Introduction
Despite its declining incidence, gastric cancer
remains the second most common cause of cancer-related mortality in
Asia and worldwide (1,2). Surgery remains the mainstay of any
curative treatment. However, even following radical surgery, the
majority of gastric cancer patients develop local or distant
recurrence (3). Several
meta-analyses of postoperative adjuvant trials have demonstrated a
significant benefit for chemotherapy-treated patients (4). However, certain patients have
undergone expensive and potentially harmful therapy without gaining
any benefit. Thus, the identification of molecular markers in
resected tumor tissues that are able to predict outcomes is
essential for the future development of adjuvant chemotherapy for
gastric cancer patients.
Cisplatin is widely used and has been demonstrated
to be effective in the palliative treatment of gastric cancer, and
different combinations have been investigated in the adjuvant
setting (5,6). Oxaliplatin (cis-[oxalate (trans-l-1,
2-diaminocyclohexane) platinum (II)]), a third-generation platinum
compound, has been observed to be more effective than cisplatin
(7), and has a more favorable
toxicity profile than cisplatin (8). Thus the oxaliplatin plus
5-fluorouracil (5-FU) modulated with leucovorin (LV) (FOLFOX
regimen) has been widely used as the first-line treatment in
advanced gastric cancer (9–13). However, resistance to oxaliplatin
and cisplatin remains a major obstacle to further increasing the
response rate. Additionally, the involvement of the FOLFOX regimen
in combination with surgery to increase local control or prolong
survival also requires further investigation in resected gastric
cancer.
DNA repair capacity is considered to be both a
barrier to carcinogenesis and a crucial molecular pathway
implicated in resistance to platinum-based chemotherapy (14). The cytotoxic effect of anticancer
platinum drugs is principally attributable to the formation of
platinum-DNA adducts (15).
Nucleotide excision repair (NER) is the primary DNA repair
mechanism that removes platinum-DNA adducts from genomic DNA.
Excision repair cross-complementing 1 (ERCC1) is a critical gene in
the NER pathway (16). ERCC1 is
highly conserved during evolution and is constitutively expressed
in all tissues at relatively high levels. A functional ERCC1 is
essential for survival; knockdown of the ERCC1 gene in mice was
observed to lead to an accelerated-aging phenotype, with brain
damage, liver failure and death occurring shortly after weaning
(17). A growing body of evidence
has demonstrated that the ERCC1 gene acts as both a predictive and
a prognostic marker (18,19). It has been demonstrated in several
clinical studies that ERCC1 messenger RNA expression in various
types of cancer, including ovarian, colorectal, gastric and
esophageal cancer, as well as non-small cell lung cancer (NSCLC),
is correlated with clinical resistance to platinum agents (20–23).
However, a limited number of gastric cancer studies have focused on
the effect of ERCC1 expression on the outcome of FOLFOX adjuvant
chemotherapy.
The aim of this study was to evaluate the effect of
ERCC1 expression levels on the chemosensitivity of platinum agents
in gastric cancer cell lines, and to evaluate whether ERCC1
expression levels are correlated with survival in gastric cancer
patients treated with surgery followed by oxaliplatin-based
adjuvant chemotherapy.
Materials and methods
Cell lines and cultures
The human gastric cancer cell lines, including AGS,
NCI-N87, BGC-823, HGC and MKN45, were obtained from the Shanghai
Institute of Cell Biology (Shanghai, China). All cell lines were
propagated in Roswell Park Memorial Institute (RPMI)-1640 medium
(Gibco-BRL; Carlsbad, CA, USA), supplemented with 10% bovine serum,
penicillin (100 U/ml)-streptomycin (100 mg/ml), pyruvate, glutamine
and insulin at 37°C in a water-saturated atmosphere with 5%
CO2.
Drugs
Oxaliplatin (Oxa) and cisplatin (DDP) were supplied
by the Jiangsu Hengrui Medicine Company (Jiangsu, China). The
dilutions of all reagents were freshly prepared before each
experiment. CellTiter 96 Aqueous One Solution Cell Proliferation
Assay kit was purchased from Promega Corporation (Madison, WI,
USA). Annexin-V-fluorescein isothiocyanate (FITC) Apoptosis
Detection kit was purchased from Invitrogen Life Technologies
(Carlsbad, CA, USA).
siRNA-mediated ERCC1 silencing
Transient knockdown of ERCC1 was achieved by
transient transfection of 10 ng/μl ERCC1 siRNA (OriGene
Technologies, Inc.; Rockville, MD, USA). AGS and MKN cells were
transfected with siRNA duplexes (10 ng/μl) using
Lipofectamine 2000 (Invitrogen Life Technologies) for 48 h,
according to the manufacturer’s instructions, and then treated with
platinum agents for 48 h. An empty pGFP-V-RS vector and HuSH 29-mer
non-effective scrambled pGFP-V-RS were used in control experiments,
and were purchased from OriGene Technologies, Inc.
Cell viability assay
Cytotoxicity was determined using the CellTiter 96
Aqueous One Solution Cell Proliferation Assay kit. Briefly, tumor
cells growing in the log-phase were trypsinized and seeded at
2×103 cells/well into 96-well plates and allowed to
attach overnight. The medium in each well was replaced with fresh
medium or medium with various concentrations of drugs in at least
six replicate wells and left to make contact for 48 h. One-fifth of
the volume of CellTiter 96 Aqueous One Solution was added to each
well and incubated for an additional 3 h. Absorbance was determined
with a microplate reader (Bio-Rad; Hercules, CA, USA) at 490 nm.
The blank control wells were used for zeroing the absorbance. Each
experiment was allocated 10 wells containing drug-free medium as a
control. The inhibition rate (I%) was calculated using the
background-corrected absorbance by the following equation:
I%=(Auntreated control well - Aexperimental
well) / Auntreated control well ×100. The
IC50 value was defined as the concentration required for
50% inhibition of cell growth.
