-HIF-1α (1:2,000), rabbit
anti-GAPDH (1:3,000), rabbit anti-HO-1 (1:5,000), rabbit anti-Bax
(1:1,000), rabbit anti-Bcl-2 (1:1,000), rabbit anti-β-actin
(1:3,000) and rabbit anti-cleaved-caspase-3 (1:1,000) overnight at
4°C. After washing, a goat anti-rabbit HRP antibody (1:2,000) was
incubated with the membrane for 1 h at 37°C. Finally, the protein
bands were detected by the enhanced chemiluminescence method
(Life-ilab), and the relative protein levels were determined by
scanning densitometry analysis in Quantity One software (version
4.6; Bio-Rad Laboratories, Inc.) with GAPDH and β-actin as the
loading controls.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
After the cells were treated as aforementioned,
total RNA was extracted using TRIzol® (Invitrogen;
Thermo Fisher Scientific, Inc.) according to the manufacturer's
instructions. RT of ~2 µg of RNA into cDNA was performed using a
Prime Script RT kit (TransGen Biotech Co., Ltd.) according to the
manufacturer's protocol. qPCR analysis was then performed with a
Light Cycler Real-Time PCR System (LightCycler 480; Roche
Diagnostics; SYBR Green). The amplification procedure was as
follows: 95°C for 30 sec, 40 cycles at 95°C for 5 sec, 60°C for 30
sec and 72°C for 60 sec. The results were determined using the
2−ΔΔCq method (21) and
are expressed as the fold difference relative to the GAPDH level.
The primers used are shown in Table
I.
 | Table I.Primers used in reverse
transcription-quantitative polymerase chain reaction. |
Table I.
Primers used in reverse
transcription-quantitative polymerase chain reaction.
| Gene name
(mouse) | Forward primer
(5′-3′) | Reverse primer
(5′-3′) |
|---|
| SENP1 |
CTGGGGAGGTGACCTTAGTGA |
GTGATAATCTGGACGATAGGCTG |
| GAPDH |
AGTGGCAAAGTGGAGATT |
GTGGAGTCATACTGGAACA |
Enzyme-linked immunosorbent assays
(ELISAs)
The supernatant of the cultured cells was collected,
