Introduction
Adrenal lymphangiomas are rare and non-functioning
benign tumors, which are usually asymptomatic. Laboratory findings
are nonspecific. As imaging techniques have improved, Adrenal
lymphangiomas usually appear as incidental findings at abdominal
ultrasonography and computed tomography scan examinations. The most
effective treatment option is surgical removal of the tumor.
Herein, we report a case of an adrenal lymphangioma that was
removed by retroperitoneal laparoscopy.
Case report
A 45-year-old female was referred to the urological
ward of The First Affiliated Hospital, College of Medicine,
Zhejiang University, China, for an adrenal mass that had been
detected incidentally by ultrasound examination one month earlier.
The physical examination results were normal. A hormonal
examination revealed that the function of the left adrenal gland
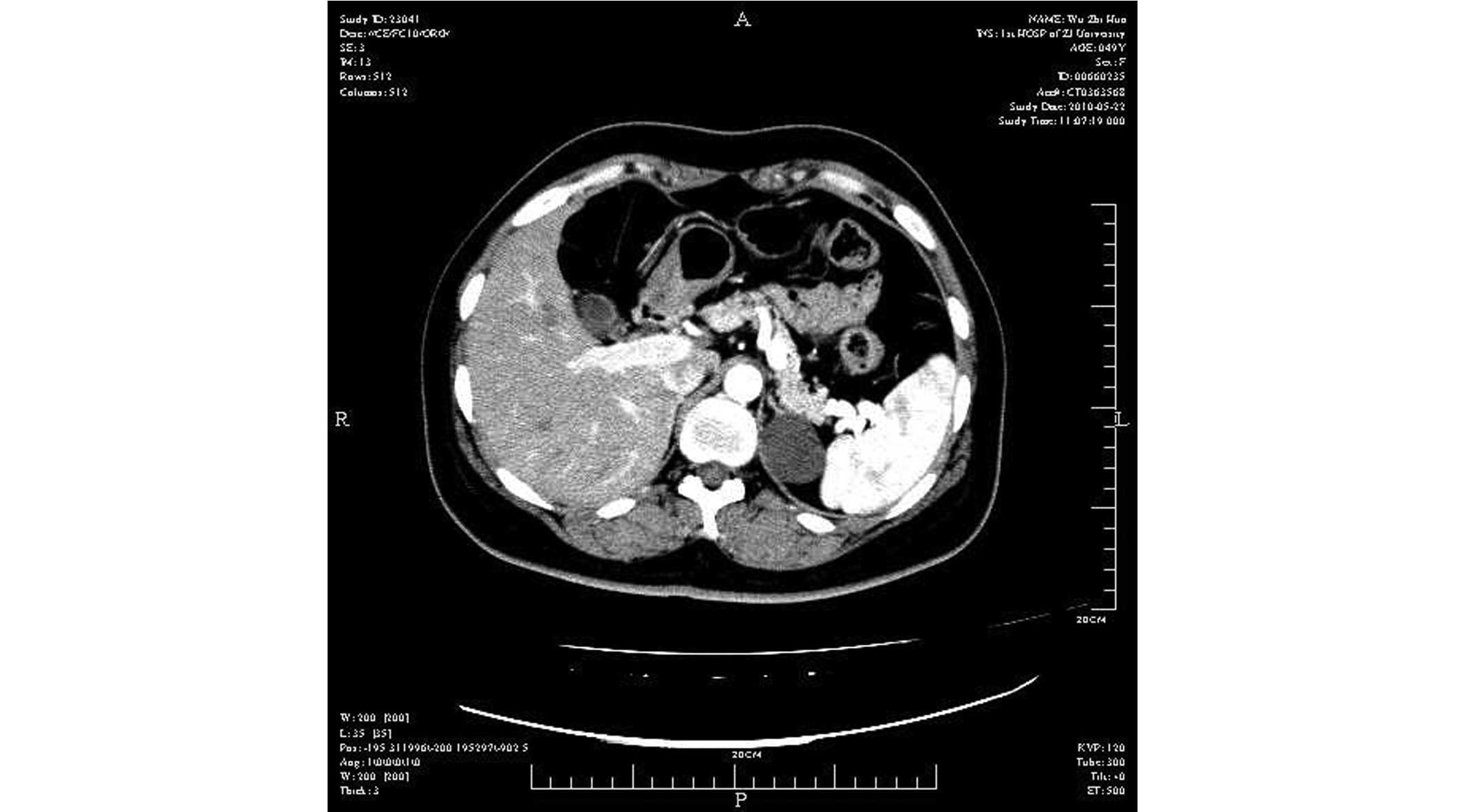
was also normal. An abdominal ultrasonography (US) scan revealed a
3.0-cm anechoic cystic mass of the left adrenal gland. A computed
tomography (CT) scan revealed a 3.0×2.7-cm hypodense non-enhancing
lesion of the left adrenal gland, which was suspected to be an
adrenal cyst (Fig. 1).
Retroperitoneoscopic removal of the tumor was
successfully performed via a posterior approach. For the first
trocar insertion, a 2.0-cm transverse incision was made at the
midaxillary line, approximately 3 finger-breadths cephalad to the
crista iliaca. Two additional supracostal trocars (5 and 10
mm) were subsequently inserted in the anterior and posterior
axillary lines, respectively. These two trocars were then guided by
the index finger into the first port. Thereafter, a
pneumoretroperitoneum was created by maintaining a carbon dioxide
pressure of ∼5 mmHg, and retroperitoneoscopy was performed.