Apoptosis assay
The quantification of apoptotic cells was performed
using an Annexin-V-FITC Apoptosis Detection kit (Invitrogen Life
Technologies) according to the manufacturer’s instructions.
Briefly, cells were plated in a 60-mm Petri dish and allowed to
grow to 75–80% confluence. Cells were exposed to ERCC1 siRNA and
anticancer drugs were added singly for 48 h or cells were
pretreated with ERCC1 siRNA for 48 h. Subsequently, the medium was
replaced with fresh medium with anticancer drugs for another 48 h,
and these were compared with control cells that had not been
treated with drugs. The cells were then collected and resuspended
in 500 μl binding buffer, and 5 μl Annexin-V-FITC and
5 μl propidium iodide (PI) were added. Analyses were
performed with a flow cytometer (FACSCalibur; Becton Dickinson;
Franklin Lakes, NJ, USA).
Quantitative polymerase chain reaction
(qPCR) assessment of ERCC1 expression
Fresh specimens were collected, grossly viewed and
dissected from the primary malignant lesion by a pathologist
immediately after surgical resection, and frozen within 20 min in
liquid nitrogen. Cells were harvested with trypsin, washed with PBS
and collected by centrifugation at 1,000 rpm for 5 min. Total RNA
was extracted using SV Total RNA isolation system (Promega
Corporation) according to the manufacturer’s instructions. The
purity and quality of the mRNA were measured by a Bio-visible
spectrophotometer (Eppendorf AG; Hamburg, Germany), while 1%
agarose gel electrophoresis was used to assess the integrity of the
obtained RNA. cDNA with a total volume of 20 μl was
synthesized using the reverse transcription system containing
reverse transcriptase (Promega Corporation) according to the
manufacturer’s instructions. Real-time qPCR of the target gene and
β-actin as internal control was carried out with iCycler iQ
Multicolor Real-time PCR Detection System (Bio-Rad). The 20
μl PCR reaction mixture contained 1X primers and probe
mixture [assay IDs: Hs00157415_m1 (ERCC1) and Hs99999903_m1
(β-actin); Applied Biosystems, Foster City, CA, USA] and 1X
Absolute QPCR mix (Abgene UK, Ltd.; Surrey, UK). The PCR conditions
were 50°C for 2 min, 95°C for 15 min, followed by 45 cycles at 95°C
for 15 sec and 60°C for 1 min. Relative gene expression
quantifications were calculated according to the comparative Ct
method using β-actin as an endogenous control and commercial human
total RNA (Clontech Laboratories, Inc.; Mountain View, CA, USA) as
calibrators. Final results were determined by the 2−ΔΔCt
formula, as described previously by Livak and Schmittgen (24). In the siRNA-mediated ERCC1 silencing
study, equal amounts of the qRT-PCR products were also analyzed in
ethidium bromide-stained 1% agarose gel.
Western blot analysis
ERCC1 protein expression in cells was detected by
western blot analysis. Briefly, cells were washed twice with
ice-cold phosphate-buffered saline (PBS). Total protein lysates
were obtained from cells using radio immuno-precipitation assay
(RIPA) cell lysis buffer (Boster, Wuhan, China). Samples were spun
at 20,000 x g at −4°C for 15 min, and the supernatant was stored at
−80°C or immediately quantified using a protein assay (Bio-Rad).
Protein lysates were electrophoresed and equal loading was assessed
by Ponceau Red staining following transfer to nitrocellulose
membranes. The primary antibodies used for blotting were anti-ERCC1
and anti-β-actin (OriGene Technologies, Inc.) as a loading control.
The secondary antibody used was goat anti-mouse-horseradish
peroxidase (HRP) (Santa Cruz Biotechnology, Inc.; Santa Cruz, CA,
USA). Luminescence was revealed by incubation with ECL Western
blotting substrate (Promega Corporation) and signals were detected
using a FluorChem SP imaging system (Alpha Innotech, San Leandro,
CA, USA).
Patients and treatment protocols
Tumor specimens were collected from 75 patients with
stages Ib-IV (M0) who were recruited during the period from
January, 2005 to June, 2007 and underwent surgery at the Department
of Gastroenterological Surgery, Changzhou Tumor Hospital. The
patients comprised 53 males and 22 females, ranging in age from
36–73 years, with a median age of 58 years. None of the patients
had previously received chemotherapy. This study had been approved
by the local ethics committees, and written informed consent was
obtained from all patients. Following surgery, 57 patients received
≥6 cycles of oxaliplatin at 85 mg/m2 plus leucovorin at
20 mg/m2 on the first day of treatment, followed by
5-FU, via a 400 mg/m2 bolus, and a 22 h continuous
infusion of 600 mg/m2 5-FU on Days 1–2 at 2-week
intervals. Twenty-three patients received surgery alone.
Follow-up
Interim history, physical examination, hematological
studies, carcinoembryonic antigen levels and whole-body computed
tomography were conducted every 3 months in the first year and
every 6 months thereafter. Patients underwent upper endoscopy 6
months after surgery and every 12 months thereafter. Recurrences or
metastases of gastric carcinoma were determined by cytology biopsy,
surgery or whole-body computed tomography. The American Joint
Committee on Cancer (AJCC) 7th Edition of Gastric Cancer was used
for the classification of each case. The study was implemented in a
blind fashion; the patient outcome was unknown to investigators
performing the molecular analyses. Relapse-free survival (RFS) was
the time period from study initiation until disease recurrence or
death or the day of the last follow-up visit (whichever of these
occurred first). Overall survival (OS) was the time period from
study initiation until the date of mortality, regardless of the
cause, or until the most recently documented follow-up.
