Introduction
Non-Hodgkin lymphoma (NHL) arising from the soft
tissue of the extremities is rare (1), and its clinical manifestation and
defects observed on magnetic resonance imaging and computed
tomography are characteristic features. In this study, we describe
a 68-year-old female with primary extra-nodal NHL of the right
thigh, which was amputated. The diagnosis was formally established
by pathology. The study shows that tumor tissue immunohistochemical
features are the most important factors in the histological
diagnosis of NHL.
Case report
A 68-year-old female presented to the Department of
Orthopaedics with a 2-month history of a mass in the posterior part
of the right thigh and a 1-month history of movement disorder of
the right lower leg, with numbness and a painful sensation in the
area. The patient was apparently well prior to the illness and her
past medical history was uneventful. Physical examination revealed
a well-nourished older woman with no abnormal findings on systemic
examination. No palpable cervical, axillary or inguinal
lymphadenopathy was observed. The patient was found to have a huge
undefined, thick, swollen and fleshy mass of approximately 22×15×10
cm occupying the majority of the posterior part of the right thigh,
with a similar mass of approximately 10×8×6 cm at the proximal
posterior area of the right leg, and movement disorder of the right
lower leg. Fine needle aspiration cytology (FNAC) of the tumor
demonstrated neoplastic small, round cells, which were considered
to indicate a mesenchymal tissue tumor.
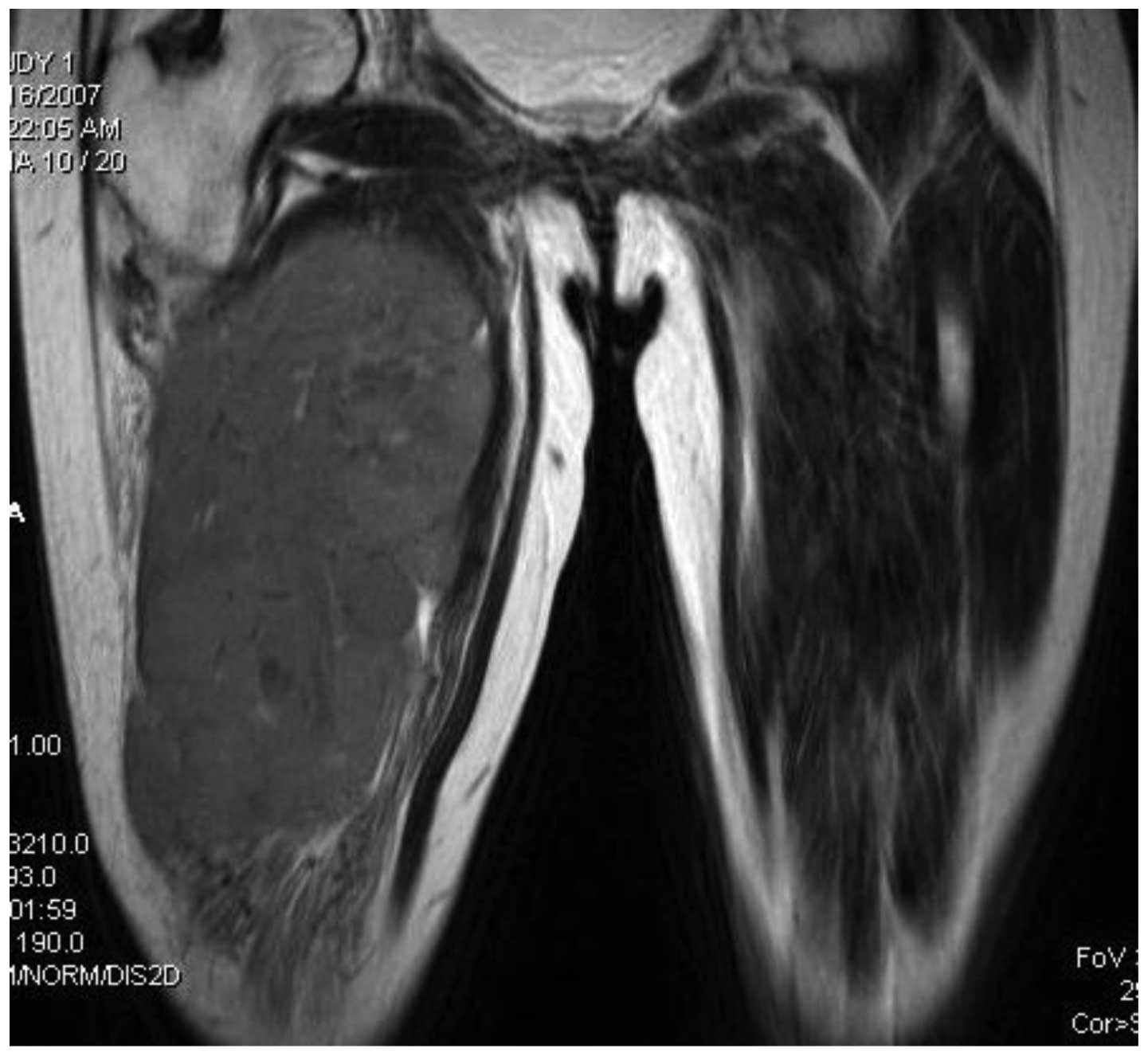