and the levels of VEGF (cat. no. MMV00), IL-6 (cat. no. M6000B) and
TNF-α (cat. no. MTA00B) were determined with commercial ELISA kits
(R&D Systems, Inc.). The sample was diluted five times, and all
the experiments were conducted according to the manufacturer's
instructions. Each experiment was repeated three times.
Statistical analysis
All data are presented as the average ± standard
deviation. The P-values were determined by Ordinary one-way ANOVA
(Tukey's multiple comparisons test), two-way ANOVA (Sidak's
multiple comparisons test) and unpaired t-tests. All analyses were
performed using Prism 8 (Dotmatics). P<0.05 was considered to
indicate a statistically significant difference.
Results
Expression of SENP1 in LSECs is
significantly upregulated following H-R
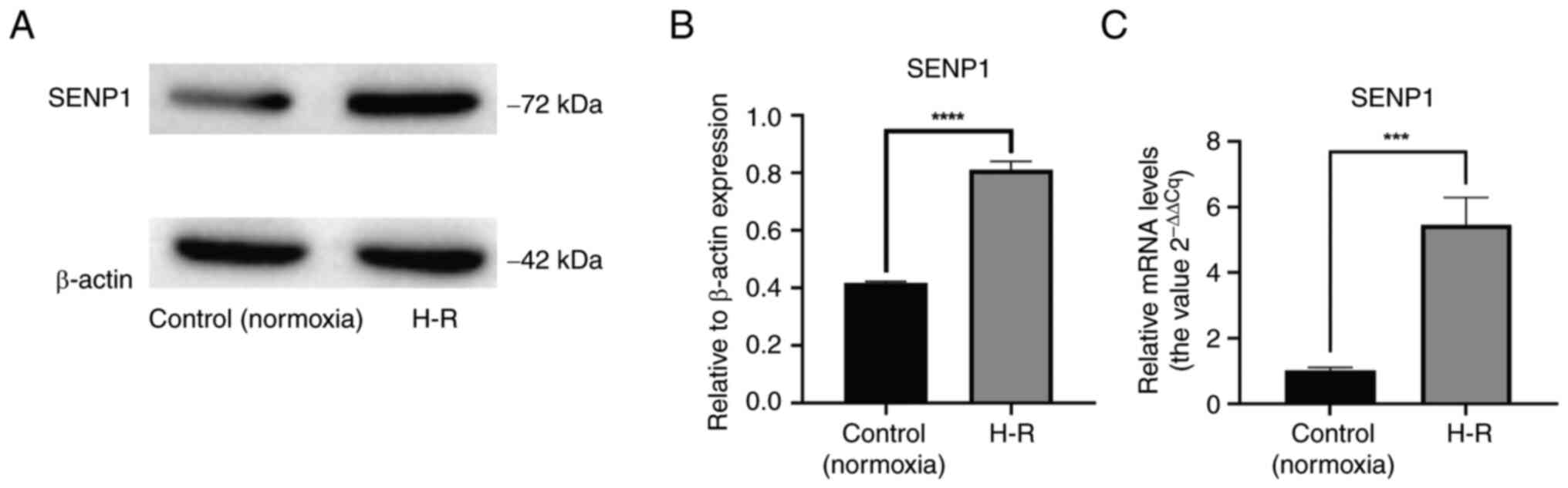
After the H-R LSEC model was established, it was
verified via RT-qPCR that the level of SENP1 mRNA in these LSECs
was significantly higher than that in the control (normoxic) cells
(P<0.001; Fig. 1C). Similarly,
it was demonstrated by WB that the protein expression level of
SENP1 in the H-R LSEC model was significantly higher than that in
the control (normoxic) cells (P<0.0001; Fig. 1A and B). From these results, it can
be suggested that SENP1 may be involved in the regulation of H-R
injury in LSECs.
Viability of LSECs is impaired and
fenestration damage is increased following H-R
To explore the phenotypic changes in primary mouse
LSECs following H-R injury, a CCK-8 assay was conducted to measure
cell viability. It was found that, compared with the control
(normoxic) group, the viability of the H-R injured LSECs decreased
significantly (P<0.0001; Fig.
2C).
To explore the effect of H-R on LSEC fenestration,
scanning electron microscopy was performed to identify fenestrated
cells. Compared with the control (normoxic) group, the fenestration