Statistical analysis
Statistical significance was based on a two-sided
significance level of 0.05. All analyses were performed with the
Statistical Package for the Social Sciences (SPSS), version 13.0
(SPSS, Inc.; Chicago, IL, USA). The Spearman’s correlation
coefficient was adopted to analyze the correlation between gene
expression levels and drug sensitivity. Statistical comparisons
were performed using the Student’s t-test. To test for correlations
between gene expression levels and the clinical variables,
dichotomization of the gene expression values as equal/above and
below the median expression value were conducted and tested by the
χ2 test or Fisher’s exact test (two-sided), as
appropriate. Kaplan-Meier survival curves and the log-rank test
were used to analyze univariate distributions for RFS and OS. The
prognostic significance of ERCC1 following adjustment for other
prognostic factors was assessed using a Cox proportional hazards
regression model.
Results
ERCC1 expression level is correlated with
the chemosensitivity of platinum agents in gastric cancer cell
lines
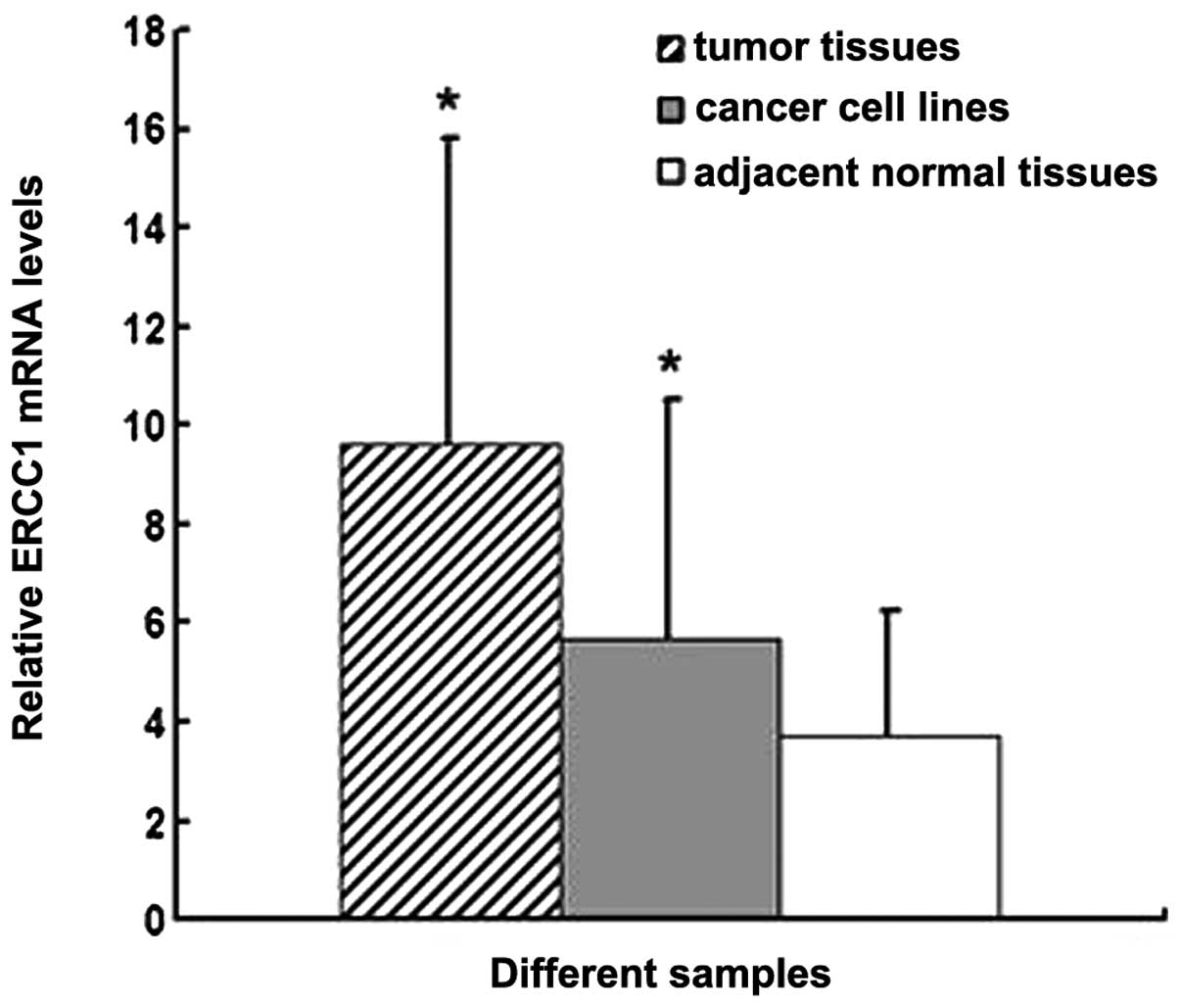
The ERCC1 expression levels were first examined in 7
gastric cancer cell lines, tumor tissues and adjacent normal
tissues by qRT-PCR. ERCC1 mRNA levels in gastric cancer cell lines
and gastric cancer tissues were significantly higher than those in
adjacent normal tissues (P<0.05; Fig. 1). No significant differences were
observed between gastric cancer cell lines and gastric cancer
tissues.