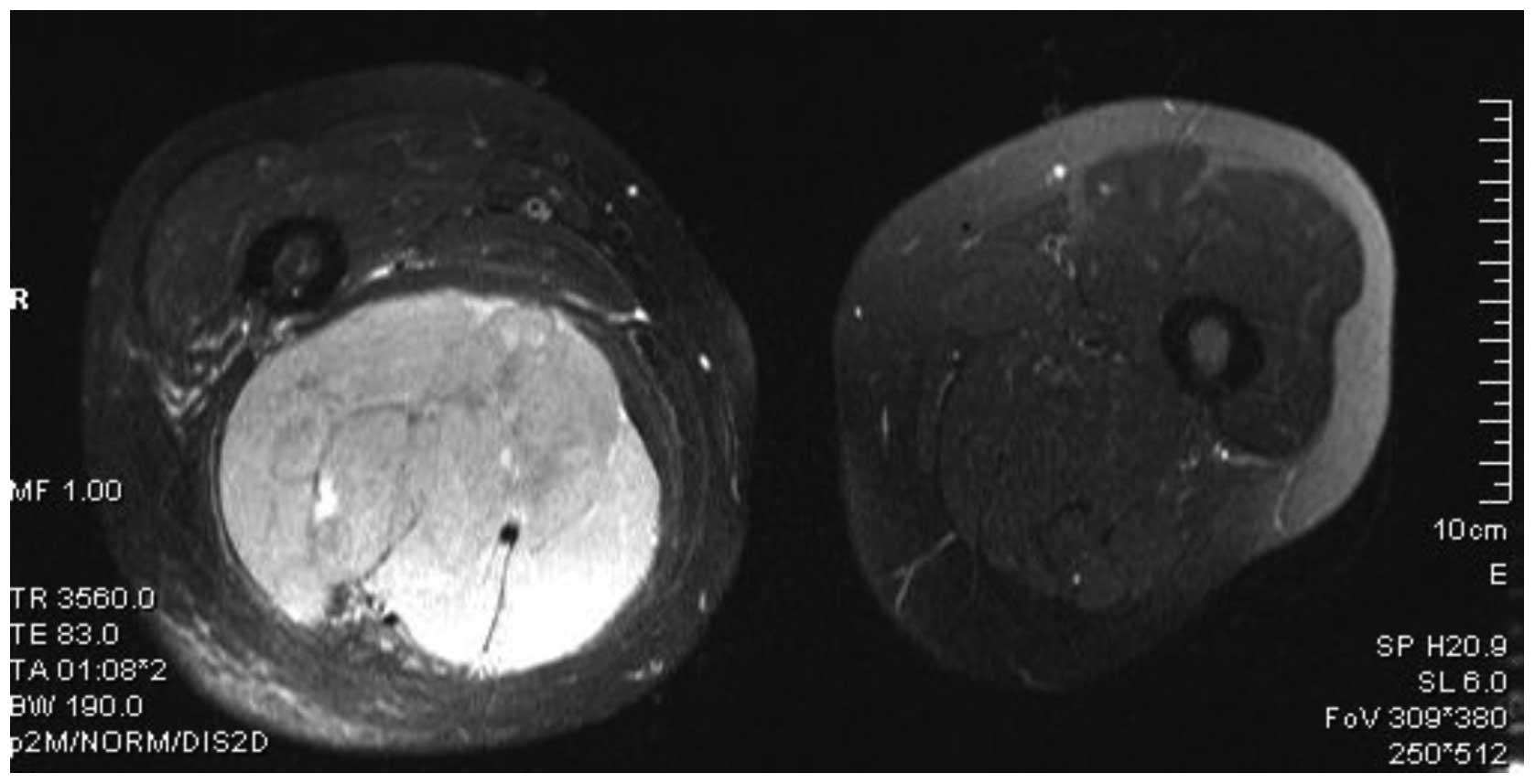
Magnetic resonance (MR) imaging revealed an
approximate circle-shaped mass measuring 21×12×9.5 cm at the
posterior aspect of the right thigh (Fig. 1). The lesion showed lower signal
intensity on T1-weighted images and uneven higher signal intensity
on T2-weighted images. Compression and aversion of the muscles and
blood vessels in the peripheral region of the lesion were also
noted. Muscular fibers in some planes of the images demonstrated
separation and looseness. The sclerotin of adjacent bone appeared
normal in all planes of the images (Fig. 2). Tentative diagnoses included
mesenchymal sarcomas, such as malignant fibrous histiocytoma and
liposarcoma.
Extended resection of the soft connective tissue
tumor of the right thigh was performed. Due to the huge size of the
mass and involvement of the femoral artery, femoral vein and
sciatic nerve, it was difficult to separate and excise the tumor,
therefore the patient was treated with right hip disarticulation
with the permission of the family. Biopsy of the excised mass was
performed and histopathological examination revealed a diagnosis of
NHL of the soft tissue. Immunohistochemical study revealed that the
neoplastic cells were of B cell origin: positive for CD20; negative
for CD3, Myo, Des, PTAH and S-100. Expression of Ki-67 was observed
in 50% of the cells. Therefore, a diagnosis of diffuse large B cell
lymphoma was made.
Following surgery, the patient was referred to the
Department of Hematology for further evaluation. Following a
detailed inquiry, a medical history of night-sweats and loss of