in the H-R injured cells was significantly damaged, with a
significant decrease in the number of fenestrated cells (P<0.05;
Fig. 2A and B). These results
suggested that the fenestration of LSECs decreased rapidly
following H-R, which accelerated cell dedifferentiation.
Apoptosis rate of LSECs is
significantly increased following H-R
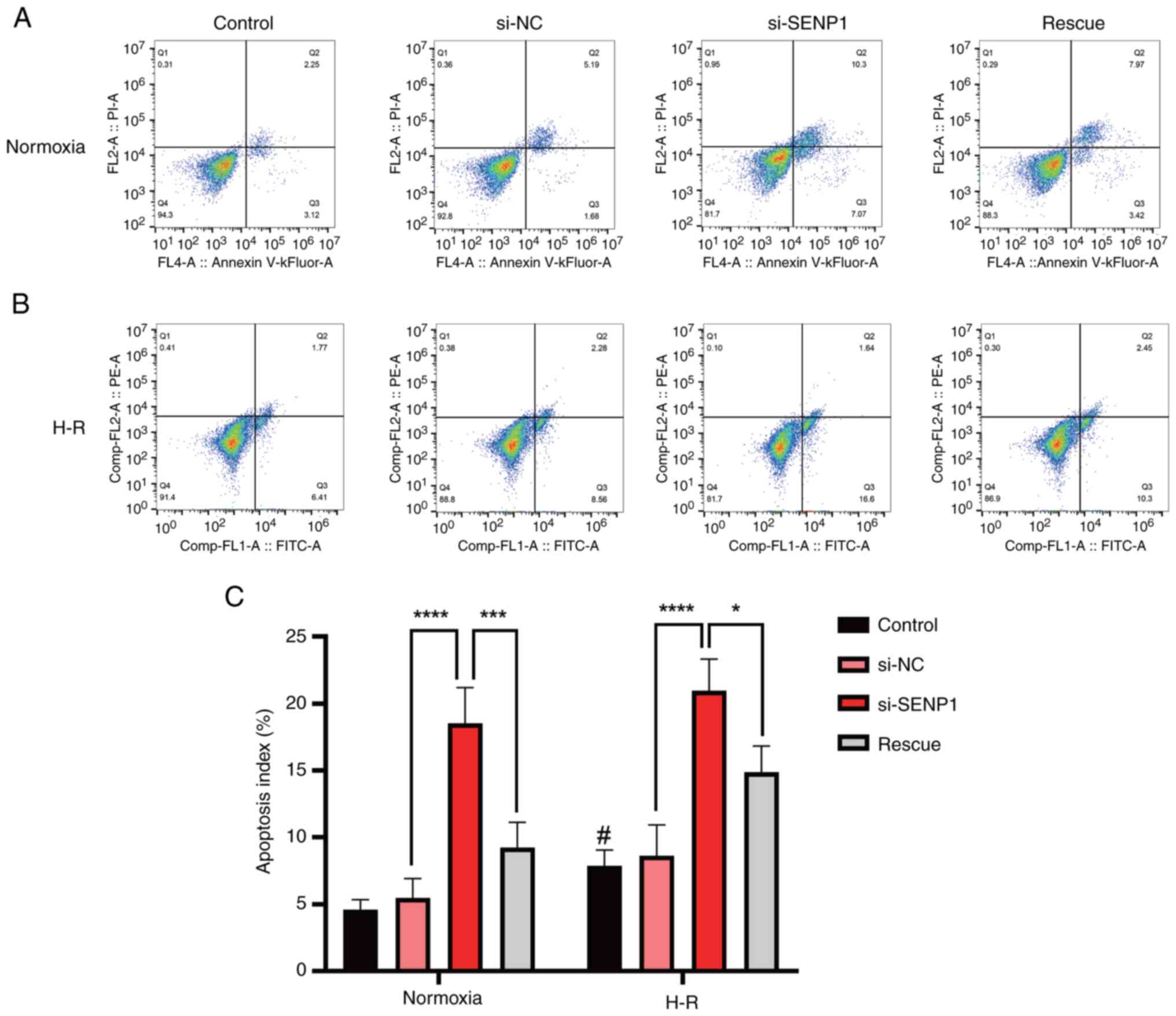
To explore the effect of H-R injury on primary mouse
LSEC apoptosis, the number of apoptotic cells was measured by flow
cytometry. It was found that the apoptosis rate of the H-R injured
cells was significantly higher than that of the control (normoxic)
group (Fig. 3A-C).
Silencing of SENP1 in H-R injured
LSECs decreases the proliferation rate and increases the extent of
fenestration damage and the apoptosis rate
To determine whether the phenotypic changes in LSECs
following H-R injury, such as the decrease in proliferation rate
and fenestration and the increase in apoptosis, were related to
changes in SENP1 protein expression, the SENP1 expression in LSECs
was silenced with siRNA. It was found that, compared with the
control group, after silencing SENP1 expression, the decrease in
the proliferation rate, the extent of diminished fenestration and
the increase in the apoptosis rate were all exacerbated. This
indicated that SENP1 may be involved in the regulation of LSEC
proliferation, fenestration and apoptosis after H-R exposure
(Figs. 2 and 3).
Following activation of the HIF-1α
signaling pathway, the reduction in LSEC fenestration and
proliferation rate is alleviated and the apoptosis rate is
decreased
After activating the HIF-1α signaling pathway with
the HIF-1α agonist, DMOG, the reduction in LSEC fenestration and
proliferation rate was significantly alleviated and the apoptosis
rate was significantly decreased (Figs. 2 and 3). These results suggested that SENP1 may