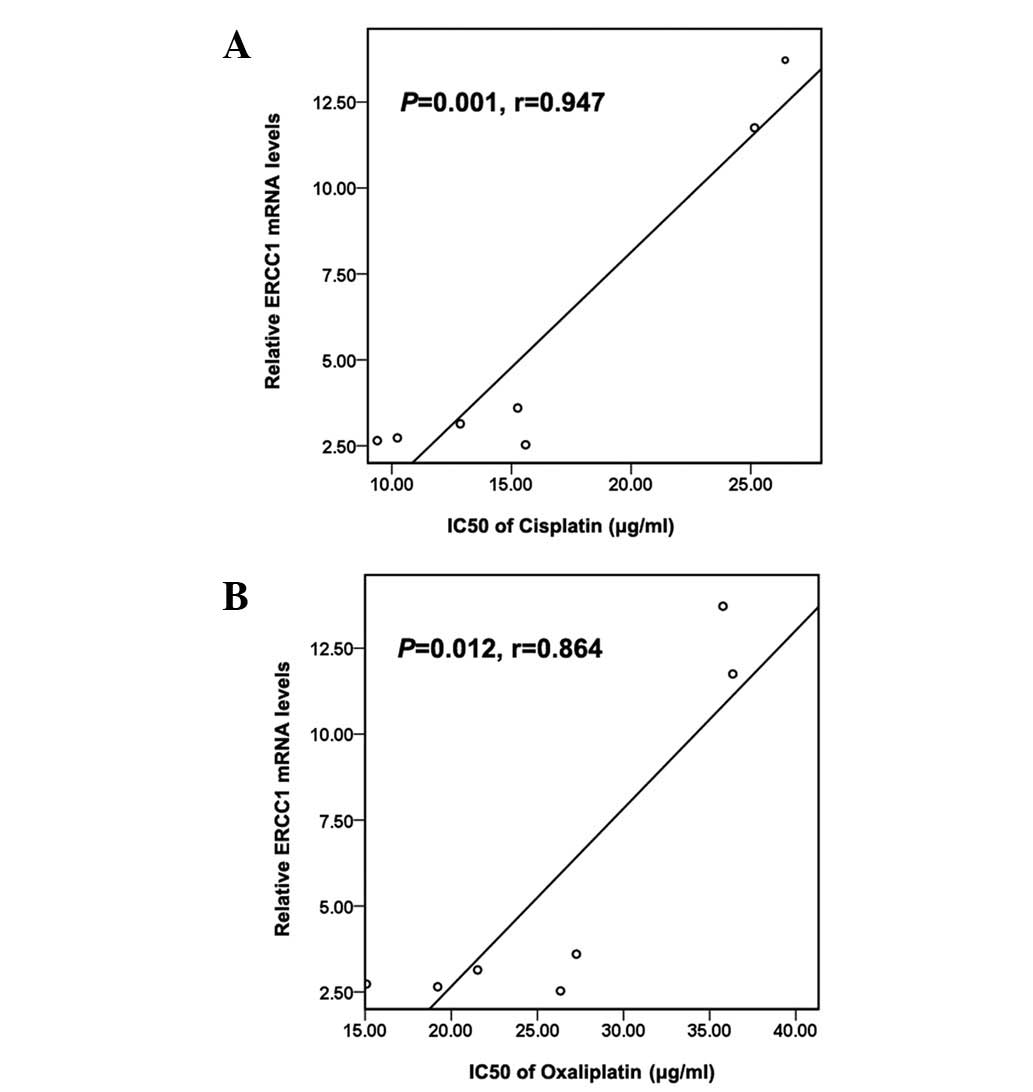
The correlation between ERCC1 mRNA expression levels
and the chemosensitivity of platinum agents in 7 gastric cancer
cell lines was subsequently determined. We found that ERCC1 mRNA
expression levels were positively correlated with the
IC50 value of cisplatin (P=0.001; r=0.947; Fig. 2A) and oxaliplatin (P=0.012; r=0.864;
Fig. 2B), respectively.
Inhibition of ERCC1 by siRNA sensitizes
gastric cancer cell lines to cisplatin and oxaliplatin
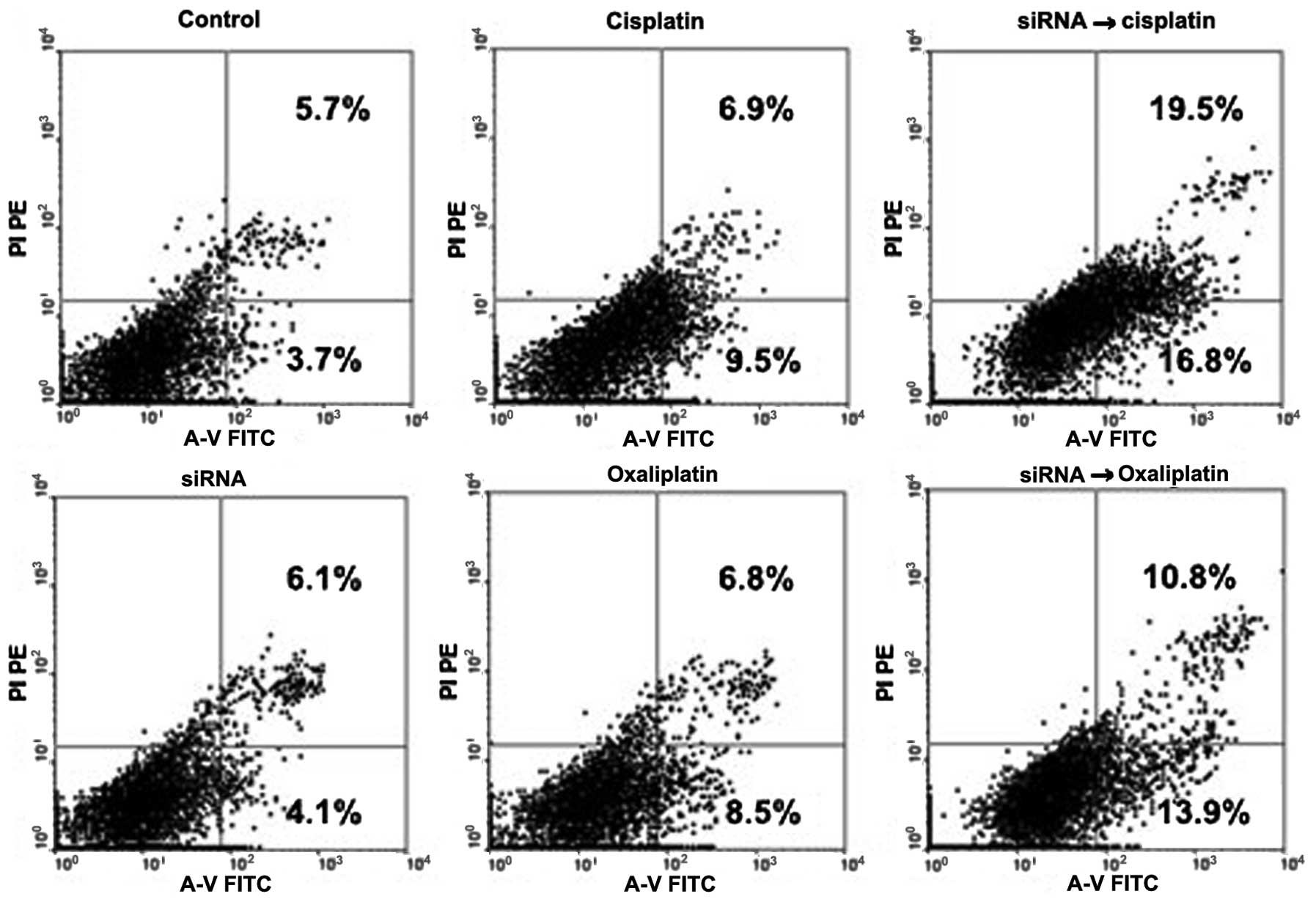
To further examine the functional role of ERCC1 in
gastric cancer cells, the relatively resistant MKN45 cells were
transfected with siRNA duplexes against ERCC1. In MKN45 cell lines,
successful knockdown of ERCC1 expression was confirmed by qRT-PCR
and western blot analysis (Fig. 3).
Downregulation of ERCC1 by siRNA did not result in significant
suppression of cell proliferation following transfection for 48 h,
while siRNA-mediated attenuation of ERCC1 expression led to a
subsequent sensitizing effect to cisplatin and oxaliplatin by an
early apoptosis test (Fig. 4). The
CellTiter 96 Aqueous One Solution Cell Proliferation test
demonstrated that downregulation of ERCC1 by siRNA decreased the
IC50 value of cisplatin from 26.44±2.72 to 2.12±0.31
μg/ml (P<0.001) and that of oxaliplatin from 35.77±3.82
to 7.12±0.72 μg/ml (P=0.003). These results suggest that the
ERCC1 expression level is important for cell viability against
platinum-based drugs, and that the expression of ERCC1 siRNA
effectively increased the sensitivity to these drugs.
Expression levels of ERCC1 mRNA are
correlated with clinicopathological characteristics
The expression of ERCC1 mRNA was evaluable in all 75
patients, and the median value was 7.32 (range 0.50–147.03).
Table I summarizes the
characteristics of the study population. Patients were divided into
two groups centered about the median value; 38 patients with high
ERCC1 levels and 37 with low ERCC1 levels. High ERCC1 expression
was more common in younger patients (60.5% for younger patients vs.
37.8% for elderly patients; P=0.049). No other correlations were
observed between the clinical characteristics and ERCC1 expression
levels (Table I).
 | Table ICorrelations between ERCC1 expression
levels and clinical variables. |
Table I
Correlations between ERCC1 expression
levels and clinical variables.