Following confirmation of the location of the tumor, the tumor was
successfully mobilized and removed using an ultrasonically
activated scalpel and clip. The tumor was removed through an
incision and subsequently placed in a specimen bag. The operating
time was 80 min and blood loss was ∼30 ml. A drainage tube was put
in place for 2 days. No complications were observed either intra-
or postoperatively. No recurrence has been observed in the 6-month
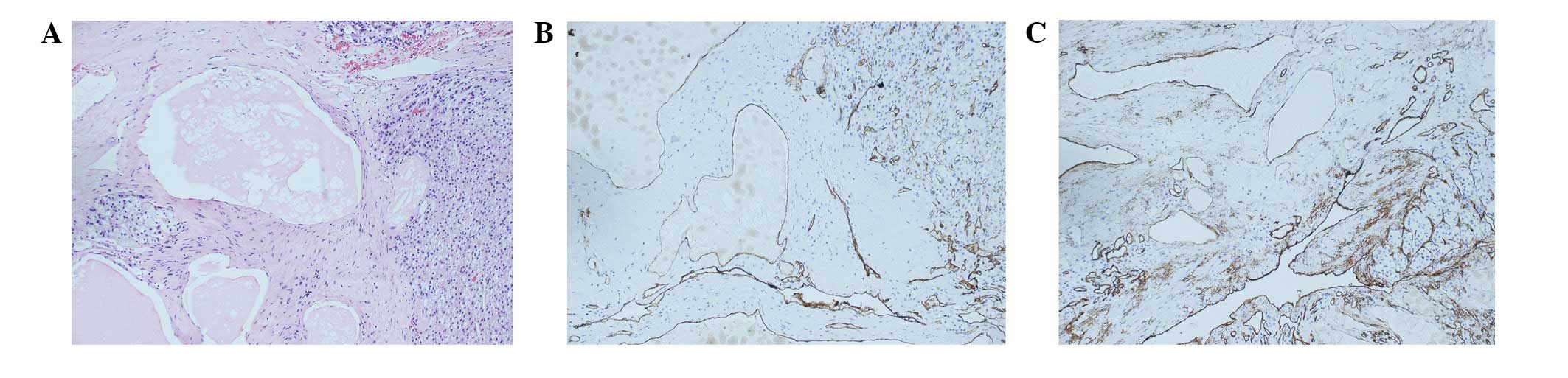
follow-up period. Pathological evaluation revealed a cystic
lymphangioma in the left adrenal gland (Fig. 2).
Discussion
Lymphangiomas are benign malformations of lymphatic
vessels that originate from an abnormal embryologic development of
the lymphatic system. There are four histological subtypes of
lymphangiomas: cystic, capillary, cavernous and vasculolymphatic
malformation (1). Combinations of
such types may be seen in the same lesion. The dominating
histological feature of lymphangiomas is endothelial-lined
lymphatic channels, which are separated by connective tissue
(2).
Lymphangiomas of the adrenal gland are rare. They
are characterized by multiloculated cystic- and endothelial-lined
cavities (3). The endothelial
lining reacts with Factor VIII-related antigen, CD31 and CD34
(4). Adrenal lymphangiomas are
typically asymptomatic; they are discovered as incidental findings
in abdominal US and CT scan examinations, due to improved imaging
techniques. Surgical removal of adrenal lymphangiomas is the most
effective treatment. Retroperitoneoscopic removal of the tumor is
regarded as a safe, effective and minimally invasive approach. This
treatment option offers several advantages, such as an excellent
visualization of the adrenal vessels allowing early ligation, and
avoiding opening of the peritoneal cavity and manipulation of the
intra-abdominal organs. Although the work space is limited for this
procedure, retroperitoneal laparoscopy is usually performed without
any difficulties. Therefore, it may become the standard treatment
procedure for adrenal lymphangioma.
Acknowledgements
This study was supported by grant from
the Zhejiang Provincial Educational Science Foundation of China
(Grant Y201226273) and the National Key Clinical Specialty
Construction Project of China.
References
|
1.
|
Fauquenot-Nollen AM, Plaisier ML, Tjon A
and Tham RT: Combined thoracic and abdominal lymphangioma in an
adult. JBR-BTR. 85:130–131. 2002.PubMed/NCBI
|
|
2.
|
Ates LE, Kapran Y, Erbil Y, Barbaros U and
Dizdaroglu F: Cystic lymphangioma of the right adrenal gland.
Pathol Oncol Res. 11:242–244. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Satou T, Uesugi T, Nakai Y, Hayashi Y,
Imano M and Hashimoto S: Case of adrenal lymphangioma with atypical
lymphocytes in aspirate cytology. Diagn Cytopathol. 29:87–90. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Torres C, Ro JY, Batt MA, Park YW, Ordonez
NG and Ayala AG: Vascular adrenal cysts: a clinicopathologic and
immunohistochemical study of six cases and review of the
literature. Mod Pathol. 10:530–536. 1997.PubMed/NCBI
|