regulate LSEC fenestration maintenance, proliferation and apoptosis
after H-R exposure through the HIF-1α signaling pathway.
SENP1 attenuates the decrease in
proliferation rate, increase in apoptosis rate and damage to
fenestration in H-R injured LSECs through the HIF-1α signaling
pathway
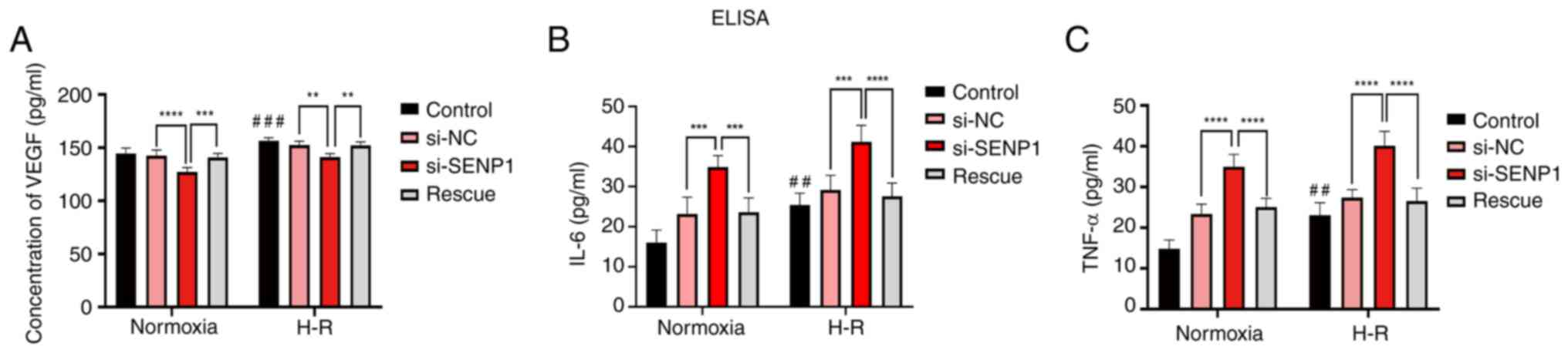
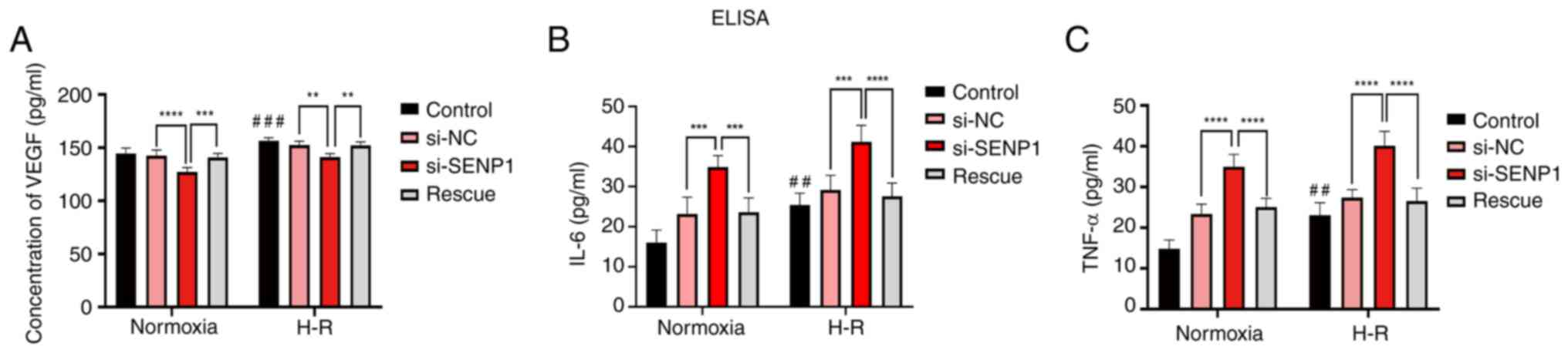
To further explore the specific mechanism by which
SENP1 regulated the proliferation, apoptosis and fenestration of
LSECs following H-R injury, SENP1 expression in LSECs was silenced
with siRNA. It was found that si-SENP1 not only decreased the SENP1
protein level but also decreased the expression of HIF-1α and HO-1,
increased the expression of apoptosis-related proteins,
cleaved-Caspase-3 and Bax, and decreased the expression of Bcl-2
(Fig. 4A-F). In addition, the
levels of VEGF, IL-6 and TNF-α in the cell culture medium were
determined by ELISA (Fig. 5). The
levels of IL-6 and TNF-α in the H-R group were significantly higher
than those in the control (normoxic) group. The concentration of
VEGF was also increased (Fig. 5).
However, compared with the si-NC group, the VEGF protein expression
level in the si-SENP1 group decreased significantly, while the
levels of IL-6 and TNF-α increased significantly (Fig. 5). However, after the HIF-1α
signaling pathway agonist, DMOG, was added to cells (the rescue
group), the results were the opposite of that following SENP1
silencing. In addition, the HIF-1α signaling pathway was
reactivated, attenuating the damage caused by H-R. This indicated
that silencing SENP1 may inhibit the effect of the HIF-1α signaling
pathway and subsequently aggravate the damage caused by H-R.
Specifically, these results suggested that SENP1 attenuated the
increase in apoptosis and fenestration impairments in LSECs
following H-R through the HIF-1α signaling pathway.