| Variables | ERCC1 expression
level
| Total | P-value |
|---|
| High (%) | Low (%) |
|---|
| Gender | | | | 0.276 |
| Male | 24 (45.3) | 29 (54.7) | 53 (100) | |
| Female | 13 (59.1) | 9 (40.9) | 22 (100) | |
| Age (years)
(median) | | | | 0.049 |
| ≤58 | 23 (60.5) | 15 (39.5%) | 38 (100) | |
| >58 | 14 (37.8) | 23 (62.2%) | 37 (100) | |
| Tumor
differentiation | | | | 0.537 |
| Well | 15 (57.7) | 11 (42.3) | 26 (100) | |
| Moderate | 17 (43.6) | 22 (56.4) | 39 (100) | |
| Poor or
undifferentiated | 5 (50.0) | 5 (50.0) | 10 (100) | |
| Site of tumor | | | | 0.427 |
| Proximal
stomach | 12 (50.0) | 12 (50.0) | 24 (100) | |
| Stomach body | 10 (62.5) | 6 (37.5) | 16 (100) | |
| Distal
stomach | 15 (42.9) | 20 (57.1) | 35 (100) | |
| Staging | | | | 0.311 |
| I and II | 9 (56.3) | 7 (43.7) | 16 (100) | |
| III | 13 (39.4) | 20 (60.6) | 33 (100) | |
| IV | 15 (57.7) | 11 (42.3) | 26 (100) | |
| Carcinoembryonic
antigen (ng/ml) | | | | 0.296 |
| ≤5 | 21 (44.7) | 26 (55.3) | 47 (100) | |
| >5 | 16 (57.1) | 12 (42.9) | 28 (100) | |
Expression levels of ERCC1 mRNA are
correlated with survival in patients receiving surgery followed by
FOLFOX adjuvant chemotherapy
The median RFS was 12.5 months (range, 2–49 months),
and the median OS time was 22 months (range, 4–49 months). Table II demonstrates that ERCC1 expression
is significantly correlated with both RFS (P= 0.001) and OS
(P=0.001) time, Fig. 5A and B show
the Kaplan-Meier survival curve for patients with intratumoral
ERCC1 levels equal/above and below the median ERCC1 level. Patients
with ERCC1 levels below the median had a significantly longer
median RFS and median OS times compared with patients with ERCC1
levels equal/above the median (median RFS, 18 vs. 7 months; median
OS, 27 vs. 11 months), respectively. Other factors that were
significantly correlated with RFS and OS in the univariate analysis
by the Kaplan-Meier survival curves and the log-rank test included
age, tumor stage and the levels of serum carcinoembryonic antigen
(Table II). Gender, tumor
differentiation and tumor location were not significant prognostic
factors for either RFS and OS. ERCC1 levels, stage and serum
carcinoembryonic antigen remained significant prognostic factors
correlated with RFS and OS in the Cox proportional hazards
regression model multivariate analysis (Table III).