weight was found. Hematological and biochemical work-up revealed
the following results: 106 g/l of hemoglobin (Hb),
209×109/l of platelets, a white blood cell count of
8.5×109/l, 24.8 g/l of albumin, normal levels of lactate
dehydrogenase (LDH) and β2 microglobulin, and normal renal and
liver function. Bone marrow smears displayed reactive
plasmacytosis. The chest X-ray and abdominal ultrasonogram were
normal. The patient refused chemotherapy. Approximately 23 days
later, a rapidly growing mass in the right gluteal region was
observed, and clinical examination revealed a diffuse lump in the
left gluteal area. The subsequent non-contrast computed tomography
(CT) scan of the right hip region revealed a diffuse, hypodense
soft tissue mass with a diameter of 10 cm in the right gluteal
area. Involvement of the right pelvis was found (Fig. 3). The disease was progressive and 50
days later, contrast-enhanced CT of the right gluteal area showed
that there was a huge soft tissue mass with irregular contours in
the right hip area, which extended to the cavity of the pelvis. On
some planes of the image, there was no clear boundary between the
mass and uterus. Sclerotin of the right ala of the ilium, pubis,
femoral head and acetabulum was destroyed. The patient was
subsequently staged as IVB (Ann Arbor staging), and received a
cycle of CHOP (cyclophosphamide, adriamycin, vincristine and
prednisolone) chemotherapy. A transient clinical improvement was
achieved and the patient’s symptoms improved. However, she could
not be given further therapy, and her condition deteriorated
rapidly. The patient succumbed to the disease 6 months later.