 | Figure 4.SENP1, HIF-1α, HO-1,
cleaved-caspase-3, Bax and Bcl-2 protein expression levels in
SENP1-knockdown H-R-injured liver sinusoidal endothelial cells. (A)
Representative western blots and ratio of SENP1, HIF-1α vs. GAPDH
expression determined from the western blot images in the normoxia
group. (B) Representative western blots and ratio of SENP1, HIF-1α
in the H-R group. (C) Representative western blots and ratio of Bax
and cleaved-caspase-3 in the normoxia group. (D) Representative
western blots and ratio of Bax and cleaved-caspase-3 in the H-R
group. (E) Representative western blots and ratio of Bcl-2 and HO-1
in the normoxia group. (F) Representative western blots and ratio
of Bcl-2 and HO-1 in the H-R group. Date were shown as the mean ±
SD (n=3); *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001
vs. the si-NC or si-SENP1 group. HIF-1α, hypoxia-inducible
transcription factor-1α; HO-1, heme oxygenase; NC, negative
control; SENP1, Sentrin/SUMO-specific protease 1; si(RNA), short
interfering RNA; H-R, hypoxia-reoxygenation. |
 | Figure 5.VEGF, IL-6 and TNF-α protein levels
in SENP1-knockdown hypoxia-reoxygenation-injured LSECs. (A) ELISA
of VEGF expression in all LSEC groups. (B and C) ELISAs of IL-6 and
TNF-α expression in all LSEC groups. Data were presented as the
mean ± SD (n=5); **P<0.01, ***P<0.001, ****P<0.0001 vs.
the si-NC or si-SENP1 groups; ##P<0.01,
###P<0.001 vs. the normoxic group. ELISA,
enzyme-linked immunosorbent assay; LSECs, liver sinusoidal
endothelial cells; NC, negative control; VEGF, vascular endothelial
growth factor; SENP1, Sentrin/SUMO-specific protease 1; si(RNA),
short interfering RNA. |
Discussion
Hepatic I/R injury is a common pathophysiological
outcome of liver transplantation and hepatectomy (1,2).
LSECs experience H-R injury, which proceeds through two different
stages (1,2). During the ischemic period, blood flow
to the liver is interrupted, resulting in tissue hypoxia, which
damages the normal function of mitochondria (1,2,22).
Specifically, the lack of oxygen delivered via electron carriers to
the end of the mitochondrial respiratory chain immediately
interrupts electron flow, resulting in reduced respiratory chain
output (22). The subsequent
interruption to oxidative phosphorylation leads to the rapid
depletion of ATP, the acceleration of glycolysis, an increase in
lactic acid production and a change in Ca2+ homeostasis,
which all exert damaging effects on LSECs, hepatocytes and other
liver cells (23). Although blood
flow to the liver is restored through reperfusion, the number of
inflammatory cells, pro-inflammatory mediators and reactive oxygen
species increases, exacerbating liver injury (24). Furthermore, damage to LSECs leads
to a lack of neovascularization in hyperplastic liver tissue and
the disruption of microcirculation in hepatic sinusoids,
exacerbating ischemic and hypoxic damage to hepatocytes and other
non-parenchymal cells (6). These
outcomes increase the hepatocyte apoptosis and necrosis rates,
eventually aggravating hepatic I/R injury and potentially inducing
liver failure (6). Therefore,
reducing H-R injury to LSECs would increase the stability of
microcirculation in the hepatic sinusoid environment and alleviate
I/R injury.
Previous studies have shown that LSECs not only
coordinate the response of the liver to injury but also mediate the
recovery of liver injury (2,12,13).
LSECs reduce the effect of I/R injury through autophagy, thus
ensuring normal cell function (25). Furthermore, LSECs with normal
function ensure liver regeneration and liver function recovery
following hepatectomy (12,13).
A number of mechanisms may regulate the activation of autophagy in
endothelial cells. A decrease in ATP or in the availability of
growth factors leads to the activation of AMP-activated protein
kinase (AMPK). Once activated, AMPK inhibits mTOR action, resulting
in the activation of unc-51 like autophagy activating kinase
(ULK1), which triggers autophagy. In endothelial cells,
calmodulin-dependent protein kinase-β-mediated AMPK activation
inhibits mTOR activity, resulting in the upregulation of ULK1 and
autophagy activation. Therefore, in endothelial cells, the
activation of autophagy involves the dynamic interaction between
AMPK, intracellular calcium, mTOR and ULK-1 (26,27).
However, when H-R injury is severe, LSECs show dysfunction, the
hepatic sinusoid microenvironment is subjected to ischemic and
hypoxic conditions, the number of inflammatory mediators increases
and reactive oxygen species accumulate (1,6,22).
The LSECs and hepatocytes then undergo necrosis or apoptosis and
liver regeneration is attenuated, making liver failure a likely
outcome (1,22). Therefore, reducing the damage to
LSECs caused by I/R injury promotes liver regeneration and liver
function recovery following hepatectomy.
Our previous study revealed that, under hypoxic
culture conditions, LSECs maintained fenestration and proliferated
via regulation of the SENP1/HIF-1α/VEGF signaling pathway (17,28).