 | Table IIFactors correlated with survival in
patients receiving surgery followed by oxaliplatin-based adjuvant
chemotherapy. |
Table II
Factors correlated with survival in
patients receiving surgery followed by oxaliplatin-based adjuvant
chemotherapy.
| n | M-RFS (months) | P-value | MST (months) | P-value |
|---|
| Gender | | | 0.526 | | 0.408 |
| Male | 37 | 14 | | 24 | |
| Female | 15 | 9 | | 21 | |
| Age (years) | | | 0.017 | | 0.019 |
| ≤58 | 25 | 8 | | 15 | |
| >58 | 27 | 18 | | | |
| Tumor
differentiation | | | 0.652 | | 0.419 |
| Well | 20 | 17 | | 22 | |
| Moderate | 25 | 12 | | 22 | |
|
Undifferentiated | 7 | 8 | | 15 | |
| Tumor location | | | 0.484 | | 0.598 |
| Proximal
stomach | 14 | 10 | | 17 | |
| Stomach body | 10 | 13 | | 21 | |
| Distal
stomach | 28 | 16 | | 24 | |
| Staging | | | <0.001 | | <0.001 |
| I, II and
III | 32 | 18 | | | |
| IV | 20 | 6 | | 11 | |
| ERCC1 level | | | 0.001 | | 0.001 |
| <7.32 | 29 | 18 | | 27 | |
| ≥7.32 | 23 | 7 | | 12 | |
| Carcinoembryonic
antigen (ng/ml) | | | <0.001 | | <0.001 |
| ≤5 | 33 | 18 | | 27 | |
| >5 | 19 | 6 | | 12 | |
 | Table IIIHazard ratios for relapse-free
survival and overall survival in patients receiving adjuvant
chemotherapy. |
Table III
Hazard ratios for relapse-free
survival and overall survival in patients receiving adjuvant
chemotherapy.
| RFS
| OS
|
|---|
| Prognostic
factors | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| ERCC1 level | | | 0.026 | | | 0.031 |
| <7.32 | 1 | | | 1 | | |
| ≥7.32 | 2.16 | 1.09–4.25 | | 2.21 | 1.07–4.55 | |
| Staging | | | 0.002 | | | 0.010 |
| I, II and
III | 1 | | | 1 | | |
| IV | 3.12 | 1.52–6.42 | | 2.81 | 1.29–6.15 | |
| Carcinoembryonic
antigen (ng/ml) | | | 0.012 | | | 0.050 |
| ≤5 | 1 | | | 1 | | |
| >5 | 2.49 | 1.23–5.09 | | 2.16 | 0.99–4.68 | |
Discussion
Platinum-based chemotherapy remains the backbone of
therapy in the management of advanced gastric cancer. Recently,
oxaliplatin, a third platinum analog, has been widely used in
patients with gastric cancer (25).
A small number of studies have demonstrated that the combination of
oxaliplatin and 5-FU modulated with LV obtained an objective
response rate of 38–55% in gastric cancer patients (9–13,26).
However, this implies that ∼50% of patients suffered the toxic
effects of this regimen without obtaining any real benefit.
Therefore, predictive markers are required to identify those
patients likely to benefit from oxaliplatin-based treatment in
gastric cancer.
The cytotoxic effects of cisplatin and oxaliplatin
are principally attributable to the formation of bulky platinum-DNA
adducts (7,27), and these adducts are recognized and
repaired by the nucleotide excision repair (NER) pathway. The ERCC1
protein is major component of the NER complex, acting as the
rate-limiting enzyme in the NER pathway, while high expression of
ERCC1 has been demonstrated to be correlated with poor responses to
chemotherapy in various tumor types (19,28–33).
In our study, we found the ERCC1 expression levels
were inversely associated with the chemosensitivity of platinum
agents in 7 gastric cancer cell lines, and the inhibition of ERCC1
expression by siRNA sensitized the effects of cisplatin and
oxaliplatin in the relatively resistant MKN45 cells. These results
were partially consistent with those of other studies (28,34,35).
The mechanisms whereby ERCC1 participates in platinum resistance in
cancer cells has been demonstrated to be correlated with increased
removal of the platinum-DNA adducts and interstrand cross-links
(36–38).
Several studies have investigated the influence of
ERCC1 in resistance to platinum compound in gastric cancer
patients, and the majority of which revealed that patients with low
levels of ERCC1 protein or mRNA expression were associated with
favorable clinical outcomes of platinum based anti-cancer
chemotherapy (32,39,40).
This suggests that ERCC1 is a predictive marker for clinical
resistance to platinum compounds. Our results demonstrated that
patients with low ERCC1 levels had longer RFS and OS times than
those with high ERCC1 levels, and the multivariate analysis
suggested that ERCC1 expression is an independent predictive marker
associated with RFS and OS, which is consistent with the studies
mentioned previously. By contrast, other studies have demonstrated
that low ERCC1 expression was correlated with poor survival
(41) or exhibited no correlation
with survival (42). Conflicting
results between different studies may be related to biological
variations of the analyzed tumors, or to variations with respect to
the chemotherapeutic protocol or to the different techniques for
testing ERCC1 expression.