Discussion
Malignant lymphoma may present in any region of the
body. The condition is referred to as primary extranodal NHL when
the extranodal site is the only site involved or when the bulk of
the disease is confined to the extranodal site (2). The most common extranodal sites
include the gastrointestinal tract, Waldeyer’s ring, head and neck,
testes, ovary, central nervous system, thyroid, breast, bone and
skin, in order of decreasing frequency (3–13).
Primary NHL localized in the soft tissue of the extremities is
uncommon. Certain reports suggest that true primary NHL in the soft
tissue of the extremities represents approximately 0.11% of all
malignant lymphomas (1). Meanwhile,
diseases such as lymphoma or pseudolymphoma of the skin, histocytic
variants of malignant fibrohistiocytoma or manifestations of
systemic lymphoma should be ruled out at the time of diagnosis. The
symptoms are nonspecific and may mimic other entities, such as
rhabdomyosarcoma, Ewing’s sarcoma, fibrosarcoma, liposarcoma,
synoviosarcoma and metastatic carcinoma. As a consequence of its
low incidence, a standard treatment for primary soft tissue
non-Hodgkin lymphoma has not been clearly defined. Considering that
the therapy for malignant lymphoma is very different from that for
other soft tissue malignancies, accurate diagnosis should be
established prior to definitive treatment.
Several studies have found MR imaging to be superior
in the evaluation of soft tissue tumors compared with CT (14–16).
There are a few reports describing the MR imaging findings of
lymphoma in the soft tissue of the extremities (1,17): a
large soft tissue mass with equal to slightly low signal intensity
on T1-weighted images and markedly high signal intensity on
conventional T2-weighted images, without osseous involvement, but
with infiltration of skeletal muscle and surrounding soft tissues
was observed. Therefore, Lee et al (17) recommend that, at MR imaging, if a
large soft-tissue mass with normal adjacent bone marrow or a mass
more extensive than the adjacent bone marrow abnormalities that
affects a long segment of an extremity with diffuse muscle
involvement is observed, and there is the presence of subcutaneous
stranding or extension, the differential diagnosis should include
and favor primary soft tissue lymphoma in the absence of a history
of trauma or infection. CT is commonly the imaging method of choice
for the detection and staging of lymphoma (18). CT enables accurate measurement of
both the size and extent of the tumor, and provides information to
determine appropriate therapy and response to treatment.
The diagnosis of lymphoma should be based on the
histological examination. However, there are cases in which biopsy
specimens are too difficult to acquire; therefore, fine-needle
aspiration cytology (FNAC) becomes an acceptable alternative
diagnostic procedure with excellent accuracy (19). The usefulness of FNAC in the
differential diagnosis of soft tissue tumors has been discussed in
detail in other studies (20–23).
Since the architectural features of tumors are an important element
in histological diagnosis, the main limitation of FNAC is that it
does not always yield information about tumor tissue architecture
and occasionally the cytological smears are not adequate for
ancillary studies (24), so
histology is preferable. Therefore, in the guidelines published by
the National Comprehensive Cancer Network (NCCN), FNAC is not
recommended for the diagnosis of NHL. On account of FNAC being a
primary diagnostic tool for all soft tissue tumors, a differential
diagnosis of lymphoma should always be kept in mind for other
small, round-cell malignant tumors. Such cases require biopsy
confirmation and immunophenotyping for further subtyping.