Thus, SENP1 has been suggested to be involved in regulating the
maintenance of a healthy LSEC phenotype under hypoxic conditions,
assisting LSEC function in promoting liver regeneration. However,
during and after hepatectomy, the pathophysiological process of I/R
in hepatic sinusoids due to the disappearance of a hepatic artery
buffering effect and unbalanced proliferation of cells in the liver
during liver regeneration, leads to H-R injury to LSECs (29). The expression of SENP1 has been
reported to be upregulated in cardiomyocytes during H-R injury,
reducing H-R injury (30). Our
previous study confirmed that SENP1 expression was significantly
upregulated in hypoxia-treated LSECs and participated in the
regulation of LSEC proliferation and fenestration maintenance.
Therefore, it was hypothesized that SENP1 may be involved in
regulating the pathological process underlying H-R injury in
LSECs.
In the present study, using a mouse primary LSEC H-R
model, it was found that SENP1 expression in LSECs was
significantly upregulated at both the mRNA and protein levels
compared with the control group. These findings therefore indicated
that SENP1 expression in LSECs is affected by H-R. In addition, it
was found that the proliferation rate was reduced, fenestration
damage was increased and the apoptosis rate was increased in LSECs
cultured in H-R conditions. To explore whether these phenotypic
changes were related to changes in SENP1 expression, siRNA was used
to silence SENP1 expression in LSECs. It was demonstrated that,
compared with the control group, the reduction in viability was
more profound, fenestration damage was increased and the apoptosis
rate was increased in cells transfected with si-SENP1. This
indicated that SENP1 may be involved in the regulation of
viability, fenestration and apoptosis in LSECs exposed to H-R.
To further explore the specific mechanisms by which
SENP1 regulates the viability, apoptosis and fenestration of LSECs
following H-R, the expression levels of associated factors were
assessed. It was found that si-SENP1 transfection not only
decreased the protein level of SENP1 but also decreased the
expression of HIF-1α and HO-1, increased the expression of the
apoptosis-related proteins, caspase-3 and Bax, and decreased the
expression of Bcl-2. These results therefore revealed that
silencing SENP1 expression suppressed the HIF-1α signaling pathway,
increasing the activity of the intrinsic apoptosis pathway, and
thus increasing LSEC apoptosis. In addition, ELISAs were performed
to measure the levels of VEGF, IL-6 and TNF-α in the cell culture
medium. It was found that, compared with the control group, the
levels of VEGF, IL-6 and TNF-α were significantly increased in the
H-R group. However, compared with the H-R group, the protein
expression of VEGF was decreased, while the levels of IL-6 and
TNF-α were significantly increased in the group transfected with
si-SENP1. Studies (12–15) have demonstrated that VEGF
participated in maintaining LSEC differentiation and fenestration.
However, when LSECs were damaged by H-R, the expression of VEGF
increased, delaying the loss of fenestration. Moreover, after SENP1
silencing, the expression of VEGF decreased significantly, and the
loss of fenestration was more notable, indicating that SENP1
regulated the expression of VEGF in LSECs, which was similar to the
findings of our previous study (17). In the present study, IL-6, TNF-α
and other inflammatory mediator levels were found to be increased
in LSECs following H-R exposure, which was similar to previous
findings reported in the literature (20,31).
These findings suggested that the number of LSECs may increase due
to the increase in inflammatory factors that trigger the intrinsic
apoptosis pathway, thus explaining the increase in the LSEC
apoptosis rate following H-R injury.
However, the limitations of the present study should
be acknowledged. The experiments were conducted in vitro and
cannot truly reflect the complex internal environment in
vivo. Studies have shown that in vivo, VEGF is secreted
mainly by hepatocytes and hepatic stellate cells, which affect
LSECs through paracrine signaling (13,15).
The results of the present study demonstrated that LSECs
self-regulate fenestration via autocrine VEGF.
In addition, through the use of an HIF-1α signaling
pathway agonist, the outcomes of the aforementioned experiments
were reversed. Specifically, the inhibitory effect of si-SENP1 was
counteracted, indicating that silencing SENP1 expression may
inhibit the effect of the HIF-1α signaling pathway, aggravating the
damage caused by H-R. However, when a HIF-1α signaling pathway
agonist was used, the damage caused by H-R was alleviated.
Therefore, SENP1 may reduce the apoptosis rate and fenestration
damage in LSECs following H-R through the HIF-1α signaling
pathway.
In summary, after H-R treatment, the proliferation
rate was decreased, fenestration was inhibited, the apoptosis rate
increased and SENP1 expression was increased in LESCs. Moreover,
after SENP1 silencing, the expression of HIF-1α decreased and the
damage to LSECs was aggravated. However, the H-R injury of LSECs
was reversed when an HIF-1α signaling pathway agonist was used to
treat the cells. These findings indicated that SENP1 may alleviate
H-R injury to LSECs by mediating the effects of HIF-1α
signaling.