We also investigated the correlation between ERCC1
expression levels and clinicopathological characteristics. A
significant correlation was only observed between ERCC1 expression
levels and age (P=0.049), and high ERCC1 expression was more common
in younger patients (60.5% for younger patients vs. 37.8% for
elderly patients), which may explain why younger patients had
poorer RFS and OS times than elderly patients, following
oxaliplatin-based adjuvant chemotherapy (median RFS, 8 vs. 18
months, P=0.017; median OS, 15 months vs. undefined, P=0.019,
respectively; Table II).
One limitation of the present study is the
relatively small sample size. Moreover, the majority of patients
who received surgery alone belonged to stages II and III, but were
not willing to receive the adjuvant chemotherapy or radiotherapy.
Due to the imbalance in the distribution of clinical stage and the
inadequate sample size, we did not compare survival times between
patients receiving adjuvant chemotherapy and those treated with
surgery alone.
In conclusion, the present results support the
theories that ERCC1 may participate in platinum resistance in
gastric cancer cells, and that high ERCC1 expression may be a poor
predictor of efficient oxaliplatin-based adjuvant chemotherapy. To
further confirm the prognostic value of tumor ERCC1 expression in
gastric cancer, a multi-center prospective study with a large
sample size is required in our future investigations.
Acknowledgements
This study was partly supported by the
Science and Technology Planning Project of Changzhou, Jiangsu
Province (CS20092025), the Research of Health Department in Jiangsu
Province (Z201221), the Science and Technology Planning Project of
Changzhou Health Bureau, Jiangsu Province (QN201106 and ZD201203),
the 333 Talents Training Project of Jiangsu Province, the Key
Medical Innovation Talents Training Project of Changzhou, Jiangsu
Province, and the Project of Jiangsu Province Sanitation Innovation
Team.
References
|
1
|
Leung WK, Wu MS, Kakugawa Y, et al:
Screening for gastric cancer in Asia: current evidence and
practice. Lancet Oncol. 9:279–287. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kamangar F, Dores GM and Anderson WF:
Patterns of cancer incidence, mortality, and prevalence across five
continents: defining priorities to reduce cancer disparities in
different geographic regions of the world. J Clin Oncol.
24:2137–2150. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Macdonald JS: Treatment of localized
gastric cancer. Semin Oncol. 31:566–573. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Carrato A, Gallego-Plazas J and
Guillen-Ponce C: Adjuvant therapy of resected gastric cancer is
necessary. Semin Oncol. 32:S105–S108. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chipponi J, Huguier M, Pezet D, et al:
Randomized trial of adjuvant chemotherapy after curative resection
for gastric cancer. Am J Surg. 187:440–445. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Topuz E, Basaran M, Saip P, et al:
Adjuvant intraperitoneal chemotherapy with cisplatinum,
mitoxantrone, 5-fluorouracil, and calcium folinate in patients with
gastric cancer: a phase II study. Am J Clin Oncol. 25:619–624.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mamenta EL, Poma EE, Kaufmann WK,
Delmastro DA, Grady HL and Chaney SG: Enhanced replicative bypass
of platinum-DNA adducts in cisplatin-resistant human ovarian
carcinoma cell lines. Cancer Res. 54:3500–3505. 1994.PubMed/NCBI
|
|
8
|
Extra JM, Espie M, Calvo F, Ferme C,
Mignot L and Marty M: Phase I study of oxaliplatin in patients with
advanced cancer. Cancer Chemother Pharmacol. 25:299–303. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Louvet C, André T, Tigaud JM, et al: Phase
II study of oxaliplatin, fluorouracil, and folinic acid in locally
advanced or metastatic gastric cancer patients. J Clin Oncol.
20:4543–4548. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
De Vita F, Orditura M, Matano E, et al: A
phase II study of biweekly oxaliplatin plus infusional
5-fluorouracil and folinic acid (FOLFOX-4) as first-line treatment
of advanced gastric cancer patients. Br J Cancer. 92:1644–1649.
2005.PubMed/NCBI
|
|
11
|
Al-Batran SE, Atmaca A, Hegewisch-Becker
S, et al: Phase II trial of biweekly infusional fluorouracil,
folinic acid, and oxaliplatin in patients with advanced gastric
cancer. J Clin Oncol. 22:658–663. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lordick F, Lorenzen S, Stollfuss J, et al:
Phase II study of weekly oxaliplatin plus infusional fluorouracil
and folinic acid (FUFOX regimen) as first-line treatment in
metastatic gastric cancer. Br J Cancer. 93:190–194. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cavanna L, Artioli F, Codignola C, et al:
Oxaliplatin in combination with 5-fluorouracil (5-FU) and
leucovorin (LV) in patients with metastatic gastric cancer (MGC).
Am J Clin Oncol. 29:371–375. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wei Q, Frazier ML and Levin B: DNA repair:
a double-edged sword. J Natl Cancer Inst. 92:440–441. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Woynarowski JM, Faivre S, Herzig MC, et
al: Oxaliplatin-induced damage of cellular DNA. Mol Pharmacol.
58:920–927. 2000.PubMed/NCBI
|
|
16
|
Reed E: ERCC1 and clinical resistance to
platinum-based therapy. Clin Cancer Res. 11:6100–6102. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nuñez F, Chipchase MD, Clarke AR and
Melton DW: Nucleotide excision repair gene (ERCC1) deficiency
causes G(2) arrest in hepatocytes and a reduction in liver
binucleation: the role of p53 and p21. FASEB J. 14:1073–1082.