The histological subtype, location and the approach
to therapy appear to have some correlation with the clinical
outcome of soft tissue lymphoma of the extremities (1). Our patient presented to the Department
of Orthopaedics with a bulky tumor at the thigh, with a size larger
than 10 cm. Preoperatively, MR imaging revealed a huge mass with a
lower signal intensity on T1-weighted images and a higher signal
intensity on T2-weighted images. Adjacent muscles and blood vessels
were involved without adjacent osseous destruction. The primary
diagnosis was malignant mesenchymoma according to FNAC, and the
patient’s right thigh was then amputated. Histopathological
examination showed diffuse large B cell NHL, a high-grade
malignancy. Postoperative CT revealed a large soft tissue mass in
the right gluteal area with significant involvement of the cavity
of the pelvis and uterus. The sclerotin of the adjacent bone was
infiltrated. The patient succumbed 6 months after the initial
surgery and diagnosis. Based on these observations, our patient had
a very aggressive lymphoma with high probability for
infiltration.
In conclusion, surgical excision is the main
treatment for most primary soft tissue sarcomas. Nevertheless,
primary extremity lymphomas are rare tumors with potentially high
malignancy and metastatic capacity, exhibiting clinical and
histological difficulty for a correct diagnosis. The presence of an
intense soft tissue mass on MR imaging, particularly in a middle-
or older-aged patient, is highly suggestive of lymphoma.
Considering the sensitivity to chemotherapy and radiotherapy,
amputation of the extremity is not optimal for lymphomas. FNAC is
seldom adequate to establish diagnosis, and biopsy of the mass and
histopathological examination are essential to distinguish lymphoma
from other malignant round-cell tumors. Early recognition and
correct diagnosis will allow the proper treatment protocol to be
initiated.
Acknowledgements
This study was supported in part by
the Institution of Higher Learning Strong and Special Subjects Item
Foundation, Hebei Province, China.
References
|
1.
|
WD TravisPM BanksHM ReimanPrimary
extranodal soft tissue lymphoma of the extremitiesAm J Surg
Pathol11359366198710.1097/00000478-198705000-000043578646
|
|
2.
|
R KomakiJ CoxR HansenW GunnM
GreenbergMalignant lymphoma of the uterus and
cervixCancer5416991704198410.1002/1097-0142(19841015)54:8%3C1699::AID-CNCR2820540836%3E3.0.CO;2-E
|
|
3.
|
R HariprasadL KumarDM BhatlaM KukrejaS
PapaiahPrimary uterine lymphoma: Report of 2 cases and review of
literatureAm J Obstet
Gynecol195308313200610.1016/j.ajog.2006.04.00216813759
|
|
4.
|
ME KolveW FischbachM WilhelmPrimary
gastric non-Hodgkin’s lymphoma: requirements for diagnosis and
stagingRecent Results Cancer Res15663682000
|
|
5.
|
S LaskarP MohindraS GuptaT ShetMA
MuckadenNon-Hodgkin lymphoma of the Waldeyer’s ring:
clinicopathologic and therapeutic issuesLeuk
Lymphoma49226322712008
|
|
6.
|
AD KingKI LeiAT AhujaMRI of neck nodes in
non-Hodgkin’s lymphoma of the head and neckBr J
Radiol771111152004
|
|
7.
|
K SasaiH YamabeK TsutsuiY DodoT IshigakiY
ShibamotoM HiraokaPrimary testicular non-Hodgkin’s lymphoma: a
clinical study and review of the literatureAm J Clin
Oncol2059621997
|
|
8.
|
S RayMG MallickPB PalMK ChoudhuryA
BandopadhyayD GuhaExtranodal non-Hodgkin’s lymphoma presenting as
an ovarian massIndian J Pathol Microbiol515285302008
|
|
9.