Acknowledgements
Not applicable.
Funding
This research was supported by the Scientific Research
Foundation Project of the Department of Science and Technology of
Yunnan Province (grant no. 202101AY070001-128) and the National
Natural Science Foundation of China (grant no. 81960124).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
ZQ, QL and ZZ designed the study. ZQ and QL
performed most of the data analysis, imaging and cell experiments.
QL and JD performed all scanning electron microscopy experiments.
QL performed the cell experiments. JD, JL, SY and HH collected and
analyzed the data. JL, SY and HH performed literature review. ZQ
and QL wrote the manuscript. ZZ and HH revised the manuscript. All
authors read and approved the final version of the manuscript. ZQ,
QL and ZZ confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
All experiments were conducted in accordance with
the National Institutes of Health Guide for the Care and Use of
Laboratory Animals and were approved by the Animal Ethics Committee
of the First Affiliated Hospital of Kunming Medical University
(Kunming, China; approval no. KMMU2020202).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
LSECs
|
liver sinusoidal endothelial cells
|
|
SENP1
|
Sentrin/SUMO-specific protease 1
|
|
HIF-1α
|
hypoxia-inducible transcription
factor-1α
|
|
VEGF
|
vascular endothelial growth factor
|
|
I/R
|
ischemia-reperfusion
|
|
H-R
|
hypoxia-reoxygenation
|
|
RT-qPCR
|
reverse transcription-quantitative
polymerase chain reaction
|
|
WB
|
western blotting
|
|
ELISA
|
enzyme-linked immunosorbent assay
|
References
|
1
|
Yang W, Chen J, Meng Y, Chen Z and Yang J:
Novel targets for treating ischemia-reperfusion injury in the
liver. Int J Mol Sci. 19:13022018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Selzner N, Rudiger H, Graf R and Clavien
PA: Protective strategies against ischemic injury of the liver.
Gastroenterology. 125:917–936. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dar WA, Sullivan E, Bynon JS, Eltzschig H
and Ju C: Ischaemia reperfusion injury in liver transplantation:
Cellular and molecular mechanisms. Liver Int. 39:788–801. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Russo L, Gracia-Sancho J, García-Calderó
H, Marrone G, García-Pagán JC, García-Cardeña G and Bosch J:
Addition of simvastatin to cold storage solution prevents
endothelial dysfunction in explanted rat livers. Hepatology.
55:921–930. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Peralta C, Jiménez-Castro MB and
Gracia-Sancho J: Hepatic ischemia and reperfusion injury: Effects
on the liver sinusoidal milieu. J Hepatol. 59:1094–1106. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hide D, Warren A, Fernandez-Iglesias A,
Maeso-Diaz R, Peralta C, Le Couteur DG, Bosch J, Cogger VC and
Gracia-Sancho J: Ischemia/reperfusion injury in the aged liver: The
importance of the sinusoidal endothelium in developing therapeutic
strategies for the elderly. J Gerontol A Biol Sci Med Sci.
75:268–277. 2020.PubMed/NCBI
|
|
7
|
Wang X, Walkey CJ, Maretti-Mira AC, Wang
L, Johnson DL and DeLeve LD: Susceptibility of Rat steatotic liver
to ischemia-reperfusion is treatable with liver-selective matrix
metalloproteinase inhibition. Hepatology. 72:1771–1785. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Stolz DB, Ross MA, Ikeda A, Tomiyama K,
Kaizu T, Geller DA and Murase N: Sinusoidal endothelial cell
repopulation following ischemia/reperfusion injury in rat liver
transplantation. Hepatology. 46:1464–1475. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Caldwell-Kenkel JC, Currin RT, Tanaka Y,
Thurman RG and Lemasters JJ: Reperfusion injury to endothelial
cells following cold ischemic storage of rat livers. Hepatology.
10:292–299. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hui AM, Kawasaki S, Makuuchi M, Nakayama
J, Ikegami T and Miyagawa S: Liver injury following normothermic
ischemia in steatotic rat liver. Hepatology. 20:1287–1293. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jawad R, D'Souza M, Selenius LA, Lundgren
MW, Danielsson O, Nowak G, Björnstedt M and Isaksson B:
Morphological alterations and redox changes associated with hepatic
warm ischemia-reperfusion injury. World J Hepatol. 9:1261–1269.