2000.PubMed/NCBI
|
|
18
|
Cobo M, Isla D, Massuti B, et al:
Customizing cisplatin based on quantitative excision repair
cross-complementing 1 mRNA expression: a phase III trial in
non-small-cell lung cancer. J Clin Oncol. 25:2747–2754. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Olaussen KA, Dunant A, Fouret P, et al:
DNA repair by ERCC1 in non-small-cell lung cancer and
cisplatin-based adjuvant chemotherapy. N Engl J Med. 355:983–991.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Weberpals J, Garbuio K, O’Brien A, et al:
The DNA repair proteins BRCA1 and ERCC1 as predictive markers in
sporadic ovarian cancer. Int J Cancer. 124:806–815. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Denlinger CS and Cohen SJ: Progress in the
development of prognostic and predictive markers for
gastrointestinal malignancies. Curr Treat Options Oncol. 8:339–351.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Iqbal S, Stoehlmacher J and Lenz HJ:
Tailored chemotherapy for colorectal cancer: a new approach to
therapy. Cancer Invest. 22:762–773. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Höfler H, Langer R, Ott K and Keller G:
Prediction of response to neoadjuvant chemotherapy in carcinomas of
the upper gastrointestinal tract. Adv Exp Med Biol. 587:115–120.
2006.
|
|
24
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Boku N: Perspectives for personalization
in chemotherapy of advanced gastric cancer. Discov Med. 9:84–89.
2010.PubMed/NCBI
|
|
26
|
Mauer AM, Kraut EH, Krauss SA, et al:
Phase II trial of oxaliplatin, leucovorin and fluorouracil in
patients with advanced carcinoma of the esophagus. Ann Oncol.
16:1320–1325. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Suo Z, Lippard SJ and Johnson KA: Single
d(GpG)/cis-diammineplatinum(II) adduct-induced inhibition of DNA
polymerization. Biochemistry. 38:715–726. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Selvakumaran M, Pisarcik DA, Bao R, Yeung
AT and Hamilton TC: Enhanced cisplatin cytotoxicity by disturbing
the nucleotide excision repair pathway in ovarian cancer cell
lines. Cancer Res. 63:1311–1316. 2003.PubMed/NCBI
|
|
29
|
Sun JM, Ahn MJ, Park MJ, et al: Expression
of excision repair cross-complementation group 1 as predictive
marker for nasopharyngeal cancer treated with concurrent
chemoradiotherapy. Int J Radiat Oncol Biol Phys. 80:655–660. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hwang IG, Ahn MJ, Park BB, et al: ERCC1
expression as a prognostic marker in N2(+) nonsmall-cell lung
cancer patients treated with platinum-based neoadjuvant concurrent
chemoradiotherapy. Cancer. 113:1379–1386. 2008.
|
|
31
|
Jun HJ, Ahn MJ, Kim HS, et al: ERCC1
expression as a predictive marker of squamous cell carcinoma of the
head and neck treated with cisplatin-based concurrent
chemoradiation. Br J Cancer. 99:167–172. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kwon HC, Roh MS, Oh SY, et al: Prognostic
value of expression of ERCC1, thymidylate synthase, and glutathione
S-transferase P1 for 5-fluorouracil/oxaliplatin chemotherapy in
advanced gastric cancer. Ann Oncol. 18:504–509. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kim MK, Cho KJ, Kwon GY, et al: ERCC1
predicting chemoradiation resistance and poor outcome in
oesophageal cancer. Eur J Cancer. 44:54–60. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chang IY, Kim MH, Kim HB, et al: Small
interfering RNA-induced suppression of ERCC1 enhances sensitivity
of human cancer cells to cisplatin. Biochem Biophys Res Commun.
327:225–233. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Song L, Ritchie AM, McNeil EM, Li W and
Melton DW: Identification of DNA repair gene Ercc1 as a novel
target in melanoma. Pigment Cell Melanoma Res. 24:966–971. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sancar A: Excision repair in mammalian
cells. J Biol Chem. 270:15915–15918. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Darcy KM, Tian C and Reed E: A Gynecologic
Oncology Group study of platinum-DNA adducts and excision repair
cross-complementation group 1 expression in optimal, stage III
epithelial ovarian cancer treated with platinum-taxane
chemotherapy. Cancer Res. 67:4474–4481. 2007. View Article : Google Scholar
|
|
38
|
Kudo K, Gavin E, Das S, Amable L, Shevde
LA and Reed E: Inhibition of Gli1 results in altered c-Jun
activation, inhibition of cisplatin-induced upregulation of ERCC1,
XPD and XRCC1, and inhibition of platinum-DNA adduct repair.
Oncogene. 31:4718–4724. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wei J, Zou Z, Qian X, et al: ERCC1 mRNA
levels and survival of advanced gastric cancer patients treated
with a modified FOLFOX regimen. Br J Cancer. 98:1398–1402. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Matsubara J, Nishina T, Yamada Y, et al:
Impacts of excision repair cross-complementing gene 1 (ERCC1),
dihydropyrimidine dehydrogenase, and epidermal growth factor
receptor on the outcomes of patients with advanced gastric cancer.
Br J Cancer. 98:832–839. 2008. View Article : Google Scholar
|
|
41
|
Kim JS, Kim MA, Kim TM, et al: Biomarker
analysis in stage III–IV (M0) gastric cancer patients who received
curative surgery followed by adjuvant 5-fluorouracil and cisplatin
chemotherapy: epidermal growth factor receptor (EGFR) associated
with favourable survival. Br J Cancer. 100:732–738. 2009.
|
|
42
|
Napieralski R, Ott K, Kremer M, et al:
Combined GADD45A and thymidine phosphorylase expression levels
predict response and survival of neoadjuvant-treated gastric cancer
patients. Clin Cancer Res. 11:3025–3031. 2005. View Article : Google Scholar
|