|
S Camilleri-BroëtA MartinA MoreauR
AngoninD HéninMF GontierMC RousseletS Caulet-MaugendreP CuillièreT
LefrancqPrimary central nervous system lymphomas in 72
immunocompetent patients: pathologic findings and clinical
correlationsAm J Clin Pathol11060761219989802345
|
|
10.
|
M ColovićS MatićE KryeziuD TominN
ColovićHD AtkinsonOutcomes of primary thyroid non-Hodgkin’s
lymphoma: a series of nine consecutive casesMed
Oncol242032082007
|
|
11.
|
E HinoshitaH TashiroII TakahashiT OnoharaT
NishizakiT MatsusakaK WakasugiT IshikawaK KumeI YamamotoY
HirotaPrimary non-Hodgkin’s lymphoma of the breast: a report of two
casesBreast Cancer53093121998
|
|
12.
|
V PantNA JambhekarB MadurTM ShetM AgarwalA
PuriS GujralM BanavaliB AroraAnaplastic large cell lymphoma (ALCL)
presenting as primary bone and soft tissue sarcoma - a study of 12
casesIndian J Pathol Microbiol50303307200717883051
|
|
13.
|
E TheanderG HenrikssonO LjungbergT MandlR
ManthorpeLT JacobssonLymphoma and other malignancies in primary
Sjögren’s syndrome: a cohort study on cancer incidence and lymphoma
predictorsAnn Rheum Dis657968032006
|
|
14.
|
YC LaiHJ ChiouHT WuYH ChouHK WangPC
ChenUltrasonographic and MR findings of alveolar soft part sarcomaJ
Chin Med Assoc72336339200910.1016/S1726-4901(09)70382-X19541571
|
|
15.
|
MJ KransdorfJS JelinekRP Moser JrImaging
of soft tissue tumorsRadiol Clin North Am3135937219938446754
|
|
16.
|
KL VerstraeteP LangBone and soft tissue
tumors: the role of contrast agents for MR imagingEur J
Radiol34229246200010.1016/S0720-048X(00)00202-310927164
|
|
17.
|
VS LeeS MartinezRE ColemanPrimary muscle
lymphoma: clinical and imaging
findingsRadiology203237244199710.1148/radiology.203.1.91224019122401
|
|
18.
|
EK FishmanJE KuhlmanRJ JonesCT of
lymphoma: spectrum of
diseaseRadiographics11647669199110.1148/radiographics.11.4.18871201887120
|
|
19.
|
D DaskalopoulouAD RapidisN MaounisS
MarkidouFine-needle aspiration cytology in tumors and tumor-like
conditions of the oral and maxillofacial region: diagnostic
reliability and
limitationsCancer81238252199710.1002/(SICI)1097-0142(19970825)81:4%3C238::AID-CNCR6%3E3.0.CO;2-L
|
|
20.
|
P DeyMK MallikSK GuptaRK VasishtaRole of
fine needle aspiration cytology in the diagnosis of soft tissue
tumours and tumour-like
lesionsCytopathology153237200410.1046/j.0956-5507.2003.00102.x14748789
|
|
21.
|
MS AminM LuqmanS JamalN MamoonM AnwarFine
needle aspiration biopsy of soft tissue tumoursJ Coll Physicians
Surg Pak13625628200314700487
|
|
22.
|
KW BennertFW Abdul-KarimFine needle
aspiration cytology vs. needle core biopsy of soft tissue tumors. A
comparisonActa Cytol3838138419948191828
|
|
23.
|
S MathurR DawarK VermaDiagnosis and
grading of non-Hodgkin’s lymphomas on fine needle aspiration
cytologyIndian J Pathol Microbiol5046502007
|
|
24.
|
HA DomanskiM AkermanB CarlénJ EngellauP
GustafsonK JonssonF MertensA RydholmCore-needle biopsy performed by
the cytopathologist, a technique to complement fine-needle
aspiration of soft tissue and bone lesionsCancer (Cancer
Cytopathol)105229239200515918176
|