2007. View Article : Google Scholar
|
|
12
|
DeLeve LD: Liver sinusoidal endothelial
cells and liver regeneration. J Clin Invest. 123:1861–1866. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
DeLeve LD, Wang X, Hu L, McCuskey MK and
McCuskey RS: Rat liver sinusoidal endothelial cell phenotype is
maintained by paracrine and autocrine regulation. Am J Physiol
Gastrointest Liver Physiol. 287:G757–G763. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
DeLeve LD and Maretti-Mira AC: Liver
sinusoidal endothelial cell: An update. Semin Liver Dis.
37:377–387. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Funyu J, Mochida S, Inao M, Matsui A and
Fujiwara K: VEGF can act as vascular permeability factor in the
hepatic sinusoids through upregulation of porosity of endothelial
cells. Biochem Biophys Res Commun. 280:481–485. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xie G, Wang X, Wang L, Wang L, Atkinson
RD, Kanel GC, Gaarde WA and Deleve LD: Role of differentiation of
liver sinusoidal endothelial cells in progression and regression of
hepatic fibrosis in rats. Gastroenterology. 142:918–927.e6. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Qing Z, Huang H, Yang S, Lin J, Zeng Z,
Duan J, Yuan B and Ming T: Hypoxia maintains the fenestration of
liver sinusoidal endothelial cells and promotes their proliferation
through the SENP1/HIF-1α/VEGF signaling axis. Biochem Biophys Res
Commun. 540:42–50. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cheng J, Kang X, Zhang S and Yeh ET:
SUMO-specific protease 1 is essential for stabilization of
HIF1alpha during hypoxia. Cell. 131:584–695. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cui CP, Wong CCL, Kai AKL, Ho DWH, Lau
EYT, Tsui YM, Chan LK, Cheung TT, Chok KSH, Chan ACY, et al: SENP1
promotes hypoxia-induced cancer stemness by HIF-1α deSUMOylation
and SENP1/HIF-1α positive feedback loop. Gut. 66:2149–2159. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Qu S, Yuan B, Zhang H, Huang H, Zeng Z,
Yang S, Ling J, Jin L and Wu P: Heme oxygenase 1 attenuates
hypoxia-reoxygenation injury in mice liver sinusoidal endothelial
cells. Transplantation. 102:426–432. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Saidi RF and Kenari SKH: Liver
ischemia/reperfusion injury: An overview. J Invest Surg.
27:366–379. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gasbarrini A, Borle AB, Farghali H, Bender
C, Francavilla A and Van Thiel D: Effect of anoxia on intracellular
ATP, Na+i, Ca2+i, Mg2+i, and cytotoxicity in rat hepatocytes. J
Biol Chem. 267:6654–6663. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cannistrà M, Ruggiero M, Zullo A, Gallelli
G, Serafini S, Maria M, Naso A, Grande R, Serra R and Nardo B:
Hepatic ischemia reperfusion injury: A systematic review of
literature and the role of current drugs and biomarkers. Int J
Surg. 33 (Suppl 1):S57–S70. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Høyer-Hansen M and Jäättelä M:
AMP-activated protein kinase: A universal regulator of autophagy?
Autophagy. 3:381–383. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kim HS, Montana V, Jang HJ, Parpura V and
Kim JA: Epigallocatechin gallate (EGCG) stimulates autophagy in
vascular endothelial cells: A potential role for reducing lipid
accumulation. J Biol Chem. 288:22693–22705. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ghislat G, Patron M, Rizzuto R and Knecht
E: Withdrawal of essential amino acids increases autophagy by a
pathway involving Ca2+/calmodulin-dependent kinase kinase-β
(CaMKK-β). J Biol Chem. 287:38625–38636. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Qing Z, Huang H, Luo Q, Lin J, Yang S, Liu
T, Zeng Z and Ming T: Hypoxia promotes the proliferation of mouse
liver sinusoidal endothelial cells: miRNA-mRNA expression analysis.
Bioengineered. 12:8666–8678. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Poisson J, Lemoinne S, Boulanger C, Durand
F, Moreau R, Valla D and Rautou PE: Liver sinusoidal endothelial
cells: Physiology and role in liver diseases. J Hepatol.
66:212–227. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gu J, Fan Y, Liu X, Zhou L, Cheng J, Cai R
and Xue S: SENP1 protects against myocardial ischaemia/reperfusion
injury via a HIF1α-dependent pathway. Cardiovasc Res. 104:83–92.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pibiri M, Leoni VP and Atzori L: Heme
oxygenase-1 inhibitor tin-protoporphyrin improves liver
regeneration after partial hepatectomy. Life Sci. 204:9–14. 2018.
View Article : Google Scholar : PubMed/NCBI
|